Abstract
Background
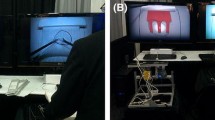
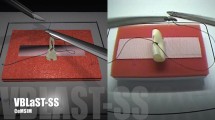
Mastery of laparoscopic skills is essential in surgical practice and requires considerable time and effort to achieve. The Virtual Basic Laparoscopic Skill Trainer (VBLaST-PC©) is a virtual simulator that was developed as a computerized version of the pattern cutting (PC) task in the Fundamentals of Laparoscopic Surgery (FLS) system. To establish convergent validity for the VBLaST-PC©, we assessed trainees’ learning curves using the cumulative summation (CUSUM) method and compared them with those on the FLS.
Methods
Twenty-four medical students were randomly assigned to an FLS training group, a VBLaST training group, or a control group. Fifteen training sessions, 30 min in duration per session per day, were conducted over 3 weeks. All subjects completed pretest, posttest, and retention test (2 weeks after posttest) on both the FLS and VBLaST© simulators. Performance data, including time, error, FLS score, learning rate, learning plateau, and CUSUM score, were analyzed.
Results
The learning curve for all trained subjects demonstrated increasing performance and a performance plateau. CUSUM analyses showed that five of the seven subjects reached the intermediate proficiency level but none reached the expert proficiency level after 150 practice trials. Performance was significantly improved after simulation training, but only in the assigned simulator. No significant decay of skills after 2 weeks of disuse was observed. Control subjects did not show any learning on the FLS simulator, but improved continually in the VBLaST simulator.
Conclusions
Although VBLaST©- and FLS-trained subjects demonstrated similar learning rates and plateaus, the majority of subjects required more than 150 trials to achieve proficiency. Trained subjects demonstrated improved performance in only the assigned simulator, indicating specificity of training. The virtual simulator may provide better opportunities for learning, especially with limited training exposure.








Similar content being viewed by others
References
Dawson SL, Kaufman JA (1998) The imperative for medical simulation. In: Proceedings of the IEEE, pp 479–483
Cao CGL, MacKenzie C, Payandeh S (1996) Task and motion analyses in endoscopic surgery. In: Proceedings ASME Dynamic Systems and Control Division (Fifth Annual Symposium on Haptic Interfaces for Virtual Environment and Teleoperator Systems), pp 583–590
Fried GM (2008) FLS assessment of competency using simulated laparoscopic tasks. J Gastrointest Surg 12(2):210–212
Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B et al (2004) Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 135(1):21–27. http://www.ncbi.nlm.nih.gov/pubmed/14694297
Fraser SA, Klassen DR, Feldman LS, Ghitulescu GA, Stanbridge D, Fried GM (2003) Evaluating laparoscopic skills, setting the pass/fail score for the MISTELS system. Surg Endosc Other Interv Tech 17(6):964–967
Arikatla VS, Sankaranarayanan G, Ahn W, Chellali A, Cao CGL, De S (2013) Development and validation of VBLaST-PT©: a virtual peg transfer simulator. In: Studies in health technology and informatics. IOS Press, Amsterdam, pp. 24–30. http://www.ncbi.nlm.nih.gov/pubmed/23263645
Sankaranarayanan G, Adair JD, Halic T, Gromski MA, Lu Z, Ahn W et al (2011) Validation of a novel laparoscopic adjustable gastric band simulator. Surg Endosc 25(4):1012–1018. http://www.ncbi.nlm.nih.gov/pubmed/20734069
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK et al (2002) Virtual reality training improves operating room performance. Ann Surg 236(4):458–464. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1422600/
