Abstract
Background
Both one-stage [laparoscopic cholecystectomy (LC) plus laparoscopic common bile duct exploration (LCBDE)] and two-stage [endoscopic retrograde cholangiopancreatography (ERCP) followed by sequential LC] approaches are effective treatment for concomitant common bile duct (CBD) stones and gallstone. Although many studies compared one-stage with two-stage surgical approach for cholecysto-choledocholithiasis, there are very few studies compared the two management strategies for acute cholecystitis (AC) associated with CBD stones.
Methods
Between January 2014 and December 2019, patients with concomitant AC and CBD stones proposed to early surgery were retrospectively studied. The patients were scheduled to undergo either the one-stage [LCBDE and LC (LCBDE+LC) were undertaken at the same operation] or two-stage [preoperative ERCP for CBD stone clearance was followed by LC 1–3 days later (pre-ERCP+LC)] procedure. The success rate of complete stone clearance, procedure-related complication, hospital stay, hospitalization charges and later biliary complications were compared between the two groups.
Results
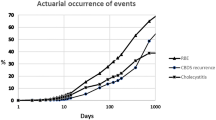
Sixty patients were included in the study, 28 in the one-stage group and 32 in the two-stage group. There was no significant difference in the success rate of complete stone clearance (96.4% vs. 93.8%, P = 1.000), complication rate (10.7% vs. 9.4%, P = 1.000), incidence of pancreatitis (0 vs. 6.3%, P = 0.494) or length of hospital stay (12 ± 5 vs. 11 ± 4 days, P = 0.393) between the two groups.
Conclusion
For patients with concomitant AC and choledocholithiasis proposed to early surgery, both the one-stage (LCBDE+LC) and two-stage (pre-ERCP+LC) approaches were acceptable and broadly comparable in achieving clearance of CBD stones.
Similar content being viewed by others
References
Lammert F, Gurusamy K, Ko CW, Miquel JF, Méndez-Sánchez N, Portincasa P, van Erpecum KJ, van Laarhoven CJ, Wang DQ (2016) Gallstones. Nat Rev Dis Primers 2:16024
Chisholm PR, Patel AH, Law RJ, Schulman AR, Bedi AO, Kwon RS, Wamsteker EJ, Anderson MA, Elta GH, Govani SM, Prabhu A (2019) Preoperative predictors of choledocholithiasis in patients presenting with acute calculous cholecystitis. Gastrointest Endosc 89:977-983.e972
Wong HP, Chiu YL, Shiu BH, Ho LC (2012) Preoperative MRCP to detect choledocholithiasis in acute calculous cholecystitis. J Hepatobiliary Pancreat Sci 19:458–464
Chen H, Jorissen R, Walcott J, Nikfarjam M (2019) Incidence and predictors of common bile duct stones in patients with acute cholecystitis: a systematic literature review and meta-analysis. ANZ J Surg. https://doi.org/10.1111/ans.15565
Tzovaras G, Baloyiannis I, Zachari E, Symeonidis D, Zacharoulis D, Kapsoritakis A, Paroutoglou G, Potamianos S (2012) Laparoendoscopic rendezvous versus preoperative ERCP and laparoscopic cholecystectomy for the management of cholecysto-choledocholithiasis: interim analysis of a controlled randomized trial. Ann Surg 255:435–439
Koc B, Karahan S, Adas G, Tutal F, Guven H, Ozsoy A (2013) Comparison of laparoscopic common bile duct exploration and endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for choledocholithiasis: a prospective randomized study. Am J Surg 206:457–463
Rogers SJ, Cello JP, Horn JK, Siperstein AE, Schecter WP, Campbell AR, Mackersie RC, Rodas A, Kreuwel HT, Harris HW (2010) Prospective randomized trial of LC+LCBDE vs ERCP/S+LC for common bile duct stone disease. Arch Surg 145:28–33
Bansal VK, Misra MC, Rajan K, Kilambi R, Kumar S, Krishna A, Kumar A, Pandav CS, Subramaniam R, Arora MK, Garg PK (2014) Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with concomitant gallbladder stones and common bile duct stones: a randomized controlled trial. Surg Endosc 28:875–885
Dasari BV, Tan CJ, Gurusamy KS, Martin DJ, Kirk G, McKie L, Diamond T, Taylor MA (2013) Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev 2013:Cd003327
Vettoretto N, Arezzo A, Famiglietti F, Cirocchi R, Moja L, Morino M (2018) Laparoscopic-endoscopic rendezvous versus preoperative endoscopic sphincterotomy in people undergoing laparoscopic cholecystectomy for stones in the gallbladder and bile duct. Cochrane Database Syst Rev 2018:Cd010507
Li ZQ, Sun JX, Li B, Dai XQ, Yu AX, Li ZF (2020) Meta-analysis of single-stage versus two-staged management for concomitant gallstones and common bile duct stones. J Minim Access Surg 16:206–214
