Abstract
Background
Intestinal metaplasia represents an esophageal mucosal transformation due to uncontrolled gastroesophageal reflux disease. Fundoplication has been shown to lead to regression of disease. Magnetic sphincter augmentation is an alternative to fundoplication that effectively treats reflux disease. Initially, patients with intestinal metaplasia were not considered candidates for device placement, so outcomes in these patients are unknown.
Methods
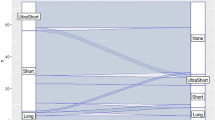
A retrospective review of all patients who underwent magnetic sphincter augmentation device placement between 2007 and 2017 was performed. All patients underwent pre-operative endoscopic evaluation and were categorized as having ultra-short segment (less than 1 cm), short-segment (1–3 cm), or long-segment (greater than or equal to 3 cm) disease. To be included in the study, pathologic examination demonstrating columnar mucosa with goblet cells was required.
Results
There were 86 patients with biopsy-proven non-dysplastic intestinal metaplasia. 35 patients had ultra-short segment, 37 patients had short-segment, and 14 patients had long-segment disease. At a median follow-up of 1.2 years, 67/86 (78%) patients completed endoscopic follow-up. 48/67 (71.6%) patients had regression of intestinal metaplasia. There was no progression to dysplasia or carcinoma. Patients with abnormal post-operative DeMeester scores were less likely to have regression of disease. Regression was more likely in the ultra-short segment (82.8%) and short-segment (73.3%) groups compared to the long-segment group (25.0%).
Conclusions
Magnetic sphincter augmentation is effective in achieving regression of intestinal metaplasia. Longer-term follow-up is needed to assess durability of effect and make meaningful comparisons to fundoplication.
Similar content being viewed by others
References
Oh DS, Demeester SR (2010) Pathophysiology and treatment of Barrett’s esophagus. World J Gastroenterol 16:3762–3772
Zehetner J, DeMeester SR, Ayazi S, Costales JL, Augustin F, Oezcelik A, Lipham JC, Sohn HJ, Hagen JA, DeMeester TR (2010) Long-term follow-up after anti-reflux surgery in patients with Barrett’s esophagus. J Gastrointest Surg 14:1483–1491
Knight BC, Devitt PG, Watson DI, Smith LT, Jamieson GG, Thompson SK (2017) Long-term efficacy of laparoscopic antireflux surgery on regression of Barrett’s esophagus using BRAVO wireless pH monitoring: a prospective clinical cohort study. Ann Surg 266:1000–1005
Ganz RA, Peters JH, Horgan S, Bemelman WA, Dunst CM, Edmundowicz SA, Lipham JC, Luketich JD, Melvin WS, Oelschlager BK, Schlack-Haerer SC, Smith CD, Smith CC, Dunn D, Taiganides PA (2013) Esophageal sphincter device for gastroesophageal reflux disease. N Engl J Med 368:719–727
Saino G, Bonavina L, Lipham JC, Dunn D, Ganz RA (2015) Magnetic sphincter Augmentation for gastroesophageal reflux at 5 years: final results of a pilot study show long-term acid reduction and symptom improvement. J Laparoendosc Adv Surg Tech A 25:787–792
Ganz RA, Edmundowicz SA, Taiganides PA, Lipham JC, Smith CD, DeVault KR, Horgan S, Jacobsen G, Luketich JD, Smith CC, Schlack-Haerer SC, Kothari SN, Dunst CM, Watson TJ, Peters J, Oelschlager BK, Perry KA, Melvin S, Bemelman WA, Smout AJ, Dunn D (2016) Long-term outcomes of patients receiving a magnetic sphincter augmentation device for gastroesophageal reflux. Clin Gastroenterol Hepatol 14:671–677
Rona KA, Reynolds J, Schwameis K, Zehetner J, Samakar K, Oh P, Vong D, Sandhu K, Katkhouda N, Bildzukewicz N, Lipham JC (2017) Efficacy of magnetic sphincter augmentation in patients with large hiatal hernias. Surg Endosc 31:2096–2102
Buckley FP 3rd, Bell RCW, Freeman K, Doggett S, Heidrick R (2018) Favorable results from a prospective evaluation of 200 patients with large hiatal hernias undergoing LINX magnetic sphincter augmentation. Surg Endosc 32:1762–1768
Kuckelman JP, Phillips CJ, Hardin MO, Martin MJ (2017) Standard vs expanded indications for esophageal magnetic sphincter augmentation for reflux disease. JAMA Surg 152:890–891
Stadlhuber RJ, Dubecz A, Meining A, Stein HJ (2015) Adenocarcinoma of the distal esophagus in a patient with a magnetic sphincter augmentation device: first of many to come? Ann Thorac Surg 99:e147–e148
Komanduri S, Kahrilas PJ, Krishnan K, McGorisk T, Bidari K, Grande D, Keefer L, Pandolfino J (2017) Recurrence of Barrett’s esophagus is rare following endoscopic eradication therapy coupled with effective reflux control. Am J Gastroenterol 112:556–566
Rudolph RE, Vaughan TL, Storer BE, Haggitt RC, Rabinovitch PS, Levine DS, Reid BJ (2000) Effect of segment length on risk for neoplastic progression in patients with Barrett esophagus. Ann Intern Med 132:612–620
Gurski RR, Peters JH, Hagen JA, DeMeester SR, Bremner CG, Chandrasoma PT, DeMeester TR (2003) Barrett’s esophagus can and does regress after antireflux surgery: a study of prevalence and predictive features. J Am Coll Surg 196:706–712. (discussion 712–703)
DeMeester SR, Campos GM, DeMeester TR, Bremner CG, Hagen JA, Peters JH, Crookes PF (1998) The impact of an antireflux procedure on intestinal metaplasia of the cardia. Ann Surg 228:547–556
Maret-Ouda J, Konings P, Lagergren J, Brusselaers N (2016) Antireflux surgery and risk of esophageal adenocarcinoma: a systematic review and meta-analysis. Ann Surg 263:251–257
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclousres
Nikolai Bildzukewicz and John C. Lipham—consultant for Torax Medical, Inc. Evan T. Alicuben, James M. Tatum, Kamran Samakar, Jamil S. Samaan, Einav N. Silverstein, Kulmeet Sandhu, and Caitlin C. Houghton have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Alicuben, E.T., Tatum, J.M., Bildzukewicz, N. et al. Regression of intestinal metaplasia following magnetic sphincter augmentation device placement. Surg Endosc 33, 576–579 (2019). https://doi.org/10.1007/s00464-018-6367-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6367-x