Abstract
Background
Bariatric surgical procedures have recognized benefits for morbidly obese patients. Unfortunately, staple line leaks remain a profound complication after these procedures. Currently available intraoperative surveillance modalities have multiple drawbacks, such as requiring an available upper endoscope and experienced endoscopist. Additionally, increased procedure time and resources are needed to perform intraoperative endoscopy and maintain equipment.
Methods
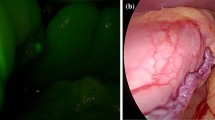
This is a retrospective cohort study of all bariatric patients undergoing Roux-en-Y gastric bypass or sleeve gastrectomy procedures performed by one attending surgeon at a tertiary care facility designated as a bariatric surgical center of excellence. Patients were grouped based on procedure date being before (September 2016 to mid-October 2018) or after (mid-October 2018 to March 2019) implementation of a novel intraluminal indocyanine green leak testing protocol. Diluted indocyanine green was injected via orogastric bougie intraluminally at the location of the gastric staple line and observed with near-infrared imaging from the intraperitoneal perspective for evidence of immunofluorescence extravasation. Data from the electronic medical record and bariatric surgical outcomes database were gathered to analyze the sensitivity and specificity of this new intraoperative diagnostic modality.
Results
Total of 196 patients underwent bariatric surgery with intraoperative leak testing using the gastroscopy method; of these, there were 3 false negatives and 193 true negatives. Total of 59 patients underwent bariatric surgery with intraoperative leak testing using the intraluminal ICG method; of these, there was 1 true positive, 1 false positive, 0 false negatives, and 57 true negatives. Indocyanine green leak testing had a sensitivity of 100.00% and specificity of 98.28%.
Conclusions
Intraluminal indocyanine green is an alternative for intraoperative detection of staple line integrity during bariatric surgical procedures with comparable specificity to intraoperative gastroscopy.


Similar content being viewed by others
Abbreviations
- ICG:
-
Indocyanine green
- MBSAQIP:
-
Metabolic and bariatric surgery accreditation and quality improvement program
- BMI:
-
Body mass index
- RYGB:
-
Roux-en-Y gastric bypass
- SG:
-
Sleeve gastrectomy
- SD:
-
Standard deviation
References
Kirby GC, Macano CAW, Nyasavajjala SM, Sahloul M, Nijjar R, Daskalakis M, Richardson M, Singhal R (2017) The Birmingham experience of high-pressure methylene blue dye test during primary and revisional bariatric surgery: a retrospective cohort study. Ann Med Surg (Lond) 23:32–34
Bingham J, Kaufman J, Hata K et al (2017) A multicenter study of routine versus selective intraoperative leak testing for sleeve gastrectomy. Surg Obes Relat Dis 27:240–245
Špička P (2017) Staple line leak with peritonitis after laparoscopic sleeve gastrectomy—a solution in one to six steps. Other Miniinvasive Tech 2(3):154–159
Arndtz K, Steed H, Hodson J, Manjunath S (2016) The hidden endoscopic burden of sleeve gastrectomy and its comparison with Roux-en-Y gastric bypass. Ann Gastroenterol. 29(1):44–49
Puli DR, Spofford IS, Thompson CC (2012) Use of self-expandable stents in the treatment of bariatric surgery leaks: a systematic review and meta-analysis. Gastrointest Endosc 75(2):287–293
Kim J, Azagury D, Eisenberg D, DeMaria E, Campos GM, American Society for Metabolic and Bariatric Surgery Clinical Issues Committee (2015) ASMBS position statement on prevention, detection, and treatment of gastrointestinal leak after gastric bypass and sleeve gastrectomy, including the roles of imaging, surgical exploration, and nonoperative management. Surg Obes Relat Dis 11(4):739–748.
