Abstract
Background
As the use of minimally invasive techniques in colorectal surgery has become increasingly prevalent, concerns remain about the oncologic effectiveness and long-term outcomes of minimally invasive low anterior resection (MI-LAR) for the treatment of rectal cancer.
Study design
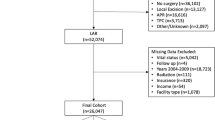
The 2010–2015 National Cancer Database (NCDB) Participant Data Use File was queried for patients undergoing elective open LAR (OLAR) or MI-LAR for rectal adenocarcinoma. A 1:1 propensity match was performed on the basis of demographics, comorbidity, and tumor characteristics. Outcomes were compared between groups and Cox proportional hazard modeling was performed to identify independent predictors of mortality. A subset analysis was performed on high-volume academic centers.
Results
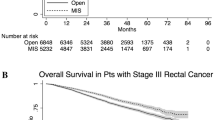
35,809 patients undergoing LAR were identified of whom 18,265 (51.0%) underwent MI-LAR. After propensity matching, patients receiving MI-LAR were less likely to have a positive circumferential radial margin (CRM) (5.5% vs. 6.6%, p = 0.0094) or a positive distal margin (3.6% vs. 4.6%, p = 0.0022) and had decreased 90-day all-cause mortality (2.0% vs. 2.6%, p = 0.0238). MI-LAR resulted in decreased hospital length of stay (5 vs. 6 days, p < 0.0001) but a greater rate of 30-day readmission (7.6% vs. 6.5%, p = 0.0054). Long-term overall survival was improved with MI-LAR (79% vs. 76%, p < 0.0001). Cox proportional hazard modeling demonstrated a decreased risk of mortality with MI-LAR (HR 0.859, 95% CI 0.788–0.937).
Conclusion
MI-LAR is associated with improvement in CRM clearance and long-term survival. In the hands of experienced surgeons with advanced laparoscopy skills, MI-LAR appears safe and effective technique for the management of rectal cancer.

Similar content being viewed by others
References
American Cancer Society (2017) Colorectal Cancer Facts & Figures 2017-2019. Atlanta, pp 1–40
Esemuede IO, Gabre-Kidan A, Fowler DL, Kiran RP (2015) Risk of readmission after laparoscopic vs. open colorectal surgery. Int J Colorectal Dis 30(11):1489–1494
Pasam RT, Esemuede IO, Lee-Kong SA, Kiran RP (2015) The minimally invasive approach is associated with reduced surgical site infections in obese patients undergoing proctectomy. Tech Coloproctol 19(12):733–743
Read TE (2007) Laparoscopic proctectomy for rectal adenocarcinoma. J Surg Oncol 96:660–664
Turner M, Adam MA, Sun Z, Kim J, Ezekian B, Yerokun B et al (2017) Insurance status, not race, is associated with use of minimally invasive surgical approach for rectal cancer. Ann Surg 265:774–781
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes the ACOSOG Z6051 randomized clinical trial. JAMA-J Am Med Assoc 314(13):1346–1355
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AMH et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): Multicentre, randomised controlled trial. Lancet 365(9472):1718–1726
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15(7):767–774
Bemelman WA, Ph D, Andersson J, Angenete E, Ph D, Rosenberg J et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Stevenson ARL, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ et al (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA-J Am Med Assoc 314(13):1356–1363
Boffa DJ, Rosen JE, Mallin K, Loomis A, Gay G, Palis B et al (2017) Using the national cancer database for outcomes research. JAMA Oncol 3:1722–1728
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AMH et al (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-Year results of the UK MRC CLASICC trial group. J Clin Oncol 25(21):3061–3068
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ (2010) Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 97(11):1638–1645
Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG et al (2013) Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg 100(1):75–82
van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC et al (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14(3):210–218
