Abstract
Background
There is currently no consensus regarding the relative applicability of minimally invasive treatment, including radiofrequency ablation (RFA) and minimally invasive surgery (MIS) in patients with a single small peripheral hepatocellular carcinoma (HCC) and compensated cirrhosis. This study investigated the clinical outcomes of MIS and RFA for single subcapsular HCC ≤ 2 cm in patients with compensated cirrhosis.
Methods
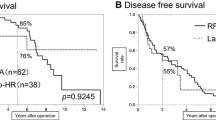
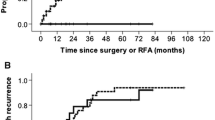
In this retrospective study, we enrolled 75 patients who had a single subcapsular HCC ≤ 2 cm along with Child–Pugh class A cirrhosis and a preoperative platelet count ≥ 100 k/μl. These patients underwent RFA (n = 39) or MIS (n = 36) between 2010 and 2016. Clinical outcomes including disease-free survival (DFS), survival without recurrence beyond the Milan criteria (RBM), and overall survival (OS) were compared.
Results
The 7-year DFS rates in the MIS and RFA groups were 86.1% and 35.9% (p < 0.001), respectively, the 7-year RBM rates were 88.9% and 66.7% (p = 0.014), respectively, and the 7-year OS rates were 97.2% and 82.1% (p = 0.008), respectively. RFA was associated with more ipsilateral lobe recurrence (20% vs. 83.4%, p = 0.004), and 40% were in direct contact with the ablation penumbra. A Cox proportional hazard analysis identified RFA as an independent predictor of mortality (adjusted hazard ratio, 9.625, p = 0.038). No major complications occurred in either group. RFA patients had a shorter hospital stay (median of 2 vs. 6 days, p < 0.001) and operation time (median of 23.5 vs. 216 min, p = 0.001).
Conclusions
MIS was associated with a better 7-year OS, RBM, and DFS among patients with single subcapsular HCC ≤ 2 cm, Child–Pugh A liver function, and no clinically significant portal hypertension when compared to those who underwent percutaneous RFA.



Similar content being viewed by others
References
Ferlay J, Soerjomataram I, Dikshit R et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359–386
Kudo M (2010) The 2008 Okuda lecture: management of hepatocellular carcinoma: from surveillance to molecular targeted therapy. J Gastroenterol Hepatol 25:439–452
European Association For The Study of the Liver, European Organisation for Research and Treatment of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56:908–943
Bruix J, Sherman M, American Association for the Study of Liver Diseases (2011) Management of hepatocellular carcinoma: an update. Hepatology 53:1020–1022
Cheung TT, Poon RT, Yuen WK et al (2013) Long-term survival analysis of pure laparoscopic versus open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a single-center experience. Ann Surg 257:506–511
Ishizawa T, Gumbs AA, Kokudo N, Gayet B (2012) Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 256:959–964
Hirokawa F, Hayashi M, Miyamoto Y et al (2015) Short- and long-term outcomes of laparoscopic versus open hepatectomy for small malignant liver tumors: a single-center experience. Surg Endosc 29:458–465
Lin SM (2013) Local ablation for hepatocellular carcinoma in taiwan. Liver Cancer 2:73–83
Huang J, Yan L, Cheng Z et al (2010) A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria. Ann Surg 252:903–912
Chen PD, Wu CY, Hu RH et al (2017) Robotic versus open hepatectomy for hepatocellular carcinoma: a matched comparison. Ann Surg Oncol 24:1021–1028
Vigano L, Laurenzi A, Solbiati L, Procopio F, Cherqui D, Torzilli G (2018) Open liver resection, laparoscopic liver resection, and percutaneous thermal ablation for patients with solitary small hepatocellular carcinoma (%3c/=30 mm): review of the literature and proposal for a therapeutic strategy. Dig Surg 35:359–371
Omata M, Lesmana LA, Tateishi R et al (2010) Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int 4:439–474
Lau WY, Lai EC (2009) The current role of radiofrequency ablation in the management of hepatocellular carcinoma: a systematic review. Ann Surg 249:20–25
Vietti Violi N, Duran R, Guiu B et al (2018) Efficacy of microwave ablation versus radiofrequency ablation for the treatment of hepatocellular carcinoma in patients with chronic liver disease: a randomised controlled phase 2 trial. Lancet Gastroenterol Hepatol 3:317–325
Song J, Wang Y, Ma K et al (2016) Laparoscopic hepatectomy versus radiofrequency ablation for minimally invasive treatment of single, small hepatocellular carcinomas. Surg Endosc 30:4249–4257
Lai ZC, Liang JY, Chen LD et al (2018) Do hepatocellular carcinomas located in subcapsular space or in proximity to vessels increase the rate of local tumor progression? A meta-analysis. Life Sci 207:381–385
Bruix J, Sherman M, Practice Guidelines Committee, American Association for the Study of Liver Diseases (2005) Management of hepatocellular carcinoma. Hepatology 42:1208–1236
Chen C-J, Chang W-H, Shih S-C, Wang T-E, Chang C-W, Chen M-J (2009) Clinical presentation and outcome of hepatic subcapsular fluid collections. J Formos Med Assoc 108:61–68
Lee JW, Kim S, Kwack SW et al (2008) Hepatic capsular and subcapsular pathologic conditions: demonstration with CT and MR imaging. Radiographics 28:1307–1323
