Abstract
Background
Achalasia is a rare motility disorder of the esophagus. Treatment is palliative with the goal of symptom remission and slowing the progression of the disease. Treatment options include per oral endoscopic myotomy (POEM), laparoscopic Heller myotomy (LM) and endoscopic treatments such as pneumatic dilation (PD) and botulinum toxin type A injections (BI). We evaluate the economics and cost-effectiveness of treating achalasia.
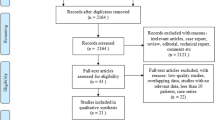
Methods
We performed cost analysis for POEM, LM, PD and BI at our institution from 2011 to 2015. Cost of LM was set to 1, and other procedures are presented as percentage change. Cost-effectiveness was calculated based on cost, number of interventions required for optimal results for dilations and injections and efficacy reported in the current literature. Incremental cost-effectiveness ratio was calculated by a cost-utility analysis using quality-adjusted life year gained, defined as a symptom-free year in a patient with achalasia.
Results
Average number of interventions required was 2.3 dilations or two injections for efficacies of 80 and 61 %, respectively. POEM cost 1.058 times the cost of LM, and PD and BI cost 0.559 and 0.448 times the cost of LM. Annual cost per cure over a period of 4 years for POEM, and LM were consistently equivalent, trending the same as PD although this has a lower initial cost. The cost per cure of BI remains stable over 3 years and then doubles.
Conclusion
The cost-effectiveness of POEM and LM is equivalent. Myotomy, either surgical or endoscopic, is more cost-effective than BI due to high failure rates of the economical intervention. When treatment is being considered BI should be utilized in patients with less than 2-year life expectancy. Pneumatic dilations are cost-effective and are an acceptable approach to treatment of achalasia, although myotomy has a lower relapse rate and is cost-effective compared to PD after 2 years.



Similar content being viewed by others
Notes
Outliers were visits that included prolonged inpatient stays unrelated to the procedure in question, i.e.,: a patient received BI during an unrelated ICU stay.
References
Mayberry JF (2001) Epidemiology and demographics of achalasia. Gastrointest Endosc Clin N Am 11:235–248
Boeckxstaens GE (2005) The lower oesophageal sphincter. Neurogastroenterol Motil 17(Suppl 1):13–21. doi:10.1111/j.1365-2982.2005.00661.x
Storch WB, Eckardt VF, Wienbeck M, Eberl T, Auer PG, Hecker A et al (1995) Autoantibodies to Auerbach’s plexus in achalasia. Cell Mol Biol (Noisy-Le-Grand) 41:1033–1038
Boeckxstaens GE (2008) Achalasia: virus-induced euthanasia of neurons? Am J Gastroenterol 103:1610–1612. doi:10.1111/j.1572-0241.2008.01967.x
Boeckxstaens GE, Zaninotto G, Richter JE (2014) Achalasia. Lancet 383:83–93. doi:10.1016/S0140-6736(13)60651-0
Molena D, Yang SC (2012) Surgical management of end-stage achalasia. Semin Thorac Cardiovasc Surg 24:19–26. doi:10.1053/j.semtcvs.2012.01.015
Richter JE (2010) Achalasia—an update. J Neurogastroenterol Motil 16:232–242. doi:10.5056/jnm.2010.16.3.232
Leyden JE, Moss AC, MacMathuna P (2009) Endoscopic pneumatic dilation versus botulinum toxin injection in the management of primary achalasia. Cochrane Database Syst Rev. doi:10.1002/14651858.CD005046.pub2
Annese V, Bassotti G, Coccia G, Dinelli M, D’Onofrio V, Gatto G et al (2000) A multicentre randomised study of intrasphincteric botulinum toxin in patients with oesophageal achalasia. GISMAD achalasia study group. Gut 46:597–600. doi:10.1136/gut.46.5.597
Zaninotto G, Annese V, Costantini M, Del Genio A, Costantino M, Epifani M et al (2004) Randomized controlled trial of botulinum toxin versus laparoscopic Heller myotomy for esophageal achalasia. Ann Surg 239:364–370. doi:10.1097/01.sla.0000114217.52941.c5
Allescher HD, Storr M, Seige M, Gonzales-Donoso R, Ott R, Born P et al (2001) Treatment of achalasia: Botulinum toxin injection vs. pneumatic balloon dilation. A prospective study with long-term follow-up. Endoscopy 33:1007–1017. doi:10.1055/s-2001-18935
Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A et al (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364:1807–1816. doi:10.1056/NEJMoa1010502
Katsinelos P, Kountouras J, Paroutoglou G, Beltsis A, Zavos C, Papaziogas B et al (2005) Long-term results of pneumatic dilation for achalasia: a 15 years’ experience. World J Gastroenterol 11:5701–5705
