Abstract
Background
Single-incision laparoscopic surgery (SILS) is a new technique that aims to minimize abdominal wall trauma and improve cosmesis. Concerns have been raised about the risk of trocar-site hernia following SILS. This study aims to assess the risk of trocar-site hernia following SILS compared to conventional laparoscopic surgery, and investigate whether current evidence is conclusive.
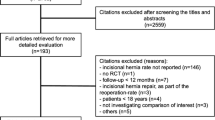
Methods
We performed a systematic search of MEDLINE, AMED, CINAHL, CENTRAL, and OpenGrey. We considered randomized clinical trials comparing the risk of trocar-site hernia with SILS and conventional laparoscopic surgery. Pooled odds ratios with 95% confidence intervals (CI) were calculated using the Mantel–Haenszel method. Trial sequential analysis using the Land and DeMets method was performed to assess the possibility of type I error and compute the information size.
Results
Twenty-three articles reporting a total of 2471 patients were included. SILS was associated with higher odds of trocar-site hernia compared to conventional laparoscopic surgery (odds ratio 2.37, 95% CI 1.25–4.50, p = 0.008). There was no evidence of between-study heterogeneity or small-study effects. The information size was calculated at 1687 patients and the Z-curve crossed the O’Brien–Fleming α-spending boundaries at 1137 patients, suggesting that the evidence of higher risk of trocar-site hernia with SILS compared to conventional laparoscopic surgery can be considered conclusive.
Conclusions
Single-incision laparoscopic procedures through the umbilicus are associated with a higher risk of trocar-site hernia compared to conventional laparoscopic surgery.





Similar content being viewed by others
References
Antoniou SA, Antoniou GA, Antoniou AI, Granderath FA (2015) Past, present, and future of minimally invasive abdominal surgery. JSLS 19(3):e2015.00052
Antoniou SA, Pointner R, Granderath FA (2011) Single-incision laparoscopic cholecystectomy: a systematic review. Surg Endosc 25:367–377
Antoniou SA, Morales-Conde S, Antoniou GA, Pointner R, Granderath FA (2016) Single-incision laparoscopic cholecystectomy with curved versus linear instruments assessed by systematic review and network meta-analysis of randomized trials. Surg Endosc 30:819–831
Milas M, Deveđija S, Trkulja V (2014) Single incision versus standard multiport laparoscopic cholecystectomy: up-dated systematic review and meta-analysis of randomized trials. Surgeon 12:271–289
Aly OE, Black DH, Rehman H, Ahmed I (2016) Single incision laparoscopic appendicectomy versus conventional three-port laparoscopic appendicectomy: a systematic review and meta-analysis. Int J Surg 35:120–128
Julliard O, Hauters P, Possoz J, Malvaux P, Landenne J, Gherardi D (2016) Incisional hernia after single-incision laparoscopic cholecystectomy: incidence and predictive factors. Surg Endosc 30:4539–4543
Agaba EA, Rainville H, Ikedilo O, Vemulapali P (2014) Incidence of port-site incisional hernia after single-incision laparoscopic surgery. JSLS 18:204–210
Tranchart H, Ketoff S, Lainas P, Pourcher G, Di Giuro G, Tzanis D, Ferretti S, Dautruche A, Devaquet N, Dagher I (2013) Single incision laparoscopic cholecystectomy: for what benefit? HPB (Oxford) 15:433–438
Buckley FP 3rd, Vassaur HE, Jupiter DC, Crosby JH, Wheeless CJ, Vassaur JL (2016) Influencing factors for port-site hernias after single-incision laparoscopy. Hernia 20:729–733
Itatsu K, Yokoyama Y, Sugawara G, Kubota H, Tojima Y, Kurumiya Y, Kono H, Yamamoto H, Ando M, Nagino M (2014) Incidence of and risk factors for incisional hernia after abdominal surgery. Br J Surg 101:1439–1447
Nakayama M, Yoshimatsu K, Yokomizo H, Yano Y, Okayama S, Satake M, Matsumoto A, Fujimoto T, Usui T, Yamaguchi K, Shiozawa S, Shimakawa T, Katsube T, Naritaka Y (2014) Incidence and risk factors for incisional hernia after open surgery for colorectal cancer. Hepatogastroenterology 61:1220–1223
Goodenough CJ, Ko TC, Kao LS, Nguyen MT, Holihan JL, Alawadi Z, Nguyen DH, Flores JR, Arita NT, Roth JS, Liang MK (2015) Development and validation of a risk stratification score for ventral incisional hernia after abdominal surgery: hernia expectation rates in intra-abdominal surgery (the HERNIA Project). J Am Coll Surg 220:405–413