Okamoto K, Suzuki K, Takada T, Strasberg SM, Asbun HJ, Endo I, Iwashita Y, Hibi T, Pitt HA, Umezawa A, Asai K, Han HS, Hwang TL, Mori Y, Yoon YS, Huang WS, Belli G, Dervenis C, Yokoe M, Kiriyama S, Itoi T, Jagannath P, Garden OJ, Miura F, Nakamura M, Horiguchi A, Wakabayashi G, Cherqui D, de Santibañes E, Shikata S, Noguchi Y, Ukai T, Higuchi R, Wada K, Honda G, Supe AN, Yoshida M, Mayumi T, Gouma DJ, Deziel DJ, Liau KH, Chen MF, Shibao K, Liu KH, Su CH, Chan ACW, Yoon DS, Choi IS, Jonas E, Chen XP, Fan ST, Ker CG, Giménez ME, Kitano S, Inomata M, Hirata K, Inui K, Sumiyama Y, Yamamoto M (2018) Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci 25:55–72
European Association for the Study of the Liver (EASL) (2016) EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol 65:146–181
Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, Pitt HA, Garden OJ, Kiriyama S, Hata J, Gabata T, Yoshida M, Miura F, Okamoto K, Tsuyuguchi T, Itoi T, Yamashita Y, Dervenis C, Chan AC, Lau WY, Supe AN, Belli G, Hilvano SC, Liau KH, Kim MH, Kim SW, Ker CG (2013) TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 20:35–46
Fuks D, Mouly C, Robert B, Hajji H, Yzet T, Regimbeau JM (2012) Acute cholecystitis: preoperative CT can help the surgeon consider conversion from laparoscopic to open cholecystectomy. Radiology 263:128–138
Ding G, Cai W, Qin M (2014) Single-stage vs. two-stage management for concomitant gallstones and common bile duct stones: a prospective randomized trial with long-term follow-up. J Gastrointest Surg 18:947–951
Lv F, Zhang S, Ji M, Wang Y, Li P, Han W (2016) Single-stage management with combined tri-endoscopic approach for concomitant cholecystolithiasis and choledocholithiasis. Surg Endosc 30:5615–5620
Miura F, Takada T, Strasberg SM, Solomkin JS, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Yoshida M, Mayumi T, Okamoto K, Gomi H, Kusachi S, Kiriyama S, Yokoe M, Kimura Y, Higuchi R, Yamashita Y, Windsor JA, Tsuyuguchi T, Gabata T, Itoi T, Hata J, Liau KH (2013) TG13 flowchart for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 20:47–54
Wakabayashi G, Iwashita Y, Hibi T, Takada T, Strasberg SM, Asbun HJ, Endo I, Umezawa A, Asai K, Suzuki K, Mori Y, Okamoto K, Pitt HA, Han HS, Hwang TL, Yoon YS, Yoon DS, Choi IS, Huang WS, Giménez ME, Garden OJ, Gouma DJ, Belli G, Dervenis C, Jagannath P, Chan ACW, Lau WY, Liu KH, Su CH, Misawa T, Nakamura M, Horiguchi A, Tagaya N, Fujioka S, Higuchi R, Shikata S, Noguchi Y, Ukai T, Yokoe M, Cherqui D, Honda G, Sugioka A, de Santibañes E, Supe AN, Tokumura H, Kimura T, Yoshida M, Mayumi T, Kitano S, Inomata M, Hirata K, Sumiyama Y, Inui K, Yamamoto M (2018) Tokyo Guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 25:73–86
Grubnik VV, Tkachenko AI, Ilyashenko VV, Vorotyntseva KO (2012) Laparoscopic common bile duct exploration versus open surgery: comparative prospective randomized trial. Surg Endosc 26:2165–2171
Bencini L, Tommasi C, Manetti R, Farsi M (2014) Modern approach to cholecysto-choledocholithiasis. World J Gastrointest Endosc 6:32–40
van Dijk AH, Lamberts M, van Laarhoven CJ, Drenth JP, Boermeester MA, de Reuver PR (2014) Laparoscopy in cholecysto-choledocholithiasis. Best Pract Res Clin Gastroenterol 28:195–209
Buxbaum JL, Abbas Fehmi SM, Sultan S, Fishman DS, Qumseya BJ, Cortessis VK, Schilperoort H, Kysh L, Matsuoka L, Yachimski P, Agrawal D, Gurudu SR, Jamil LH, Jue TL, Khashab MA, Law JK, Lee JK, Naveed M, Sawhney MS, Thosani N, Yang J, Wani SB (2019) ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc 89:1075-1105.e1015
Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, Devière J, Dinis-Ribeiro M, Dumonceau JM, Giovannini M, Gyokeres T, Hafner M, Halttunen J, Hassan C, Lopes L, Papanikolaou IS, Tham TC, Tringali A, van Hooft J, Williams EJ (2016) Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 48:657–683
Choi K, Amarasena T, Hughes A, Shaw I, Iswariah H, Tam D, Franz R, Chandrasegaram M (2020) Management of bile duct stones at cholecystectomy: an Australian single-centre experience over 2 years. Surg Endosc. https://doi.org/10.1007/s00464-020-07495-7
Zhu J, Sun G, Hong L, Li X, Li Y, Xiao W (2018) Laparoscopic common bile duct exploration in patients with previous upper abdominal surgery. Surg Endosc 32:4893–4899
