Abstract
Background
The mechanism of persistent chronic pain after TAPP and OLR remains controversial. Therefore, more prospective and well-designed studies are needed to determine the predictive risk factors that will lead to better pain prevention and possibly elimination. The aim of the present study was to investigate the risk factors of chronic pain after TAPP repair and OLR in a single institution.
Methods
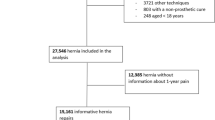
A single-center, retrospective study of propensity score-matched patients who underwent TAPP or OLR surgery between 2008 and 2018 was conducted. To overcome selection bias, we performed 1:1 matching using 6 covariates to generate the propensity score.
Results
A total of 400 patients treated with TAPP and 424 patients treated with OLR were balanced to 400 pairs of matched patients. The patients’ age (P < 0.001), BMI (P < 0.001), foreign body sensation within 3 months after surgery (P < 0.001), and persistent sensation loss (P = 0.002) were different between the two groups. The OLR group had a shorter operative time than did the TAPP group (P < 0.001). The univariate analysis of factors predicting a difference in VAS between the preoperative assessment and the assessment 3 months after surgery showed that the type of surgery (P = 0.004), hernia grade (P = 0.001), type of mesh (P < 0.001), presence of scrotal invasion (P = 0.024), and foreign body sensation within 3 months (P = 0.047) were risk factors. The multivariate analysis revealed that only hernia grade III (CI − 8.524, − 2.783; P < 0.001), OLR operation type (CI 1.069, 4.987; P = 0.002), and the use of polypropylene mesh (CI − 5.400, − 1.489; P = 0.001) were independently associated with chronic pain.
Conclusion
These results suggest that compared to OLR, TAPP leads to less postoperative pain and a better long-term quality of life.

Similar content being viewed by others
References
Claus C, Rocha G, Campos A, Bonin E, Dimbarre D, Loureiro M, Coelho J (2016) Prospective, randomized and controlled study of mesh displacement after laparoscopic inguinal repair: fixation versus no fixation of mesh. Surg Endosc 30:1134–1140
Bittner R, Montgomery MA, Arregui E, Bansal V, Bingener J, Bisgaard T, Buhck H, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Grimes KL, Klinge U, Koeckerling F, Kumar S, Kukleta J, Lomanto D, Misra MC, Morales-Conde S, Reinpold W, Rosenberg J, Singh K, Timoney M, Weyhe D, Chowbey P (2015) Update of guidelines on laparoscopic (TAPP) and endoscopy (TEP) treatment of inguinal hernia (International Endohernia Society). Surg Endosc 29:289–321
Antoniou S, Antoniou G, Bartsch D, Fendrich V, Koch O, Pointner R, Granderath F (2013) Transabdominal preperitoneal versus totally extraperitoneal repair of inguinal hernia: a meta-analysis of randomized studies. Am J Surg 206:245–252
O'Reilly EA, Burke JP, O'Connell PR (2012) A meta-analysis of surgical morbidity and reccurence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg 255:846–853
Pierides GA, Paajanen HE, Vironen JH (2016) Factors predicting chronic pain after open mesh based inguinal hernia repair: a prospective cohort study. Int J Surg 29:165–170
Usher F, Ochsner J, Tuttle L (1958) Use of marlex mesh in the repair of incisional hernias. Am Surg 24:969–974
Köckerling F, Schug-Pass C (2014) What do we know about titanized polypropylene meshes? An evidence-based review of the literature. Hernia 18:445–457
Klinge U, Klosterhalfen B, Müller M, Schumpelick V (1999) Foreign body reaction to meshes used for the repair of abdominal wall hernias. Eur J Surg 165:665–673
Wennergren J, Plymale M, Davenport D, Levy S, Hazey J, Perry K, Stigall K, Roth J (2016) Quality-of-life scores in laparoscopic preperitoneal inguinal hernia repair. Surg Endosc 30:3467–3473
Oguz H, Karagulle E, Turk E, Moray G (2015) Comparison of peritoneal closure techniques in laparoscopic transabdominal preperitoneal inguinal hernia repair: a prospective randomized study. Hernia 19:879–885
Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, Faillace G, Longoni M (2007) Use of human fibrin glue (tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg 245:222–231