Comajuncosas J, Hermoso J, Gris P, Jimeno J, Orbeal R, Vallverdú H, López Negre JL, Urgellés J, Estalella L, Parés D (2014) Risk factors for umbilical trocar site incisional hernia in laparoscopic cholecystectomy: a prospective 3-year follow-up study. Am J Surg 207:1–6
Antoniou SA, Morales-Conde S, Antoniou GA, Granderath FA, Berrevoet F, Muysoms FE; Bonham Group (2016) Single-incision laparoscopic surgery through the umbilicus is associated with a higher incidence of trocar-site hernia than conventional laparoscopy: a meta-analysis of randomized controlled trials. Hernia 20:1–10
Wetterslev J, Thorlund K, Brok J, Gluud C (2008) Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol 61:64–75
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151:W65–W94
SIGN Methodology Checklist 2: Controlled Trials. http://www.sign.ac.uk/methodology/checklists/20121206_Checklist_for_controlled_trials.doc. Accessed 12 April 2014
Higgins JP, Altman DG (2009) Assessing risk of bias in included studies. In: Higgins JP, Green S (eds) Cochrane handbook for systematic reviews of interventions. Wiley, West Sussex, pp 187–235
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ; GRADE Working Group (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926
DeMets D, Lan KK (1994) Interim analysis: the alpha spending function approach. Stat Med 12:1341–1352
O’Brien PC, Fleming TR (1979) A multiple testing procedure for clinical trials. Biometrics 35:549–556
Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P (2011) Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg 98:1695–1702
Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S (2011) Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg 254:22–27
Herrero Fonollosa E, Cugat Andorrà E, García Domingo MI, Camps Lasa J, Porta Castejón R, Carvajal López F, Rodríguez Campos A (2012) A randomised prospective comparative study between laparoscopic cholecystectomy and single port cholecystectomy in a major outpatient surgery unit. Cir Esp 90:641–646
Leung D, Yetasook AK, Carbray J, Butt Z, Hoeger Y, Denham W, Barrera E, Ujiki MB (2012) Single-incision surgery has higher cost with equivalent pain and quality-of-life scores compared with multiple-incision laparoscopic cholecystectomy: a prospective randomized blinded comparison. J Am Coll Surg 215:702–708
Noguera JF, Cuadrado A, Dolz C, Olea JM, García JC (2012) Prospective randomized clinical trial comparing laparoscopic cholecystectomy and hybrid natural orifice transluminal endoscopic surgery (NOTES) (NCT00835250). Surg Endosc 26:3435–3441
Sinan H, Demirbas S, Ozer MT, Sucullu I, Akyol M (2012) Single-incision laparoscopic cholecystectomy versus laparoscopic cholecystectomy: a prospective randomized study. Surg Laparosc Endosc Percutan Tech 22:12–16
Solomon D, Shariff AH, Silasi DA, Duffy AJ, Bell RL, Roberts KE (2012) Transvaginal cholecystectomy versus single-incision laparoscopic cholecystectomy versus four-port laparoscopic cholecystectomy: a prospective cohort study. Surg Endosc 26:2823–2827
Vilallonga R, Barbaros U, Sümer A, Demirel T, Fort JM, González O, Rodriguez N, Carrasco MA (2012) Single-port transumbilical laparoscopic cholecystectomy: a prospective randomised comparison of clinical results of 140 cases. J Minim Access Surg 8:74–78
Zheng M, Qin M, Zhao H (2012) Laparoendoscopic single-site cholecystectomy: a randomized controlled study. Minim Invasive Ther Allied Technol 21:113–117
Abd Ellatif ME, Askar WA, Abbas AE, Noaman N, Negm A, El-Morsy G, El Nakeeb A, Magdy A, Amin M (2013) Quality-of-life measures after single-access versus conventional laparoscopic cholecystectomy: a prospective randomized study. Surg Endosc 27:1896–1906
Khorgami Z, Shoar S, Anbara T, Soroush A, Nasiri S, Movafegh A, Aminian A (2014) A randomized clinical trial comparing 4-port, 3-port, and single-incision laparoscopic cholecystectomy. J Invest Surg 27:147–154
Madureira FA, Manso JE, Madureira Fo D, Iglesias AC (2013) Randomized clinical study for assessment of incision characteristics and pain associated with LESS versus laparoscopic cholecystectomy. Surg Endosc 27:1009–1115