Filippousis P, Sotiropoulou E, Manataki A, Konstantinopoulos O, Thanos L (2011) Radiofrequency ablation of subcapsular hepatocellular carcinoma: single center experience. Eur J Radiol 77:299–304
Bonny C, Abergel A, Gayard P et al (2002) Radiofrequency ablation of hepatocellular carcinoma in patients with cirrhosis. Gastroentérol Clin Biol 26:735–741
Llovet JM, Vilana R, Bru C et al (2001) Increased risk of tumor seeding after percutaneous radiofrequency ablation for single hepatocellular carcinoma. Hepatology 33:1124–1129
Oken MM, Creech RH, Tormey DC et al (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–655
Peck-Radosavljevic M (2017) Thrombocytopenia in chronic liver disease. Liver Int 37:778–793
George JN (2000) Platelets. Lancet 355:1531–1539
Maan R, de Knegt RJ, Veldt BJ (2015) Management of thrombocytopenia in chronic liver disease: focus on pharmacotherapeutic strategies. Drugs 75:1981–1992
Liang JD, Ping XO, Tseng YJ, Huang GT, Lai F, Yang PM (2014) Recurrence predictive models for patients with hepatocellular carcinoma after radiofrequency ablation using support vector machines with feature selection methods. Comput Methods Programs Biomed 117:425–434
Lee BC, Liu KL, Wu CH et al (2018) Comparison of radiofrequency ablation and transarterial chemoembolization for hepatocellular carcinoma in the caudate lobe. Cardiovasc Intervent Radiol 41:1699–1707
Ho CM, Wakabayashi G, Nitta H et al (2013) Total laparoscopic limited anatomical resection for centrally located hepatocellular carcinoma in cirrhotic liver. Surg Endosc 27:1820–1825
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Balzan S, Belghiti J, Farges O et al (2005) The “50–50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg 242:824–828; discussion 828–829
Farinati F, Sergio A, Baldan A et al (2009) Early and very early hepatocellular carcinoma: when and how much do staging and choice of treatment really matter? A multi-center study. BMC Cancer 9:33
Mazzaferro V, Bhoori S, Sposito C et al (2011) Milan criteria in liver transplantation for hepatocellular carcinoma: an evidence-based analysis of 15 years of experience. Liver Transpl 17(Suppl 2):S44–S57
Villanueva A, Hernandez-Gea V, Llovet JM (2013) Medical therapies for hepatocellular carcinoma: a critical view of the evidence. Nat Rev Gastroenterol Hepatol 10:34–42
Karabulut K, Aucejo F, Akyildiz HY, Siperstein A, Berber E (2012) Resection and radiofrequency ablation in the treatment of hepatocellular carcinoma: a single-center experience. Surg Endosc 26:990–997
Kim GA, Shim JH, Kim MJ et al (2016) Radiofrequency ablation as an alternative to hepatic resection for single small hepatocellular carcinomas. Br J Surg 103:126–135
Liu PH, Hsu CY, Hsia CY et al (2016) surgical resection versus radiofrequency ablation for single hepatocellular carcinoma %3c/= 2 cm in a propensity score model. Ann Surg 263:538–545
Cheung TT, Han HS, She WH et al (2018) The Asia Pacific Consensus Statement on Laparoscopic Liver Resection for Hepatocellular Carcinoma: a report from the 7th Asia-Pacific Primary Liver Cancer Expert Meeting Held in Hong Kong. Liver Cancer 7:28–39
Cucchetti A, Piscaglia F, Cescon M, Ercolani G, Pinna AD (2013) Systematic review of surgical resection vs radiofrequency ablation for hepatocellular carcinoma. World J Gastroenterol 19:4106–4118
Liu H, Wang ZG, Fu SY et al (2016) Randomized clinical trial of chemoembolization plus radiofrequency ablation versus partial hepatectomy for hepatocellular carcinoma within the Milan criteria. Br J Surg 103:348–356
Chen MS, Li JQ, Zheng Y et al (2006) A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Ann Surg 243:321–328
Shouval D (2012) Focus. J Hepatol 57:713–714
Ng KKC, Chok KSH, Chan ACY et al (2017) Randomized clinical trial of hepatic resection versus radiofrequency ablation for early-stage hepatocellular carcinoma. Br J Surg 104:1775–1784
Lee J, Lee JM, Yoon JH et al (2012) Percutaneous radiofrequency ablation with multiple electrodes for medium-sized hepatocellular carcinomas. Korean J Radiol 13:34–43
Cabassa P, Donato F, Simeone F, Grazioli L, Romanini L (2006) Radiofrequency ablation of hepatocellular carcinoma: long-term experience with expandable needle electrodes. AJR Am J Roentgenol 186:S316–321
Potretzke TA, Ziemlewicz TJ, Hinshaw JL et al (2016) Microwave versus radiofrequency ablation treatment for hepatocellular carcinoma: a comparison of efficacy at a single center. J Vasc Interv Radiol 27:631–638
Poggi G, Tosoratti N, Montagna B, Picchi C (2015) Microwave ablation of hepatocellular carcinoma. World J Hepatol 7:2578–2589
Murali AR, Attar BM, Katz A, Kotwal V, Clarke PM (2015) Utility of platelet count for predicting cirrhosis in alcoholic liver disease: model for identifying cirrhosis in a US population. J Gen Intern Med 30:1112–1117
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Chih-Hao Lin, Cheng-Maw Ho, Chih-Horng Wu, Po-Chin Liang, Yao-Ming Wu, Rey-Heng Hu, Po-Huang Lee and Ming-Chih Ho have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, CH., Ho, CM., Wu, CH. et al. Minimally invasive surgery versus radiofrequency ablation for single subcapsular hepatocellular carcinoma ≤ 2 cm with compensated liver cirrhosis. Surg Endosc 34, 5566–5573 (2020). https://doi.org/10.1007/s00464-019-07357-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07357-x