Abstract
Background
Laparoscopic resection (LLR) of colorectal liver metastases (CRLM) located in the posterosuperior liver (segments 4a, 7, and 8) is challenging but has become more practical recently due to progress in operative techniques. We aimed to compare tumor-specific, perioperative, and short-term oncological outcomes after LLR and open liver resection (OLR) for CRLM.
Methods
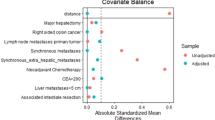
Patients who underwent curative resection of CRLM with at least 1 tumor in the posterosuperior liver during 2012–2015 were analyzed. Tumor-specific factors associated with the adoption of LLR were analyzed by logistic regression model. One-to-one propensity score matching was used to match baseline characteristics between patients with LLR and OLR.
Results
The original cohort included 30 patients with LLR and 239 with OLR. Median follow-up time was 23.8 months. Logistic regression analysis showed that multiple, diameter ≥30 mm, deep location, and closeness to major vessels were associated with OLR. None of the 24 patients with none or one of these factors were converted from LLR to OLR. After matching, 29 patients with LLR and 29 with OLR were analyzed. The 2 groups had similar preoperative factors. The LLR and OLR groups did not differ with respect to operative time, intraoperative bleeding, incidence of blood transfusion, surgical margin positivity, incidence of postoperative complications, and unplanned readmission within 45 days. Median length of postoperative hospital stay was significantly shorter for LLR versus OLR (4 days [1–12] vs. 5 days [4–18]; p = 0.0003). Median recurrence-free survival was similar for patients who underwent LLR versus OLR (10.6 months for LLR vs. 13.4 months for OLR; p = 0.87).
Conclusions
Compared to OLR, LLR of posterosuperior CRLM is associated with significantly shorter postoperative hospital stay but otherwise similar perioperative and short-term oncological outcomes. Tumor-specific factors associated with safe and routine LLR approach despite challenging location are superficial, solitary, and small (<30 mm) CRLM not associated with major vessels.



Similar content being viewed by others
References
Minagawa M, Makuuchi M, Torzilli G, Takayama T, Kawasaki S, Kosuge T, Yamamoto J, Imamura H (2000) Extension of the frontiers of surgical indications in the treatment of liver metastases from colorectal cancer: long-term results. Ann Surg 231(4):487–499
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230(3):309–318 (discussion 318–321)
Adam R, Delvart V, Pascal G, Valeanu A, Castaing D, Azoulay D, Giacchetti S, Paule B, Kunstlinger F, Ghemard O, Levi F, Bismuth H (2004) Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Ann Surg 240(4):644–657 (discussion 657–648)
Andreou A, Aloia TA, Brouquet A, Dickson PV, Zimmitti G, Maru DM, Kopetz S, Loyer EM, Curley SA, Abdalla EK, Vauthey JN (2013) Margin status remains an important determinant of survival after surgical resection of colorectal liver metastases in the era of modern chemotherapy. Ann Surg 257(6):1079–1088. doi:10.1097/SLA.0b013e318283a4d1
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61(2):69–90. doi:10.3322/caac.20107
Azagra JS, Goergen M, Gilbart E, Jacobs D (1996) Laparoscopic anatomical (hepatic) left lateral segmentectomy-technical aspects. Surg Endosc 10(7):758–761
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection-2,804 patients. Ann Surg 250(5):831–841. doi:10.1097/SLA.0b013e3181b0c4df
Rao A, Rao G, Ahmed I (2012) Laparoscopic or open liver resection? Let systematic review decide it. Am J Surg 204(2):222–231. doi:10.1016/j.amjsurg.2011.08.013
Wakabayashi G, Cherqui D, Geller DA, Han HS, Kaneko H, Buell JF (2014) Laparoscopic hepatectomy is theoretically better than open hepatectomy: preparing for the 2nd international consensus conference on laparoscopic liver resection. J Hepatobiliary Pancreat Sci 21(10):723–731. doi:10.1002/jhbp.139