Seymour NE (2008) VR to OR: a review of the evidence that virtual reality simulation improves operating room performance. World J Surg 32(2):182–188. http://www.ncbi.nlm.nih.gov/pubmed/18060453
Sankaranarayanan G, Lin H, Arikatla VS, Mulcare M, Zhang L, Derevianko A et al (2010) Preliminary face and construct validation study of a virtual basic laparoscopic skill trainer. J Laparoendosc Adv Surg Tech 20(2):153–157. http://www.liebertonline.com/doi/abs/10.1089/lap.2009.0030
Chellali A, Ahn W, Sankaranarayanan G, Flinn JT, Schwaitzberg SD, Jones DB et al (2015) Preliminary evaluation of the pattern cutting and the ligating loop virtual laparoscopic trainers. Surg Endosc 29(4):815–821. http://www.ncbi.nlm.nih.gov/pubmed/25159626
Arikatla VS, Sankaranarayanan G, Ahn W, Chellali A, De S, Caroline GL et al (2013) Face and construct validation of a virtual peg transfer simulator. Surg Endosc 27(5):1721–1729. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3625247&tool=pmcentrez&rendertype=abstract
Chellali A, Zhang L, Sankaranarayanan G, Arikatla VS, Ahn W, Derevianko A et al (2014) Validation of the VBLaST peg transfer task: a first step toward an alternate training standard. Surg Endosc. http://www.ncbi.nlm.nih.gov/pubmed/24771197
Biau DJ, Resche-Rigon M, Godiris-Petit G, Nizard RS, Porcher R (2007) Quality control of surgical and interventional procedures: a review of the CUSUM. Qual Saf Health Care 16(3):203–207. http://qualitysafety.bmj.com/content/16/3/203
Williams SM, Parry BR, Schlup MM (1992) Quality control: an application of the cusum. Br Med J 304(6838):1359–1361. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1882013/
Feldman LS, Cao J, Andalib A, Fraser S, Fried GM (2009) A method to characterize the learning curve for performance of a fundamental laparoscopic simulator task: defining “learning plateau” and “learning rate”. Surgery 146(2):381–386. http://www.ncbi.nlm.nih.gov/pubmed/19628099
Zhang L, Sankaranarayanan G, Arikatla VS, Ahn W, Grosdemouge C, Rideout JM et al (2013) Characterizing the learning curve of the VBLaST-PT(©) (Virtual Basic Laparoscopic Skill Trainer). Surg Endosc 27(10):3603–3615. http://www.ncbi.nlm.nih.gov/pubmed/23572217
Fraser SA, Bergman S, Garzon J (2012) Laparoscopic splenectomy: learning curve comparison between benign and malignant disease. Surg Innov 19(1):27–32. http://www.ncbi.nlm.nih.gov/pubmed/21719436
Melfi FMA, Mussi A (2008) Robotically assisted lobectomy: learning curve and complications. Thorac Surg Clin 18(3):289–295, vi–vii. http://www.sciencedirect.com/science/article/pii/S1547412708000492
Cook JA, Ramsay CR, Fayers P (2007) Using the literature to quantify the learning curve: a case study. Int J Technol Assess Health Care. 23(2):255–260. http://www.ncbi.nlm.nih.gov/pubmed/17493312
Li JCM, Lo AWI, Hon SSF, Ng SSM, Lee JFY, Leung KL (2012) Institution learning curve of laparoscopic colectomy–a multi-dimensional analysis. Int J Colorectal Dis 27(4):527–533. http://www.ncbi.nlm.nih.gov/pubmed/22124675
Chang L, Satava RM, Pellegrini CA, Sinanan MN (2003) Robotic surgery: identifying the learning curve through objective measurement of skill. Surg Endosc 17(11):1744–1748. http://www.ncbi.nlm.nih.gov/pubmed/12958686
Jaffer U, Cameron AEP (2008) Laparoscopic appendectomy: a junior trainee’s learning curve. J Soc Laparoendosc Surg 12(3):288–291. http://www.ncbi.nlm.nih.gov/pubmed/18765054
Veronesi G (2014) Robotic thoracic surgery technical considerations and learning curve for pulmonary resection. Thorac Surg Clin 24(2):135–141. http://dx.doi.org/10.1016/j.thorsurg.2014.02.009
Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM (2011) Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc 25(3):855–860. http://www.ncbi.nlm.nih.gov/pubmed/20734081
Petersen RH, Hansen HJ (2012) Learning curve associated with VATS lobectomy. Ann Cardiothorac Surg 1(1):47–50
Fraser SA, Feldman LS, Stanbridge D, Fried GM (2005) Characterizing the learning curve for a basic laparoscopic drill. Surg Endosc 19(12):1572–1578. http://www.ncbi.nlm.nih.gov/pubmed/16235127
Son G-M, Kim J-G, Lee J-C, Suh Y-J, Cho H-M, Lee Y-S et al (2010) Multidimensional analysis of the learning curve for laparoscopic rectal cancer surgery. J Laparoendosc Adv Surg Tech 20(7):609–617. http://www.ncbi.nlm.nih.gov/pubmed/20701545
Magill RA (2007) Motor learning and control: concepts and applications, 8th edn. McGraw-Hill, New York. http://www.amazon.com/dp/0073047325
Kinsey SE, Giles FJ, Holton J (1989) Cusum plotting of temperature charts for assessing antimicrobial treatment in neutropenic patients. BMJ 299(6702):775–776
Calsina L, Clará A, Vidal-Barraquer F (2011) The use of the CUSUM chart method for surveillance of learning effects and quality of care in endovascular procedures. Eur J Vasc Endovasc Surg 41(5):679–684. http://www.ncbi.nlm.nih.gov/pubmed/21333562
Okrainec A, Ferri LE, Feldman LS, Fried GM (2011) Defining the learning curve in laparoscopic paraesophageal hernia repair: a CUSUM analysis. Surg Endosc 25(4):1083–1087. http://www.ncbi.nlm.nih.gov/pubmed/20835725
Young A, Miller JP, Azarow K (2005) Establishing learning curves for surgical residents using Cumulative Summation (CUSUM) Analysis. Curr Surg 62(3):330–334. http://www.ncbi.nlm.nih.gov/pubmed/15890218
Van Rij AM, McDonald JR, Pettigrew RA, Putterill MJ, Reddy CK, Wright JJ (1995) Cusum as an aid to early assessment of the surgical trainee. Br J Surg 82(11):1500–1503. http://www.ncbi.nlm.nih.gov/pubmed/8535803
Naik VN, Devito I, Halpern SH (2003) Cusum analysis is a useful tool to assess resident proficiency at insertion of labour epidurals. Can J Anaesth 50(7):694–698. http://www.ncbi.nlm.nih.gov/pubmed/12944444
Bartlett A, Parry B (2001) Cusum analysis of trends in operative selection and conversion rates for laparoscopic cholecystectomy. ANZ J Surg 71(8):453–456. http://www.ncbi.nlm.nih.gov/pubmed/11504287
McCarter FD, Luchette FA, Molloy M, Hurst JM, Davis K, Johannigman JA et al (2000) Institutional and individual learning curves for focused abdominal ultrasound for trauma. Ann Surg 231(5):689–700. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1421056/
Papanna R, Biau DJ, Mann LK, Johnson A, Moise KJ Jr (2011) Use of the Learning Curve–Cumulative Summation test for quantitative and individualized assessment of competency of a surgical procedure in obstetrics and gynecology: fetoscopic laser ablation as a model. Am J Obstet Gynecol 204(3):218.e1–218.e9. http://www.sciencedirect.com/science/article/pii/S0002937810022258
Zhang L, Sankaranarayanan G, Arikatla VS, Ahn W, Grosdemouge C, Rideout JM et al (2013) Characterizing the learning curve of the VBLaST-PT(©) (Virtual Basic Laparoscopic Skill Trainer). Surg Endosc. http://www.ncbi.nlm.nih.gov/pubmed/23572217
Lerch L, Donald JC, Olivotto IA, Lesperance M, van der Westhuizen N, Rusnak C et al (2007) Measuring surgeon performance of sentinel lymph node biopsy in breast cancer treatment by cumulative sum analysis. Am J Surg 193(5):556–560. http://www.sciencedirect.com/science/article/pii/S0002961007000918
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery. Ann Surg 242(1):83–91. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1357708/