Zerbib F, Thétiot V, Richy F, Benajah DA, Message L, Lamouliatte H (2006) Repeated pneumatic dilations as long-term maintenance therapy for esophageal achalasia. Am J Gastroenterol 101:692–697. doi:10.1111/j.1572-0241.2006.00385.x
Hulselmans M, Vanuytsel T, Degreef T, Sifrim D, Coosemans W, Lerut T et al (2010) Long-term outcome of pneumatic dilation in the treatment of achalasia. Clin Gastroenterol Hepatol 8:30–35. doi:10.1016/j.cgh.2009.09.020
Inoue H, Sato H, Ikeda H, Onimaru M, Sato C, Minami H et al (2015) Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg 221:256–264. doi:10.1016/j.jamcollsurg.2015.03.057
Zhou PH, Li QL, Yao LQ, Xu MD, Chen WF, Cai MY et al (2013) Peroral endoscopic remyotomy for failed Heller myotomy: a prospective single-center study. Endoscopy 45:161–166. doi:10.1055/s-0032-1326203
Hu J-W, Li Q-L, Zhou P-H, Yao L-Q, Xu M-D, Zhang Y-Q et al (2014) Peroral endoscopic myotomy for advanced achalasia with sigmoid-shaped esophagus: long-term outcomes from a prospective, single-center study. Surg Endosc. doi:10.1007/s00464-014-4013-9
Sharata A, Kurian AA, Dunst CM, Bhayani NH, Reavis KM, Swanström LL (2013) Peroral endoscopic myotomy (POEM) is safe and effective in the setting of prior endoscopic intervention. J Gastrointest Surg 17:1188–1192. doi:10.1007/s11605-013-2193-6
Caldaro T, Familiari P, Romeo EF, Gigante G, Marchese M, Contini ACI et al (2015) Treatment of esophageal achalasia in children: today and tomorrow. J Pediatr Surg 50:726–730. doi:10.1016/j.jpedsurg.2015.02.047
Chen WF, Li QL, Zhou PH, Yao LQ, Xu MD, Zhang YQ et al (2013) Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: a prospective, single-center study. Gastrointest Endosc. doi:10.1016/j.gie.2014.06.035
Khashab MA, Messallam AA, Onimaru M, Teitelbaum EN, Ujiki MB, Gitelis ME et al (2015) International multicenter experience with peroral endoscopic myotomy for the treatment of spastic esophageal disorders refractory to medical therapy (with video). Gastrointest Endosc 81:1170–1177. doi:10.1016/j.gie.2014.10.011
Pasricha PJ, Hawarl R, Ahmed I, Chen J, Cotton PB, Hawes RH et al (2007) Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy 39:761–764. doi:10.1055/s-2007-966764
Bechara R, Ikeda H, Inoue H (2015) Peroral endoscopic myotomy: an evolving treatment for achalasia. Nat Rev Gastroenterol Hepatol 12:410–426. doi:10.1038/nrgastro.2015.87
Imperiale TF, O’Connor JB, Vaezi MF, Richter JE (2000) A cost-minimization analysis of alternative treatment strategies for achalasia. Am J Gastroenterol 95:2737–2745. doi:10.1111/j.1572-0241.2000.03181.x
Parkman HP, Reynolds JC, Ouyang A, Rosato EF, Eisenberg JM, Cohen S (1993) Pneumatic dilatation or esophagomyotomy treatment for idiopathic achalasia: clinical outcomes and cost analysis. Dig Dis Sci 38:75–85. doi:10.1007/BF01296777
Panaccione R, Gregor JC, Reynolds RPE, Preiksaitis HG (1999) Intrasphincteric botulinum toxin versus pneumatic dilatation for achalasia: a cost minimization analysis. Gastrointest Endosc 50:492–498. doi:10.1016/S0016-5107(99)70071-4
Ghoshal UC, Aggarwal R, Kumar S, Naik SR (2002) Pneumatic dilation versus intrasphincteric botulinum toxin injection in the treatment of achalasia cardia in India: an economic analysis. Indian J Gastroenterol 21:193–196
O’Connor JB, Singer ME, Imperiale TF, Vaezi MF, Richter JE (2002) The cost-effectiveness of treatment strategies for achalasia. Dig Dis Sci 47:1516–1525. doi:10.1023/A:1015811001267
Neumann PJ, Cohen JT, Weinstein MC (2014) Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med 371:796–797. doi:10.1056/NEJMp1405158
Pandolfino JE, Gawron AJ (2015) Achalasia: a systematic review. JAMA 313:1841–1852. doi:10.1001/jama.2015.2996
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Heidi J. Miller, Ruel Neupane, Mojtaba Fayezizadeh and Arnab Majumder have no conflicts of interest. Jeffrey M. Marks has Consultant for US Endoscopy, GI Supply, Merck, GORE, Apollo Endosurgery, Olympus, Fujifilm.
Rights and permissions
About this article
Cite this article
Miller, H.J., Neupane, R., Fayezizadeh, M. et al. POEM is a cost-effective procedure: cost-utility analysis of endoscopic and surgical treatment options in the management of achalasia. Surg Endosc 31, 1636–1642 (2017). https://doi.org/10.1007/s00464-016-5151-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5151-z