Abstract
Background
During laparoscopic groin hernia repair, the surgeon may transect the round ligament of uterus to facilitate mesh placement. Transection during open repair is rarer and anatomically further from the uterus. Our aim was to compare long-term genitourinary outcomes, particularly genital prolapse, between open and laparoscopic repair in women with a primary groin hernia.
Methods
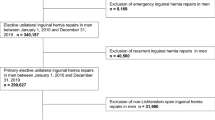
The study was reported according to RECORD guidelines. All women having received a primary anterior open or laparoscopic groin hernia repair from 1998 to 2014 were identified through The Danish Hernia Database and linked with data from The Danish National Patient Registry and the Danish Register of Causes of Death. Our outcome was postoperative genital prolapse and other long-term complications related to gynecology, urology, and infertility.
Results
We included 10,867 women having received a primary groin hernia repair, 7732 (71%) had an open anterior repair and 3135 (29%) a laparoscopic repair. The median (range) age was 59 (19–102) and 64 (18–105), respectively (p < 0.001). Median follow-up was 65 (range 0–203) months. After open repair, 313/7340 (4.2%) had a postoperative genital prolapse, and 46/2,934 (1.5%) after laparoscopic repair (p < 0.001). In multivariate Cox Regression analyses adjusting for age and hernia type, there were no difference between the two methods (p = 0.474). Women with an inguinal hernia had a higher risk of genital prolapse than women with a femoral hernia, independent of repair method [HR = 1.455 (1.143–1.853), p = 0.002]. We found no significant differences between open and laparoscopic methods in multivariate analyses assessing other long-term postoperative genitourinary and/or infertility outcomes.
Conclusion
We found no differences in postoperative genital prolapse or other complications related to gynecology, urology, and/or infertility between open anterior and laparoscopic groin hernia repair in women. Assuming the round ligament of uterus is being transected more often in laparoscopic repair than in open, the urogenital consequences of transection seem to be minimal.



Similar content being viewed by others
References
Burcharth J, Pedersen M, Bisgaard T, Pedersen C, Rosenberg J (2013) Nationwide prevalence of groin hernia repair. PLoS ONE 8:e54367
Weber A, Valencia S, Garteiz D, Burguess A (2001) Epidemology of Hernias in the Female. In: Bendavid R, Abrahamson J, Arregui ME, Flament JB, Phillips EH (eds) Abdominal Wall Hernias: principles and management. Springer, New York, pp 613–619
Kingsnorth A (2004) Treating inguinal hernias. BMJ 328:59–60
The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165
Nilsson H, Holmberg H, Nordin P (2017) Groin hernia repair in women—a nationwide register study. Am J Surg 216:274–279
Schmidt L, Oberg S, Andresen K, Rosenberg J (2018) Laparoscopic repair is superior to open techniques when treating primary groin hernias in women: a nationwide register-based cohort study. Surg Endosc 33:71–78
Schmidt L, Öberg S, Andresen K, Rosenberg J (2018) Recurrence rates after inguinal hernia repair in women: a systematic review. JAMA Surg 153:1135–1142
Cobb WS (2013) Technique: Laparoscopic TAPP and IPOM. In: Jacob BP, Ramshaw B (eds) The SAGES manual of Hernia repair. Springer, New York, pp 81–89
Yang XF, Liu JL (2016) Laparoscopic repair of inguinal hernia in adults. Ann Transl Med 4:402
Ando H, Kaneko K, Ito F, Seo T, Ito T (1997) Anatomy of the round ligament in female infants and children with an inguinal hernia. Br J Surg 84:404–405
Drake R, Vogl W, Mitchell AWM (2015) Pelvis and perineum. In: Drake R, Vogl W, Mitchell AWM (eds) Gray’s anatomy for students, 3rd edn. Churchill Livingstone, London, pp 421–432
Mahran M, Ghaleb HA (1964) The physiology of the human round ligament. J Obstet Gynaecol Br Commonw 71:374–378
Yen CF, Wang CJ, Lin SL, Lee CL, Soong YK (2002) Combined laparoscopic uterosacral and round ligament procedures for treatment of symptomatic uterine retroversion and mild uterine decensus. J Am Assoc Gynecol Laparosc 9:359–366
Schmidt L, Andresen K, Oberg S, Rosenberg J (2018) Dealing with the round ligament of uterus in laparoscopic groin hernia repair: a nationwide survey among experienced surgeons. Hernia 22:849–855
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, Sorensen HT, von Elm E, Langan SM (2015) The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med 12:e1001885
Friis-Andersen H, Bisgaard T (2016) The Danish inguinal hernia database. Clin Epidemiol 8:521–524
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT (2015) The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 7:449–490
Helweg-Larsen K (2011) The Danish register of causes of death. Scand J Public Health 39:26–29
Kyle-Leinhase I, Kockerling F, Jorgensen LN, Montgomery A, Gillion JF, Rodriguez JAP, Hope W, Muysoms F (2018) Comparison of hernia registries: the CORE project. Hernia 22:561–575
World Health Organisation (WHO) (2016) ICD-10 Version 2016. Available at: http://apps.who.int/classifications/icd10/browse/2016/en. Accessed 11 Feb 2019
The Nordic Medico-Statistical Committee (NOMESCO) (2011) Classification of surgical procedures. Available at: http://norden.diva-portal.org/smash/get/diva2:968721/FULLTEXT01.pdf. November 2011; Accessed 11 Feb 2019
Pedersen CB, Gotzsche H, Moller JO, Mortensen PB (2006) The Danish civil registration system. A cohort of eight million persons. Dan Med Bull 53:441–449
Vergelt TF, Weemhoff M, Inthout J, Kluivers KB (2015) Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J 26:1559–1573
Funding
This study received a Grant from the A.P. Moeller Marsk Foundation (Laegefonden), Grant Number: 18-L-0169.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Ms. Schmidt reports Grants from the A.P. Moeller Foundation (Laegefonden) during the conduct of the study, Grant Number 18-L-0169. Mr. Rosenberg reports personal fees from C.R. Bard, Inc. and Merck & Co., Inc. outside the submitted work. Mr. Andresen have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schmidt, L., Andresen, K. & Rosenberg, J. No difference in genitourinary complications after laparoscopic vs. open groin hernia repair in women: a nationwide linked register-based cohort study. Surg Endosc 34, 1978–1984 (2020). https://doi.org/10.1007/s00464-019-06973-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06973-x