Pendlimari R, Holubar SD, Dozois EJ, Larson DW, Pemberton JH, Cima RR (2012) Technical proficiency in hand-assisted laparoscopic colon and rectal surgery: determining how many cases are required to achieve mastery. Arch Surg 147(4):317–322. http://www.ncbi.nlm.nih.gov/pubmed/22184135
Forbes TL, DeRose G, Kribs SW, Harris KA (2004) Cumulative sum failure analysis of the learning curve with endovascular abdominal aortic aneurysm repair. J Vasc Surg 39(1):102–108. http://www.sciencedirect.com/science/article/pii/S0741521403009224
Novotný T, Dvorák M, Staffa R (2011) The learning curve of robot-assisted laparoscopic aortofemoral bypass grafting for aortoiliac occlusive disease. J Vasc Surg 53(2):414–420. http://www.ncbi.nlm.nih.gov/pubmed/21093201
Buchs NC, Pugin F, Bucher P, Hagen ME, Chassot G, Koutny-Fong P et al (2012) Learning curve for robot-assisted Roux-en-Y gastric bypass. Surg Endosc 26(4):1116–1121. http://www.ncbi.nlm.nih.gov/pubmed/22044973
Kye B-H, Kim J-G, Cho H-M, Kim H-J, Suh Y-J, Chun C-S (2011) Learning curves in laparoscopic right-sided colon cancer surgery: a comparison of first-generation colorectal surgeon to advance laparoscopically trained surgeon. J Laparoendosc Adv Surg Tech 21(9):789–796. http://www.ncbi.nlm.nih.gov/pubmed/21854205
Filho DO, Rodrigues G (2002) The construction of learning curves for basic skills in anesthetic procedures: an application for the cumulative sum method. Anesth Analg 95(2):411–416. http://www.anesthesia-analgesia.org/content/95/2/411
Murzi M, Cerillo AG, Bevilacqua S, Gilmanov D, Farneti P, Glauber M (2012) Traversing the learning curve in minimally invasive heart valve surgery: a cumulative analysis of an individual surgeon’s experience with a right minithoracotomy approach for aortic valve replacement. Eur J Cardiothorac Surg 41(6):1242–1246. http://www.ncbi.nlm.nih.gov/pubmed/22232493
Li X, Wang J, Ferguson MK (2014) Competence versus mastery: the time course for developing proficiency in video-assisted thoracoscopic lobectomy. J Thorac Cardiovasc Surg 147(4):1150–1154. 10.1016/j.jtcvs.2013.11.036
Schlup MMT, Williams SM, Barbezat GO (1997) ERCP: a review of technical competency and workload in a small unit. Gastrointest Endosc 46(1):48–52. http://www.sciencedirect.com/science/article/pii/S0016510797702098
Bould MD, Crabtree NA, Naik VN (2009) Assessment of procedural skills in anaesthesia. Br J Anaesth 103(4):472–483. http://bja.oxfordjournals.org/content/103/4/472
Acknowledgements
The authors would like to thank Drs. Scott Epstein, Jesse Rideout, George Perides, and Christopher Awtrey for their assistance with the experimental setup, and Jannine Dewar, Winnie Chen, Yiman Lou, Emily Diller, Nicole Santos, and Jamaya Carter for their assistance in collecting and analyzing the performance data.
Funding
This work was supported by a grant from the National Institutes of Health (NIBIB R01 EB010037-01).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Linsk, Monden, Sankaranarayanan, Ahn, De, and Cao have no conflicts of interest or financial ties to disclose. Dr. Jones is a Consultant for Allurion and The Medical Company. Dr. Schwaitzberg is a Consultant for Covidien, and Great Venture Partner, and has equity interest in Human Extension, Acuity Bio, Arch Therapeutics, and Gordian Medical.
Rights and permissions
About this article
Cite this article
Linsk, A.M., Monden, K.R., Sankaranarayanan, G. et al. Validation of the VBLaST pattern cutting task: a learning curve study. Surg Endosc 32, 1990–2002 (2018). https://doi.org/10.1007/s00464-017-5895-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5895-0