Baik SH, Kwon HY, Kim JS, Hur H, Sohn SK, Cho CH et al (2009) Robotic versus laparoscopic low anterior resection of rectal cancer: short-term outcome of a prospective comparative study. Ann Surg Oncol 16(6):1480–1487
Zhou T, Zhang G, Tian H, Liu Z, Xia S (2014) Laparoscopic rectal resection versus open rectal resection with minilaparotomy for invasive rectal cancer. J Gastrointest Oncol 5(1):36–45
Sammour T, Malakorn S, Bednarski BK, Kaur H, Shin US, Messick C et al (2018) Oncological outcomes after robotic proctectomy for rectal cancer: analysis of a prospective database. Ann Surg 267(3):521–526
Boutros M, Hippalgaonkar N, Silva E, Allende D, Wexner SD, Berho M (2013) Laparoscopic resection of rectal cancer results in higher lymph node yield and better short-term outcomes than open surgery: a large single-center comparative study. Dis Colon Rectum 56(6):679–688
Barnajian M, Pettet D, Kazi E, Foppa C, Bergamaschi R (2014) Quality of total mesorectal excision and depth of circumferential resection margin in rectal cancer: a matched comparison of the first 20 robotic cases. Color Dis 16(8):603–609
Hatwell C, Bretagnol F, Farges O, Belghiti J, Panis Y (2013) Laparoscopic resection of colorectal cancer facilitates simultaneous surgery of synchronous liver metastases. Color Dis 15(1):e21–e28
de’Angelis N, Landi F, Vitali GC, Memeo R, Martínez-Pérez A, Solis A et al (2017) Multicentre propensity score-matched analysis of laparoscopic versus open surgery for T4 rectal cancer. Surg Endosc Other Interv Tech 31(8):3106–3121
Greenblatt DY, Rajamanickam V, Pugely AJ, Heise CP, Foley EF, Kennedy GD (2011) Short-term outcomes after laparoscopic-assisted proctectomy for rectal cancer: results from the ACS NSQIP. J Am Coll Surg 212(5):844–854
Sun Z, Kim J, Adam MA, Nussbaum DP, Speicher PJ, Mantyh CR et al (2016) Minimally invasive versus open low anterior resection equivalent survival in a national analysis of 14,033 patients with rectal cancer. Ann Surg 263(6):1152–1158
Speicher PJ, Englum BR, Ganapathi AM, Nussbaum DP, Mantyh CR, Migaly J (2015) Robotic low anterior resection for rectal cancer: a national perspective on short-term oncologic outcomes. Ann Surg 262(6):1040–1045
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J et al (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer. JAMA 318(16):1569
Nussbaum DP, Speicher PJ, Ganapathi AM, Englum BR, Keenan JE, Mantyh CR et al (2014) Laparoscopic versus open low anterior resection for rectal cancer: results from the national cancer data base. J Gastrointest Surg 19:124–132
Sujatha-Bhaskar S, Jafari MD, Gahagan JV, Inaba CS, Koh CY, Mills SD et al (2017) Defining the role of minimally invasive proctectomy for locally advanced rectal adenocarcinoma. Ann Surg 266(4):574–581
Kayano H, Okuda J, Tanaka K, Kondo K, Tanigawa N (2011) Evaluation of the learning curve in laparoscopic low anterior resection for rectal cancer. Surg Endosc 25(9):2972–2979
Cagino K, Altieri MS, Yang J, Nie L, Talamini M, Spaniolas K et al (2017) Effect of academic status on outcomes of surgery for rectal cancer. Surg Endosc 32:2774–2780
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Brian Gilmore, Mohamed A. Adam, Kristen Rhodin, Megan C. Turner, Brian Ezekian, Christopher R. Mantyh, John Migaly have no financial ties or conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
NCDB Provision Disclosure: The National Cancer Data Base (NCDB) is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The CoC's NCDB and the hospitals participating in the CoC NCDB are the source of the de-identified data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the author.
Rights and permissions
About this article
Cite this article
Gilmore, B., Adam, M.A., Rhodin, K. et al. Evolution of minimally invasive surgery for rectal cancer: update from the national cancer database. Surg Endosc 35, 275–290 (2021). https://doi.org/10.1007/s00464-020-07393-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07393-y