Allard MA, Cunha AS, Gayet B, Adam R, Goere D, Bachellier P, Azoulay D, Ayav A, Navarro F, Pessaux P (2015) Early and long-term oncological outcomes after laparoscopic resection for colorectal liver metastases: a propensity score-based analysis. Ann Surg 262(5):794–802. doi:10.1097/sla.0000000000001475
Beppu T, Wakabayashi G, Hasegawa K, Gotohda N, Mizuguchi T, Takahashi Y, Hirokawa F, Taniai N, Watanabe M, Katou M, Nagano H, Honda G, Baba H, Kokudo N, Konishi M, Hirata K, Yamamoto M, Uchiyama K, Uchida E, Kusachi S, Kubota K, Mori M, Takahashi K, Kikuchi K, Miyata H, Takahara T, Nakamura M, Kaneko H, Yamaue H, Miyazaki M, Takada T (2015) Long-term and perioperative outcomes of laparoscopic versus open liver resection for colorectal liver metastases with propensity score matching: a multi-institutional Japanese study. J Hepatobiliary Pancreat Sci 22(10):711–720. doi:10.1002/jhbp.261
Hasegawa Y, Nitta H, Sasaki A, Takahara T, Itabashi H, Katagiri H, Otsuka K, Nishizuka S, Wakabayashi G (2015) Long-term outcomes of laparoscopic versus open liver resection for liver metastases from colorectal cancer: a comparative analysis of 168 consecutive cases at a single center. Surgery 157(6):1065–1072. doi:10.1016/j.surg.2015.01.017
Cipriani F, Rawashdeh M, Stanton L, Armstrong T, Takhar A, Pearce NW, Primrose J, Abu Hilal M (2016) Propensity score-based analysis of outcomes of laparoscopic versus open liver resection for colorectal metastases. Br J Surg 103(11):1504–1512. doi:10.1002/bjs.10211
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, O’Rourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schon MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J, Strasberg SM (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261(4):619–629. doi:10.1097/sla.0000000000001184
Ishizawa T, Gumbs AA, Kokudo N, Gayet B (2012) Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 256(6):959–964. doi:10.1097/SLA.0b013e31825ffed3
Ban D, Tanabe M, Ito H, Otsuka Y, Nitta H, Abe Y, Hasegawa Y, Katagiri T, Takagi C, Itano O, Kaneko H, Wakabayashi G (2014) A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci 21(10):745–753. doi:10.1002/jhbp.166
Ogiso S, Nomi T, Araki K, Conrad C, Hatano E, Uemoto S, Fuks D, Gayet B (2015) Laparoscopy-specific surgical concepts for hepatectomy based on the laparoscopic caudal view: a key to reboot surgeons’ minds. Ann Surg Oncol 22(Suppl 3):S327–S333. doi:10.1245/s10434-015-4661-6
Lee W, Han HS, Yoon YS, Cho JY, Choi Y, Shin HK (2014) Role of intercostal trocars on laparoscopic liver resection for tumors in segments 7 and 8. J Hepatobiliary Pancreat Sci 21(8):E65–E68. doi:10.1002/jhbp.123
Xiao L, Xiang LJ, Li JW, Chen J, Fan YD, Zheng SG (2015) Laparoscopic versus open liver resection for hepatocellular carcinoma in posterosuperior segments. Surg Endosc 29(10):2994–3001. doi:10.1007/s00464-015-4214-x
Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, Curley SA, Loyer EM, Muratore A, Mentha G, Capussotti L, Vauthey JN (2005) Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg 241(5):715–722 (discussion 722–714)
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Brudvik KW, Mise Y, Conrad C, Zimmitti G, Aloia TA, Vauthey JN (2015) Definition of readmission in 3,041 patients undergoing hepatectomy. J Am Coll Surg 221(1):38–46. doi:10.1016/j.jamcollsurg.2015.01.063
Mise Y, Vauthey JN, Zimmitti G, Parker NH, Conrad C, Aloia TA, Lee JE, Fleming JB, Katz MH (2015) Ninety-day postoperative mortality is a legitimate measure of hepatopancreatobiliary surgical quality. Ann Surg 262(6):1071–1078. doi:10.1097/sla.0000000000001048
Aloia TA, Zorzi D, Abdalla EK, Vauthey JN (2005) Two-surgeon technique for hepatic parenchymal transection of the noncirrhotic liver using saline-linked cautery and ultrasonic dissection. Ann Surg 242(2):172–177
