Abstract
Introduction
Methods of developing and determining General Surgery (GS) residents’ competency in gastrointestinal endoscopy in Canada are not currently standardized. This study aimed to assess the status of gastrointestinal endoscopy training in Royal College of Physicians and Surgeons of Canada (RCPSC) GS residency programs.
Methods
A 35-question survey was developed using GS gastrointestinal endoscopy curricula guidelines. All 17 RCPSC GS program directors were contacted to complete the questionnaire via the web-based SurveyMonkey.ca® platform.
Results
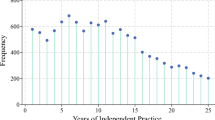
All 17 program directors completed the survey (100% response rate). Program demographics Sixteen programs reported having dedicated endoscopy rotations with a mean duration of 2.8 months (range 0–4, SD 1.1). Upon completion of dedicated endoscopy rotations, four programs (25%) reported having formal skills assessments and three (18.8%) reported formal knowledge examinations. All programs required endoscopy procedures be logged throughout residency, but only three (21.4%) included quality indicators. Only one program required residents to obtain Fundamentals of Endoscopic Surgery certification. Program outcomes The reported estimated mean number of procedures during residents’ endoscopy rotations was 82 (range 10–150, standard deviation 33.6) gastroscopies and 156 (40–350, 76.3) colonoscopies. The mean number of procedures during residents’ entire residencies was 150 (20–400, 98.6) gastroscopies and 241 (50–500, 76.3) colonoscopies. The number of months of dedicated endoscopy training significantly correlated with the total estimated number of endoscopic procedures performed (ρ = 0.67, p = 0.02). Eleven program directors (73.3%) believed residents were prepared for independent endoscopy practice, while four disagreed (26.7%). Program directors’ perceptions of residents’ preparedness were significantly correlated with the number of endoscopic procedures performed by residents (p < 0.01) but not the robustness of the endoscopy curriculum (p = 0.72).
Conclusion
Endoscopy training in RCPSC GS residency programs is highly variable. Program directors’ perceptions of residents’ competency appear to be significantly correlated with procedure numbers and few have adopted formal curricula and performance assessments.
Visual abstract





Similar content being viewed by others
References
Jones DB, Hunter JG, Townsend CM, Minter RM, Roberts PL, Brethauer S, Soper NJ (2017) SAGES rebuttal. Gastrointest Endosc 86:751–753
Asfaha S, Alqahtani S, Hilsden RJ, MacLean AR, Beck PL (2008) Assessment of endoscopic training of general surgery residents in a North American health region. Gastrointest Endosc 68:1056–1062
Ekkelenkamp VE, Koch AD, de Man RA, Kuipers EJ (2016) Training and competence assessment in GI endoscopy: a systematic review. Gut 65:607–615
SAGES – Fundamentals of Endoscopic Surgery. http://www.fesprogram.org/ Accessed 12 Nov 2017
Pearl J, Fellinger E, Dunkin B, Pauli E, Trus T, Marks J, Fanelli R, Meara M, Stefanidis D, Richardson W (2016) Guidelines for privileging and credentialing physicians in gastrointestinal endoscopy. Surg Endosc 30:3184–3190
American Board of Surgery (2016) Booklet of information – surgery. http://www.absurgery.org/xfer/BookletofInfo-Surgery.pdf Accessed 14 Nov 2017
American Board of Surgery (2014) Flexible endoscopy curriculum for general surgery residents. https://www.absurgery.org/xfer/abs-fec.pdf Accessed 1 Mar 2018
Royal College of Physicians (2017) Joint advisory group on GI endoscopy. https://www.thejag.org.uk/CMS/Page.aspx?PageId=65. Accessed 16 Dec 2017
Shahidi N, Ou G, Telford J, Enns R (2014) Establishing the learning curve for achieving competency in performing colonoscopy: a systematic review. Gastrointest Endosc 80:410–416
Forbes N, Mohamed R, Raman M (2016) Learning curve for endoscopy training: is it all about numbers? Best Pract Res Clin Gastroenterol 30:349–356
James PD, Antonova L, Martel M, Barkun A (2016) Measures of trainee performance in advanced endoscopy: a systematic review. Best Pract Res Clin Gastroenterol 30:421–452
Dubé C, Rostom A (2016) Acquiring and maintaining competency in gastrointestinal endoscopy. Best Pract Res Clin Gastroenterol 30:339–347
Bradley NL, Bazzerelli A, Lim J, Ying VWC, Steigerwald S, Strickland M (2015) Endoscopy training in Canadian general surgery residency programs. Can J Surg 58:150–152
Reid S, George R, Warnock GL, Jamieson CG, Olson D, Buie D, Bohnen J, Lidington J (2011) Canadian Association of General Surgeons statement on endoscopy. Can J Surg 54:295