Kalliomäki M, Meyerson J, Gunnarsson U, Gordh T, Sandblom G (2008) Long-term pain after inguinal hernia repair in a population-based cohort; risk factors and interference with daily activities. Eur J Pain 12:214–225
Massaron S, Bona S, Fumagalli U, Battafarano F, Elmore U, Rosati R (2007) Analysis of post-surgical pain after inguinal hernia repair: a prospective study of 1440 operations. Hernia 11:517–525
Fränneby U, Sandblom G, Nordin P, Nyrén O, Gunnarsson U (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244:212–219
Wright D, Paterson C, Scott N, Hair A, O'Dwyer PJ (2002) Five year follow-up of patients undergoing laparoscopic or open groin hernia repair: a randomized conttrolled trial. Ann Surg 235:333–337
Bjurstrom M, Nicol A, Amid P, Chen DC (2014) Pain control following inguinal herniorrhaphy: current perspectives. J Pain Res 7:277–290
Lange J, Meyer V, Voropai D, Keus E, Wijsmuller A, Ploeg R, Pierie J (2016) The role of surgical expertise with regard to chronic postoperative inguinal pain (CPIP) after Lichtenstein correction of inguinal hernia: a systematic review. Hernia 20:349–356
Köckerling F, Stechemesser B, Hukauf M, Kuthe A, Schug-Pass C (2016) TEP versus Lichtenstein: which technique is better for the repair of primary unilateral inguinal hernias in men? Surg Endosc 30:3304–3313
Stoppa R (1989) The treatment of complicated groin and incisional hernias. World J Surg 13:545–554
Amid P (2003) The Lichtenstein repair in 2002: an overview of causes of recurrence after Lichtenstein tension-free hernioplasty. Hernia 7:13–16
Callesen T, Bech K, Kehled H (1999) Prospective study of chronic pain after groin hernia repair. Br J Surg 86:1528–1531
van Veen R, Wijsmuller A, Vrijland W, Hop W, Lange J, Jeekel J (2007) Randomized clinical trial of mesh versus non-mesh primary inguinal hernia repair: long-term chronic pain at 10 years. Surgery 142:695–698
van Veen R, Wijsmuller A, Vrijland W, Hop W, Lange J, Jeekel J (2007) Long term follow-up of a randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J Surg 94:506–510
Liu H, Zheng X, Gu Y, Guo S (2014) A meta-analysis examining the use of fibrin glue mesh fixation versus suture mesh fixation in open inguinal hernia repair. Dig Surg 31:444–451
Aasvang E, Gmaehle E, Hansen J, Gmaehle B, Forman J, Schwarz J, Bittner R, Kehlet H (2010) Prdictive risk factors for persistent postherniotomy pain. Anesthesiology 112:957–969
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, Lange Dd, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European hernia society guidelines on the treatment of inguinal hernia in adul patients. Hernia 13:343–403
Rutkow I, Robbins A (1995) Open mesh plug hernioplasty. Prob Gen Surg 12:121–127
O'Dwyer P, Alani A, McConnachie A (2005) Groin hernia repair: postherniorrhaphy pain. World J Surg 29:1062–1065
Nienhuijs S, Staal E, Strobbe L, Rosman C, Groenewoud H, Bleichrodt R (2007) Chronic pain after mesh repair of inguinal hernia: a systematic review. Am J Surg 194:394–400
Dennis R, O'Riordan D (2007) Risk factors for chronic pain after inguinal hernia repair. Ann R Coll Surg Engl 89:218–220
Funding
There was no Grant funding used for this study.
Author information
Authors and Affiliations
Contributions
Study conception and design: AIB, LM, PY. Data collection: PY, LY, ZC, GQ, LH, PF. Statistical analysis: AIB, PY, ZC, GQ, LH. Data interpretation: AIB, LM, PY. Drafting of the manuscript: AIB, LM, PY. Critical revision: AIB, LM.
Corresponding authors
Ethics declarations
Disclosure
Drs. Liuweimin, Pengzhiyong, Liuyingyun, Alpha I. Balde, Zhanghuanchang, Gaoqian, Liangzhenghe, and Panyanfang have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Min, L., Yong, P., Yun, L. et al. Propensity score analysis of outcomes between the transabdominal preperitoneal and open Lichtenstein repair techniques for inguinal hernia repair: a single-center experience. Surg Endosc 34, 5338–5345 (2020). https://doi.org/10.1007/s00464-019-07324-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07324-6