Marks JM, Phillips MS, Tacchino R, Roberts K, Onders R, DeNoto G, Gecelter G, Rubach E, Rivas H, Islam A, Soper N, Paraskeva P, Rosemurgy A, Ross S, Shah S (2013) Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single-blinded trial of traditional multiport laparoscopic cholecystectomy vs single-incision laparoscopic cholecystectomy. J Am Coll Surg 216:1037–1047 (discussion 1047-1048)
Noguera J, Tejada S, Tortajada C, Sánchez A, Muñoz J (2013) Prospective, randomized clinical trial comparing the use of a single-port device with that of a flexible endoscope with no other device for transumbilical cholecystectomy: LLATZER-FSIS pilot study. Surg Endosc 27:4284–4290
Saad S, Strassel V, Sauerland S (2013) Randomized clinical trial of single-port, minilaparoscopic and conventional laparoscopic cholecystectomy. Br J Surg 100:339–349
Zapf M, Yetasook A, Leung D, Salabat R, Denham W, Barrera E, Butt Z, Carbray J, Du H, Wang CE, Ujiki M (2013) Single-incision results in similar pain and quality of life scores compared with multi-incision laparoscopic cholecystectomy: a blinded prospective randomized trial of 100 patients. Surgery 154:662–670 (discussion 670-671)
Carter JT, Kaplan JA, Nguyen JN, Lin MY, Rogers SJ, Harris HW (2014) A prospective, randomized controlled trial of single-incision laparoscopic vs conventional 3-port laparoscopic appendectomy for treatment of acute appendicitis. J Am Coll Surg 218:950–959
Jørgensen LN, Rosenberg J, Al-Tayar H, Assaadzadeh S, Helgstrand F, Bisgaard T (2014) Randomized clinical trial of single- versus multi-incision laparoscopic cholecystectomy. Br J Surg 101:347–355
Villalobos Mori R, Escoll Rufino J, Herrerías González F, Mias Carballal MC, Escartin Arias A, Olsina Kissler JJ (2014) Prospective, randomized comparative study between single-port laparoscopic appendectomy and conventional laparoscopic appendectomy. Chir Esp 92:472–477
Bingener J, Skaran P, McConico A, Novotny P, Wettstein P, Sletten DM, Park M, Low P, Sloan J (2015) A double-blinded randomized trial to compare the effectiveness of minimally invasive procedures using patient-reported outcomes. J Am Coll Surg 221:111–121
Sulu B, Yildiz BD, Ilingi ED, Gunerhan Y, Cakmur H, Anuk T, Yildiz B, Koksal N (2015) Single port vs. four port cholecystectomy-randomized trial on quality of life. Adv Clin Exp Med 24:469–473
Aktimur R, Güzel K, Çetinkünar S, Yıldırım K, Çolak E (2016) Prospective randomized comparison of single-incision laparoscopic cholecystectomy with new facilitating maneuver vs. conventional four-port laparoscopic cholecystectomy. Ulus Cerrahi Derg 32:23–29
Arezzo A, Passera R, Bullano A, Mintz Y, Kedar A, Boni L, Cassinotti E, Rosati R, Fumagalli Romario U, Sorrentino M, Brizzolari M, Di Lorenzo N, Gaspari AL, Andreone D, De Stefani E, Navarra G, Lazzara S, Degiuli M, Shishin K, Khatkov I, Kazakov I, Schrittwieser R, Carus T, Corradi A, Sitzman G, Lacy A, Uranues S, Szold A, Morino M (2016) Multi-port versus single-port cholecystectomy: results of a multi-centre, randomised controlled trial (MUSIC trial). Surg Endosc. doi:10.1007/s00464-016-5298-7
Clark LH, Soliman PT, Odetto D, Munsell MF, Schmeler KM, Fleming N, Westin SN, Nick AM, Ramirez PT (2013) Incidence of trocar site herniation following robotic gynecologic surgery. Gynecol Oncol 131:400–403
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Stavros A. Antoniou and Filip E. Muysoms were members of the Guidelines Committee of the European Hernia Society on the Closure of Abdominal Wall Incisions. They have no other conflicts of interest or financial ties to disclose. Josep M García-Alamino, Shahab Hajibandeh, Shahin Hajibandeh, Michael Weitzendorfer, Frank A. Granderath, George E. Chalkiadakis, Klaus Emmanuel, George A. Antoniou, Meropi Gioumidou, Styliani Iliopoulou-Kosmadaki, Maria Mathioudaki and Kyriakos Souliotis have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Antoniou, S.A., García-Alamino, J.M., Hajibandeh, S. et al. Single-incision surgery trocar-site hernia: an updated systematic review meta-analysis with trial sequential analysis by the Minimally Invasive Surgery Synthesis of Interventions Outcomes Network (MISSION). Surg Endosc 32, 14–23 (2018). https://doi.org/10.1007/s00464-017-5717-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5717-4