Abstract
Background
Both laparoscopy and endoscopy are image-based procedures, which are less intuitive than traditional open surgery and require extensive training to reach adequate proficiency. Currently, there is lack of understanding as to how the skills in one image-based procedure translate to another, such as endoscopy to laparoscopy and vice versa. The aim of our study was to explore the relationship between endoscopic and laparoscopic skills using a Fundamentals of Laparoscopic Surgery (FLS) trainer, a traditional virtual reality endoscopic trainer and a “desk-top” endoscopic physical simulator.
Methods
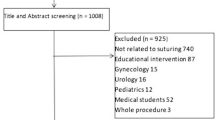
Senior surgical residents from across Canada participating in an advanced laparoscopic foregut training course were enrolled in the study. Participants were assessed performing the FLS laparoscopic suturing task, the Endobubble 2 task (Simbionix, GI Mentor), and a forward viewing peg transfer on the novel Basics in Endoscopic Skills Training Box (BEST Box).
Results
There was significant correlation between the participant’s skill in simulated laparoscopic suturing and simulated endoscopic skill using the BEST box (Pearson coefficient (r) was 0.551 (p = 0.033) and the coefficient of determination (r2) was 0.304). There was a trend towards correlation between laparoscopic suturing time and Endobubble 2 score, but this did not reach statistical significance (r = 0.458, p = 0.086; r2 = 0.210).
Conclusions
Performance in the two physical simulators, laparoscopic suturing and simulated flexible endoscopy using the BEST box, showed a correlation. This study adds to the growing body of evidence that laparoscopic and endoscopic skills are complementary and has the potential to impact simulation training involving both skill sets.





Similar content being viewed by others
References
Berguer R (1999) Surgery and ergonomics. Arch Surg 134:1011–1016
Satava RM, Ellis SR (1994) Human interface technology—an essential tool for the modern surgeon. Surg Endosc 8:817–820
Reyes DA, Tang B, Cuschieri A (2006) Minimal access surgery (MAS)-related surgeon morbidity syndromes. Surg Endosc 20:1–13
Tassios P, Ladas S, Grammenos I et al (1999) Acquisition of competence in colonoscopy: the learning curve of trainees. Endoscopy 31:702–706
Henn P, Gallagher A, Nugent E, Seymour N, Haluck R, Hseino H, Traynor O, Neary P (2018) Visual spatial ability for surgical trainees: implications for learning endoscopic, laparoscopic surgery and other image-guided procedures. Surg Endosc 32:3634–3639. https://doi.org/10.1007/s00464-018-6094-3
Lynch J, Aughwane P, Hammond M (2010) Video games and surgical ability: a literature review. J Surg Educ 67(3):184–189. https://doi.org/10.1016/j.jsurg.2010.02.010
Adamsen S, Funch-Jensen PM, Drewes AM, Rosenberg J, Grantcharov TP (2005) A comparative study of skills in virtual laparoscopy and endoscopy. Surg Endosc 19:229–234. https://doi.org/10.1007/s00464-004-9090-8
Buzink S, Goossens R, Schoon E, Ridder H, Jakimowicz J (2010) Do basic psychomotor skills transfer between different image-based procedures? World J Surg 34:933–940. https://doi.org/10.1007/s00268-010-0432-5
Crespin OM, Okrainec A, Kwong A, Habaz I, Jaminez MC, Szasz P, Weiss E, Gonzalez CG, Mosko JD, Liu LWC, Swanstrom LL, Perretta S, Shlomovitz E (2018) Feasibility of adapting the fundamentals of laparoscopic surgery trainer box to endoscopic skills training tool. Surg Endosc 32:2968–2983
Ritter E, McClusky D, Lederman A, Gallagher A, Smith C (2003) Objective psychomotor skills assessment of experienced and novice flexible endoscopists with a virtual reality simulator. J Gastro Surg 7(7):871–878
Dawe SR, Pena GN, Windsor JA, Broeders JL, Cregan PC, Hewett PJ, Maddern GJ (2014) Systematic review of skills transfer after surgical simulation-based training. Br J Surg 101:1063–1076
Bittner JGT, Coverdill JE, Imam T, Deladisma AM, Edwards MA, Mellinger JD (2008) Do increased training requirements in gastrointestinal endoscopy and advanced laparoscopy necessitate a paradigm shift? A survey of program directors in surgery. J Surg Educ 65:418–430
MacFadyen BV Jr, Vecchio R, Ricardo AE, Mathis CR (1998) Bile duct injury after laparoscopic cholecystectomy: the United States experience. Surg Endosc 12:315–321
Watson DI, Baigrie RJ, Jamieson GG (1996) A learning curve for laparoscopic fundoplication: definable, avoidable, or a waste of time? Ann Surg 224:198–203
Jeffries MA, Lawitz E, Schutz S, Hemmer P (2003) Acquisition of global competency in colonoscopy during fellowship training. Gastrointest Endosc 57:108
Wexner SD, Garbus JE, Singh JJ (2001) A prospective analysis of 13,580 colonoscopies. Reevaluation of credentialing guidelines. Surg Endosc 15(3):251–261
Gardner A, Willis RE, Dunkin BJ, Van Sickle KR, Brown KM, Truitt MS, Uecker JM, Gentry L, Scott DJ (2016) What do residents need to be competent laparoscopic and endoscopic surgeons? Surg Endosc 30(7):3050–3930. https://doi.org/10.1007/s00464-015-4597-8
Aggarwal R, Ranganathan P (2016) Common pitfalls in statistical analysis: the use of correlation techniques. Perspect Clin Res 7(4):187–190. https://doi.org/10.4103/2229-3485.192046
Derossis AM, Fried GM, Abrahamowicz M, Sigman HH, Barkun JS, Meakins JL (1998) Development of a model for training and evaluation of laparoscopic skills. Am J Surg 175:482–487
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jennifer Koichopolos, Jeffrey Hawel, Eran Shlomovitz, Ilay Habaz, Ahmad Elnahas, Nawar A. Alkhamesi, and Christopher M. Schlachta have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Koichopolos, J., Hawel, J., Shlomovitz, E. et al. Correlation of surgical trainee performance on laparoscopic versus endoscopic simulation. Surg Endosc 34, 2007–2011 (2020). https://doi.org/10.1007/s00464-019-06978-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06978-6