Abstract
Background
Operative skills correlate with patient outcomes, yet at the completion of training or after learning a new procedure, these skills are rarely formally evaluated. There is interest in the use of summative video assessment of laparoscopic benign foregut and hiatal surgery (LFS). If this is to be used to determine competency, it must meet the robust criteria established for high-stakes assessments. The purpose of this review is to identify tools that have been used to assess performance of LFS and evaluate the available validity evidence for each instrument.
Methods
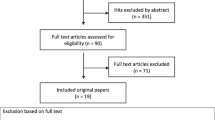
A systematic search was conducted up to July 2017. Eligible studies reported data on tools used to assess performance in the operating room during LFS. Two independent reviewers considered 1084 citations for eligibility. The characteristics and testing conditions of each assessment tool were recorded. Validity evidence was evaluated using five sources of validity (content, response process, internal structure, relationship to other variables, and consequences).
Results
There were six separate tools identified. Two tools were generic to laparoscopy, and four were specific to LFS [two specific to Nissen fundoplication (NF), one heller myotomy (HM), and one paraesophageal hernia repair (PEH)]. Overall, only one assessment was supported by moderate evidence while the others had limited or unknown evidence. Validity evidence was based mainly on internal structure (all tools reporting reliability and item analysis) and content (two studies referencing previous papers for tool development in the context of clinical assessment, and four listing items without specifying the development procedures). There was little or no evidence supporting test response process (one study reporting rater training), relationship to other variables (two comparing scores in subjects with different clinical experience), and consequences (no studies). Two tools were identified to have evidence for video assessment, specific to NF.
Conclusion
There is limited evidence supporting the validity of assessment tools for laparoscopic foregut surgery. This precludes their use for summative video-based assessment to verify competency. Further research is needed to develop an assessment tool designed for this purpose.
Graphical abstract


Similar content being viewed by others
References
Beard JD, Marriott J, Purdie H, Crossley J (2011) Assessing the surgical skills of trainees in the operating theatre: a prospective observational study of the methodology. Health Technol Assess. https://doi.org/10.3310/hta15010
Hamstra SJ, Dubrowski A (2005) Effective training and assessment of surgical skills, and the correlates of performance. Surg Innov 12:71–77
Vassiliou MC, Feldman LS (2011) Objective assessment, selection, and certification in surgery. Surg Oncol 20:140–145
Birkmeyer JD, Finks JF, O’Reilly A, Oerline M, Carlin AM, Nunn AR, Dimick J, Banerjee M, Birkmeyer NJO (2013) Surgical skill and complication rates after bariatric surgery. N Engl J Med 369:1434–1442
Touchie C, Ten Cate O (2016) The promise, perils, problems and progress of competency-based medical education. Med Educ 50(1):93–100
Feldman LS et al (2004) Relationship between objective assessment of technical skills and subjective in-training evaluations in surgical residents. J Am Coll Surg 198:105–110
Larson JL, William RG, Ketchum J, Boehler ML, Dunnington GL (2005) Feasibility, reliability and validity of an operative performance rating system for evaluating surgery residents. Surgery 138:640–649
Streiner DL (1985) Global rating scales. In: Neufeld VR, Norman GR (eds) Assessing clinical competence. Springer, New York, pp 119–141
Mackenzie H, Ni M, Miskovic D, Motson RW, Gudgeon M, Khan Z, Longman R, Coleman MG, Hanna GB (2015) Clinical validity of consultant technical skills assessment in the English National Training Programme for laparoscopic colorectal surgery. Br J Surg 102:991–997
Miskovic D, Wyles SM, Carter F, Coleman MG, Hanna GB (2011) Development, validation and implementation of a monitoring tool for training in laparoscopic colorectal surgery in the English National Training Program. Surg Endosc 25:1136–1142
Madani A, Vassiliou MC, Watanabe Y, Al-Halabi B, Al-Rowais MS, Deckelbaum DL, Fried GM, Feldman LS (2017) What are the principles that guide behaviors in the operating room?: creating a framework to define and measure performance. Ann Surg 265:255–267
Medina M (2001) Formidable challenges to teaching advanced laparoscopic skills. J Soc Laparoendosc Surg 5:153–158
fellowshipcouncil.org