Fowler FJ (2009) Survey research methods, 4th edn. Thousand Oaks SAGES Publishing Inc., London
Surgical Council on Resident Education. SCORE General Surgery Resident Curriculum Portal. http://www.surgicalcore.org/. Accessed 28 Dec 2017
Pace D, Borgaonkar M (2015) Endoscopy training in Canada in general surgery residency programs: ways forward. Can J Surg 58:E5–E6
American Board of Surgery (2011) ABS statement on GI endoscopy. http://www.absurgery.org/default.jsp?newsgiresponse. Accessed 17 Dec 2017
Hazey JW, Marks JM, Mellinger JD, Trus TL, Chand B, Delaney CP, Dunkin BJ, Fanelli RD, Fried GM, Martinez JM, Pearl JP, Poulose BK, Sillin LF, Vassiliou MC, Melvin WS (2014) Why fundamentals of endoscopic surgery (FES)? Surg Endosc 28:701–703
Vassiliou MC, Kaneva PA, Poulose BK, Dunkin BJ, Marks JM, Sadik R, Sroka G, Anvari M, Thaler K, Adrales GL, Hazey JW, Lightdale JR, Velanovich V, Swanstrom LL, Mellinger JD, Fried GM (2010) Global Assessment of Gastrointestinal Endoscopic Skills (GAGES): a valid measurement tool for technical skills in flexible endoscopy. Surg Endosc 24:1834–1841
ACGME (2017) Program requirements for graduate medical education in general surgery. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/440_general_surgery_2017-07-01.pdf. Accessed 16 Dec 2017
Bittner JG, Marks JM, Dunkin BJ, Richards WO, Onders RP, Mellinger JD (2007) Resident training in flexible gastrointestinal endoscopy: a review of current issues and options. J Surg Educ 64:399–409
Edelman D, Mattos M, Bouwman DL (2011) Impact of fundamentals of laparoscopic surgery training during medical school on performance by first year surgical residents. J Surg Res 170:6–9
Sroka G, Feldman LS, Vassiliou MC, Kaneva PA, Fayez R, Fried GM (2010) Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room-a randomized controlled trial. Am J Surg 199:115–120
Derevianko AY, Schwaitzberg SD, Tsuda S, Barrios L, Brooks DC, Callery MP, Fobert D, Irias N, Rattner DW, Jones DB (2010) Malpractice carrier underwrites fundamentals of laparoscopic surgery training and testing: a benchmark for patient safety. Surg Endosc 24:616–623
Jin CJ, Martimianakis MA, Kitto S, Moulton CA (2012) Pressures to “measure up” in surgery: managing your image and managing your patient. Ann Surg 256:989–993
Drolet BC, Sangisetty S, Tracy TF, Cioffi WG (2013) Surgical residents’ perceptions of 2011 Accreditation Council for Graduate Medical Education duty hour regulations. JAMA Surg 148:427
Ferguson CM (2015) General surgery residency inadequately prepares trainees for fellowship. Ann Surg 261(1):e6
Yamamoto S, Uedo N, Ishihara R, Kajimoto N, Ogiyama H, Fukushima Y, Yamamoto S, Takeuchi Y, Higashino K, Lishi H, Tatsuta M (2009) Endoscopic submucosal dissection for early gastric cancer performed by supervised residents: assessment of feasibility and learning curve. Endoscopy 41:923–928
Subhas G, Gupta A, Mittal VK (2010) Necessity for improvement in endoscopy training during surgical residency. Am J Surg 199:331–335
Fonseca AL, Reddy V, Yoo PS, Gusberg RJ, Longo WE (2016) Senior surgical resident confidence in performing flexible endoscopy: what can we do differently? J Surg Educ 73:311–316
Morales MP, Mancini GJ, Miedema BW, Rangnekar NJ, Koivunen DG, Ramshaw DJ, Eubanks WS, Stephenson HE (2008) Integrated flexible endoscopy training during surgical residency. Surg Endosc 22:2013–2017
Hawkins RE, Welcher CM, Holmboe ES, Kirk LM, Simos KB, Skochelak SE (2015) Implementation of competency-based medical education: are we addressing the concerns and challenges? Med Educ 49:1086–1102
Ross M (2015) Entrustable professional activities. Clin Teach 12:223–225
Ten Cate O (2013) Competency-based education, entrustable professional activities, and the power of language. J Grad Med Educ 5:6–7
Moore D, Young CJ, Hong J (2017) Implementing entrustable professional activities: the yellow brick road towards competency-based training? ANZ J Surg 87:1001–1005
Dath D, Iobst W (2010) The importance of faculty development in the transition to competency-based medical education. Med Teach 32:683–686
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Delisle, Chernos, Park, Hardy, and Vergis have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Delisle, M., Chernos, C., Park, J. et al. Canadian general surgery residents’ need formal curricula and objective performance assessments in gastrointestinal endoscopy training: a program director census. Surg Endosc 32, 5012–5020 (2018). https://doi.org/10.1007/s00464-018-6364-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6364-0