Poh BR, Ho SP, Sritharan M, Yeong CC, Swan MP, Devonshire DA, Cashin PA, Croagh DG (2016) Randomized clinical trial of intraoperative endoscopic retrograde cholangiopancreatography versus laparoscopic bile duct exploration in patients with choledocholithiasis. Br J Surg 103:1117–1124
Cao AM, Eslick GD, Cox MR (2016) Early laparoscopic cholecystectomy is superior to delayed acute cholecystitis: a meta-analysis of case-control studies. Surg Endosc 30:1172–1182
Salman B, Yilmaz U, Kerem M, Bedirli A, Sare M, Sakrak O, Tatlicioglu E (2009) The timing of laparoscopic cholecystectomy after endoscopic retrograde cholangiopancreaticography in cholelithiasis coexisting with choledocholithiasis. J Hepatobiliary Pancreat Surg 16:832–836
Zhumatayev DT, Baimakhanov AN, Abdykadyrov MK, Nurmakov DA, Raimkhanov AD, Smagulov AM, Abdiyev NM (2020) Simultaneous surgical treatment tactics of acute destructive cholecystitis combined with choledocholithiasis: a case report. Int J Surg Case Rep 70:230–233
Saber A, Hokkam EN (2014) Operative outcome and patient satisfaction in early and delayed laparoscopic cholecystectomy for acute cholecystitis. Minim Invasive Surg 2014:162643
Rajcok M, Bak V, Danihel L, Kukucka M, Schnorrer M (2016) Early versus delayed laparoscopic cholecystectomy in treatment of acute cholecystitis. Bratisl Lek Listy 117:328–331
Singh AN, Kilambi R (2018) Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with gallbladder stones with common bile duct stones: systematic review and meta-analysis of randomized trials with trial sequential analysis. Surg Endosc 32:3763–3776
Pan L, Chen M, Ji L, Zheng L, Yan P, Fang J, Zhang B, Cai X (2018) The safety and efficacy of laparoscopic common bile duct exploration combined with cholecystectomy for the management of cholecysto-choledocholithiasis: an up-to-date meta-analysis. Ann Surg 268:247–253
Saito H, Koga T, Sakaguchi M, Kadono Y, Kamikawa K, Urata A, Imamura H, Tada S, Kakuma T, Matsushita I (2019) Post-endoscopic retrograde cholangiopancreatography pancreatitis in patients with asymptomatic common bile duct stones. J Gastroenterol Hepatol 34:1153–1159
Qian Y, Xie J, Jiang P, Yin Y, Sun Q (2020) Laparoendoscopic rendezvous versus ERCP followed by laparoscopic cholecystectomy for the management of cholecysto-choledocholithiasis: a retrospectively cohort study. Surg Endosc 34:2483–2489
Jiang C, Zhao X, Cheng S (2019) T-Tube use after laparoscopic common bile duct exploration. JSLS 23(e2018):00077
Gurusamy KS, Koti R, Davidson BR (2013) T-tube drainage versus primary closure after laparoscopic common bile duct exploration. Cochrane Database Syst Rev 2013:Cd005641
Xiao LK, Xiang JF, Wu K, Fu X, Zheng MY, Song XX, Xie W (2018) The reasonable drainage option after laparoscopic common bile duct exploration for the treatment of choledocholithiasis. Clin Res Hepatol Gastroenterol 42:564–569
Podda M, Polignano FM, Luhmann A, Wilson MS, Kulli C, Tait IS (2016) Systematic review with meta-analysis of studies comparing primary duct closure and T-tube drainage after laparoscopic common bile duct exploration for choledocholithiasis. Surg Endosc 30:845–861
Zhou H, Wang S, Fan F, Peng J (2020) Primary closure with knotless barbed suture versus traditional T-tube drainage after laparoscopic common bile duct exploration: a single-center medium-term experience. J Int Med Res 48:300060519878087
He MY, Zhou XD, Chen H, Zheng P, Zhang FZ, Ren WW (2018) Various approaches of laparoscopic common bile duct exploration plus primary duct closure for choledocholithiasis: a systematic review and meta-analysis. Hepatobiliary Pancreat Dis Int 17:183–191
Yin Z, Xu K, Sun J, Zhang J, Xiao Z, Wang J, Niu H, Zhao Q, Lin S, Li Y (2013) Is the end of the T-tube drainage era in laparoscopic choledochotomy for common bile duct stones is coming? A systematic review and meta-analysis. Ann Surg 257:54–66
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Yong Yan, Yanhua Sha, Wei Yuan, Hui Yuan, Xuanjin Zhu, and Bailin Wang have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yan, Y., Sha, Y., Yuan, W. et al. One-stage versus two-stage management for acute cholecystitis associated with common bile duct stones: a retrospective cohort study. Surg Endosc 36, 920–929 (2022). https://doi.org/10.1007/s00464-021-08349-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08349-6