Broeders JAJL, Draaisma WA, Jong HGRd, Smout AJPM, Lanschot JJBv, Broeders IAMJ, Gooszen HG (2011) Impact of surgeon experience on 5-year outcome of laparoscopic Nissen fundoplication. Arch Surg 146:340–346
Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL (2003) Surgeon volume and operative mortality in the United States. N Engl J Med 349:2117–2127
Vassiliou MC, Feldman LS, Andrew CG, Bergman S, Leffondre K, Stanbridge D, Fried GM (2005) A global assessment tool for evaluation of intraoperative laparoscopic skills. Am J Surg 190:107–113
Downing SM (2003) Validity: on the meaningful interpretation of assessment data. Med Educ 37:830–837
Kogan JR, Holmboe ES, Hauer KE (2009) Tools for direct observation and assessment of clinical skills of medical trainees: a systematic review. JAMA 302:1316–1326
Ghaderi I, Manji F, Park YS, Juul D, Ott M, Harris I, Farrell TM (2015) Technical skills assessment toolbox: a review using the unitary framework of validity. Ann Surg 261:251–262
Hogle NJ, Liu Y, Ogden RT, Fowler DL (2014) Evaluation of surgical fellows’ laparoscopic performance using Global Operative Assessment of Laparoscopic Skills (GOALS). Surg Endosc 28:1284–1290
Watanabe Y, Madani A, Ito YM, Bilgic E, McKendy KM, Feldman LS, Fried GM, Vassiliou MC (2016) Psychometric properties of the Global Operative Assessment of Laparoscopic Skills (GOALS) using item response theory. Am J Surg. https://doi.org/10.1016/j.amjsurg.2016.09.050
Bilgic E, Watanabe Y, McKendy K, Munshi A, Ito YM, Fried GM, Feldman LS, Vassiliou MC (2016) Reliable assessment of operative performance. Am J Surg 211:426–430
Ghaderi I, Auvergne L, Park YS, Farrell TM (2015) Quantitative and qualitative analysis of performance during advanced laparoscopic fellowship: a curriculum based on structured assessment and feedback. Am J Surg 209:71–78
Ahlberg G, Kruuna O, Leijonmarck CE, Ovaska J, Rosseland A, Sandbu R, Stromberg C, Arvidsson D (2005) Is the learning curve for laparoscopic fundoplication determined by the teacher or the pupil? Am J Surg 189:184–189
Peyre SE, Peyre CG, Hagen JA, Sullivan ME (2010) Reliability of a procedural checklist as a high-stakes measurement of advanced technical skill. Am J Surg 199:110–114
Awad M, Awad F, Carter F, Jervis B, Buzink S, Foster J, Jakimowicz J, Francis NK (2018) Consensus views on the optimum training curriculum for advanced minimally invasive surgery: a Delphi study. Int J Surg 53:137–142
Funding
Steinberg-Bernstein Centre for Minimally Invasive Surgery and Innovation is funded by an unrestricted educational grant from Medtronic.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Elif Bilgic, Mohammed Al Mahroos, Tara Landry, Gerald M. Fried, Melina C. Vassiliou, Liane S. Feldman have no relevant conflicts of interest or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Search strategy for medline
-
1.
exp Esophageal Diseases/su [Surgery] (33036)
-
2.
exp Esophagus/su [Surgery] (9601)
-
3.
Hernia, Hiatal/su [Surgery] (1903)
-
4.
exp Diverticulum, Esophageal/su [Surgery] (1098)
-
5.
(esophag* or oesophag* or gastro?esophag* or para?esophag*).tw,kf. (167048)
-
6.
Fundoplication/ (4057)
-
7.
fundoplicat*.tw,kf. (5356)
-
8.
(nissen adj3 (operat* or procedure*)).tw,kf. (362)
-
9.
(heller adj3 myotom*).tw,kf. (687)
-
10.
epiphrenic-diverticulectom*.tw,kf. (8)
-
11.
mediastinal-dissect*.tw,kf. (283)
-
12.
or/1-11 (175735)
-
13.
exp Laparoscopy/ (84511)
-
14.
laparoscop*.tw,kf. (107840)
-
15.
13 or 14 (120628)
-
16.
12 and 15 (7394)
-
17.
Clinical Competence/ (80679)
-
18.
(competen* or skill or skills).tw,kf. (235018)
-
19.
17 or 18 (287948)
-
20.
Educational Measurement/ (33649)
-
21.
“Task Performance and Analysis”/ (28752)
-
22.
Checklist/(4544)
-
23.
((operativ* or intraoperativ* or perform*) adj5 (assess* or evaluat* or measur*)).tw,kf. (294777)
-
24.
“Surveys and Questionnaires”/ (386261)
-
25.
ed.fs. (254539)
-
26.
(tool or tools or grade or grading or checklist* or check-list* or questionnaire* or form or rating or score* or scoring or scale or scaling).tw,kf. (2951343)
-
27.
or/20-26 (3530579)
-
28.
19 and 27 (128912)
-
29.
16 and 28 (116)
-
30.
(“24414454” or “20103075” or “18417086”).ui. (3)
-
31.
29 and 30 (3)
-
32.
15 and 28 (2962)
-
33.
(“26679826” or “25454951” or “24414454” or “20103075” or “18417086” or “27776756”).ui. (6)
-
34.
32 and 33 (6)
Rights and permissions
About this article
Cite this article
Bilgic, E., Al Mahroos, M., Landry, T. et al. Assessment of surgical performance of laparoscopic benign hiatal surgery: a systematic review. Surg Endosc 33, 3798–3805 (2019). https://doi.org/10.1007/s00464-019-06662-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06662-9