Aurora AR, Khaitan L, Saber AA (2012) Sleeve gastrectomy and the risk of leak: a systematic analysis of 4888 patients. Surg Endosc 26(6):1509–1515
Sethi M, Zagzag J, Patel K, Magrath M, Somoza E, Parikh MS, Saunders JK, Ude-Welcome A, Schwack BF, Kurian MS, Fielding GA, Ren-Fielding CJ (2016) ntraoperative leak testing has no correlation with leak after laparoscopic sleeve gastrectomy. Surg Endosc 30(3):883–891
Gonzalez R, Sarr MG, Smith CD, Baghai M, Kendrick M, Szomstein S, Rosenthal R, Murr MM (2007) Diagnosis and contemporary management of anastomotic leaks after gastric bypass for obesity. J Am Coll Surg 204(1):47–55
Bingham J, Lallemand M, Barron M, Kuckelman J, Carter P, Blair K, Martin M (2016) Routine intraoperative leak testing for sleeve gastrectomy: is the leak test full of hot air? Am J Surg 211(5):943–947
Mohos E, Schmaldienst E, Richter D, Prager M (2011) Examination of the efficacy and safety of intraoperative gastroscopic testing of the gastrojejunal anastomosis in laparoscopic Roux Y gastric bypass surgery. Obes Surg. 21(10):1592–1596
Abou Rached A, Basile M, El Masri H (2014) Gastric leaks post sleeve gastrectomy: review of its prevention and management. World J Gastroenterol 20(38):13904–13910
Csendes A, Burdiles P, Burgos AM et al (2005) Conservative management of anastomotic leaks after 557 open gastric bypasses. Obes Surg 18(9):1252–1256
Praveenraj P, Gomes RM, Kumar S et al (2016) Management of gastric leaks after laparoscopic sleeve gastrectomy for morbid obesity: a tertiary care experience and design of a management algorithm. J Minim Access Surg 12(4):342–349
Miller KA, Pump A (2007) Use of bioabsorbable staple reinforcement material in gastric bypass: a prospective randomized clinical trial. Surg Obes Relat Dis 3(4):417–421
Shikora SA (2011) The use of staple-line reinforcement during laparoscopic gastric bypass. Obes Surg. 14(10):1313–1320
Sapala JA, Wood MH, Schuhknecht MP (2004) Anastomotic leak prophylaxis using a vapor-heated fibrin sealant: report on 738 gastric bypass patients. Obes Surg 14(1):35–42
Livingston EH, Liu CY, Glantz G, Li Z (2003) Characteristics of bariatric surgery in an integrated VA Health Care System: follow-up and outcomes. J Surg Res 109(2):138–143
Silecchia G, Boru C, Pecchia A, Rizzello M, Casella G, Leonetti F, Basso N (2006) Effectiveness of laparoscopic sleeve gastrectomy (first stage of biliopancreatic diversion with duodenal switch) on co-morbidities in super-obese high-risk patients. Obes Surg 16(9):1138–1144
Nandakumar G, Richards BG, Trencheva K, Dakin G (2010) Surgical adhesive increases burst pressure and seals leaks in stapled gastrojejunostomy. Surg Obes Relat Dis 6(5):498–501
Theodorou D, Doulami G, Larentzakis A, Almpanopoulos K, Stamou K, Zografos G, Menenakos E (2012) Bougie insertion: a common practice with underestimated dangers. Int J Surg Case Rep 3(2):74–77
Acknowledgements
Authors would like to acknowledge Katherine Shaver for her expert assistance verifying our statistical analysis.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
CLK, CMR, CLP and ADS do not have any financial or nonfinancial conflicts of interest to disclose.
Ethical approval
This research was approved by the Institutional Review Board of Virginia Tech Carilion.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 78386 kb)
Rights and permissions
About this article
Cite this article
Kalmar, C.L., Reed, C.M., Peery, C.L. et al. Intraluminal indocyanine green for intraoperative staple line leak testing in bariatric surgery. Surg Endosc 34, 4194–4199 (2020). https://doi.org/10.1007/s00464-020-07606-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07606-4