Day RW, Cleeland CS, Wang XS, Fielder S, Calhoun J, Conrad C, Vauthey JN, Gottumukkala V, Aloia TA (2015) Patient-reported outcomes accurately measure the value of an enhanced recovery program in liver surgery. J Am Coll Surg 221 (6):1023–1030. e1021–1022. doi:10.1016/j.jamcollsurg.2015.09.011
Ogiso S, Conrad C, Araki K, Nomi T, Anil Z, Gayet B (2015) Laparoscopic transabdominal with transdiaphragmatic access improves resection of difficult posterosuperior liver lesions. Ann Surg 262(2):358–365. doi:10.1097/sla.0000000000001015
Yamashita S, Loyer E, Kang HC, Aloia TA, Chun YS, Mehran RJ, Eng C, Lee JE, Vauthey JN, Conrad C (2016) Total transthoracic approach facilitates laparoscopic hepatic resection in patients with significant prior abdominal surgery. Ann Surg Oncol. doi:10.1245/s10434-016-5685-2
Schiffman SC, Kim KH, Tsung A, Marsh JW, Geller DA (2015) Laparoscopic versus open liver resection for metastatic colorectal cancer: a metaanalysis of 610 patients. Surgery 157(2):211–222. doi:10.1016/j.surg.2014.08.036
Lewin JW, O’Rourke NA, Chiow AK, Bryant R, Martin I, Nathanson LK, Cavallucci DJ (2016) Long-term survival in laparoscopic vs open resection for colorectal liver metastases: inverse probability of treatment weighting using propensity scores. HPB (Oxford) 18(2):183–191. doi:10.1016/j.hpb.2015.08.001
Xiang L, Xiao L, Li J, Chen J, Fan Y, Zheng S (2015) Safety and feasibility of laparoscopic hepatectomy for hepatocellular carcinoma in the posterosuperior liver segments. World J Surg 39(5):1202–1209. doi:10.1007/s00268-015-2946-3
Lee W, Han HS, Yoon YS, Cho JY, Choi Y, Shin HK, Jang JY, Choi H, Jang JS, Kwon SU (2016) Comparison of laparoscopic liver resection for hepatocellular carcinoma located in the posterosuperior segments or anterolateral segments: a case-matched analysis. Surgery 160(5):1219–1226. doi:10.1016/j.surg.2016.05.009
Chiow AK, Lewin J, Manoharan B, Cavallucci D, Bryant R, O’Rourke N (2015) Intercostal and transthoracic trocars enable easier laparoscopic resection of dome liver lesions. HPB (Oxford) 17(4):299–303. doi:10.1111/hpb.12336
Ichida H, Ishizawa T, Tanaka M, Terasawa M, Watanabe G, Takeda Y, Matsuki R, Matsumura M, Hata T, Mise Y, Inoue Y, Takahashi Y, Saiura A (2016) Use of intercostal trocars for laparoscopic resection of subphrenic hepatic tumors. Surg Endosc. doi:10.1007/s00464-016-5107-3
Pessaux P, van den Broek MA, Wu T, Olde Damink SW, Piardi T, Dejong CH, Ntourakis D, van Dam RM (2013) Identification and validation of risk factors for postoperative infectious complications following hepatectomy. J Gastrointest Surg 17(11):1907–1916. doi:10.1007/s11605-013-2226-1
Uchiyama H, Harimoto N, Itoh S, Yoshizumi T, Ikegami T, Maehara Y (2016) Pleural effusion after hepatectomy for hepatocellular carcinoma: risk factor analyses and its impact on oncological outcomes. World J Surg. doi:10.1007/s00268-016-3826-1
Hallet J, Sa Cunha A, Adam R, Goere D, Bachellier P, Azoulay D, Ayav A, Gregoire E, Navarro F, Pessaux P (2016) Factors influencing recurrence following initial hepatectomy for colorectal liver metastases. Br J Surg 103(10):1366–1376. doi:10.1002/bjs.10191
Acknowledgements
The University of Texas MD Anderson Cancer Center is supported in part by the NIH/NCI under Award Number P30CA016672.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Masayuki Okuno, Claire Goumard, Takashi Mizuno, Kiyohiko Omichi, Ching-Wei D. Tzeng, Yun Shin Chun, Thomas A. Aloia, Jason B. Fleming, Jeffrey E. Lee, Jean-Nicolas Vauthey, and Claudius Conrad have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Okuno, M., Goumard, C., Mizuno, T. et al. Operative and short-term oncologic outcomes of laparoscopic versus open liver resection for colorectal liver metastases located in the posterosuperior liver: a propensity score matching analysis. Surg Endosc 32, 1776–1786 (2018). https://doi.org/10.1007/s00464-017-5861-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5861-x