Abstract
Background and aim
Pancreatic pseudocysts (PPC) are a complication that occurs in acute and chronic pancreatitis. They comprise 75 % of cystic lesions of the pancreas. There are scarce data about surgical versus endoscopic treatment on PPC. The aim of this study was to compare both treatment modalities regarding clinical success, complication rate, recurrence, hospital stay and cost.
Methods
Retrospectively, data obtained prospectively from 2000 to 2012 were analyzed. A PPC was defined as a fluid collection in the pancreatic or peripancreatic area that had a well-defined wall and contained no solid debris or recognizable parenchymal necrosis. Clinical success was defined as complete resolution or a decrease in size of the PPC to 2 cm or smaller.
Results
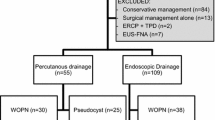
Overall, 64 procedures in 61 patients were included: 21 (33 %) cases were drained endoscopically guided by EUS and 43 (67 %) cases were drained surgically. The clinical success of the endoscopic group was 90.5 versus 90.7 % for the surgical group (P = 0.7), with a complication rate of 23.8 and 25.6 %, respectively (P = 0.8), and a mortality rate of 0 and 2.3 % for each group, respectively (P = 0.4). The hospital stay was lower for the endoscopic group: 0 (0–10) days compared with 7 (2–42) days in the surgical group (P < 0.0001). Likewise, the cost was lower in the endoscopic group (P < 0.001). The recurrence rate was similar in both groups: 9.5 and 4.5 % respectively (P = 0.59). The two recurrences found in the endoscopic group were associated with stent migration, and the recurrence in the surgical group was due to the type of surgery performed (open drainage).
Conclusion
Endoscopic treatment of PPC offers the same clinical success, recurrence, complication and mortality rate as surgical treatment but with a shorter hospital stay and lower costs.
Similar content being viewed by others
References
Bradley EL, Clements JL Jr, Gonzalez AC (1979) The natural history of pancreatic pseudocysts: a unified concept of management. Am J Surg 137:135–141
O’Malley VP, Cannon JP, Postier RG (1985) Pancreatic pseudocysts: cause, therapy, and results. Am J Surg 150:680–682
Aghdassi A, Mayerle J, Kraft M et al (2008) Diagnosis and treatment of pancreatic pseudocysts in chronic pancreatitis. Pancreas 36:105–112
Grace PA, Williamson RC (1993) Modern management of pancreatic pseudocysts. Br J Surg 80:573–581
Wang LW, Li ZS, Li SD et al (2009) Prevalence and clinical features of chronic pancreatitis in China: a retrospective multicenter analysis over 10 years. Pancreas 38:248–254
Andersson B, Nilsson E, Willner J et al (2006) Treatment and outcome in pancreatic pseudocysts. Scand J Gastroenterol 41:751–756
Vitas GJ, Sarr MG (1992) Selected management of pancreatic pseudocysts: operative versus expectant management. Surgery 111:123–130
Yeo CJ, Bastidas JA, Lynch-Nyhan A et al (1990) The natural history of pancreatic pseudocysts documented by computed tomography. Surg Gynecol Obstet 170:411–417
Mehta R, Suvarna D, Sadasivan S et al (2004) Natural course of asymptomatic pancreatic pseudocyst: a prospective study. Indian J Gastroenterol 23:140–142
Andren-Sandberg A, Dervenis C (2004) Pancreatic pseudocysts in the 21st century: Part II. Natural history. JOP 5:64–70
Sandberg AA, Dervenis C (2004) Pancreatic pseudocyst in the 21st century. Part II: natural history. J Pancreas 5:64–70
Bradley EL (2014) The natural and unnatural history of pancreatic fluid collections associated with acute pancreatitis. Dig Dis Sci 59:908–910
Varadarajulu S, Wilcox CM, Latif S et al (2011) Management of pancreatic fluid collections: a changing of the guard from surgery to endoscopy. Am Surg 77:1650–1655
Varadarajulu S, Bang J, Sutton B et al (2013) Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Gastroenterology 145:583–590
Aljarabah M, Ammori BJ (2007) Laparoscopic and endoscopic approaches for drainage of pancreatic pseudocysts: a systematic review of published series. SurgEndosc 21:1936–1944
Johnson MD, Walsh RM, Henderson JM et al (2009) Surgical versus nonsurgical management of pancreatic pseudocysts. J Clin Gastroenterol 43:586–590
Varadarajulu S, Lopes TL, Wilcox CM et al (2008) EUS versus surgical cyst-gastrostomy for management of pancreatic pseudocysts. Gastrointest Endosc 68:649–655
Banks P, Bollen T, Dervenis C et al (2013) Classification of acute pancreatitis 2012: revision of the Atlanta classification and definitions by international consensus. Gut 62:102–111
Varadarajulu S, Christein J, Tamhane A et al (2008) Prospective randomized trial comparing EUS and EGD for transmural drainage of pancreatic pseudocysts (with videos). Gastrointest Endosc 68:1102–1111
Park D, Lee S, Moon S et al (2009) Endoscopic ultrasound-guided versus conventional transmural drainage for pancreatic pseudocysts: a prospective randomized trial. Endoscopy 41:842–848
Varadarajulu S, Noone TC, Tutuian R et al (2005) Predictors of outcome in pancreatic duct disruption managed by endoscopic transpapillary stent. Gastrointest Endosc 61:568–575
Devière J, Antaki F (2008) Disconnected pancreatic tail syndrome: a plea for multidisciplinarity. Gastrointest Endosc 67:680–682
Varadarajulu S, Rana SS, Bhasin DK (2013) Endoscopic therapy for pancreatic duct leaks and disruptions. Gastrointest Endosc Clin N Am 23:863–892
Gibbs C, Baron T (2005) Outcome following endoscopic transmural drainage of pancreatic fluid collections in outpatients. J Clin Gastroenterol 39:634–637
Dávila-Cervantes A, Gómez F, Chan C et al (2004) Laparoscopic drainage of pancreatic pseudocysts. Surg Endosc 18:1420–1426
Lopes CV, Pesenti C, Bories E et al (2008) Endoscopic ultrasound-guided endoscopic transmural drainage of pancreatic pseudocysts. Arq Gastroenterol 45:17–21
Arvanitakis M, Delhaye M, Bali MA et al (2007) Pancreatic-fluid collections: a randomized controlled trial regarding stent removal after endoscopic transmural drainage. Gastrointest Endosc 65:609–619
Krüger M, Scneider AS, Manns MR et al (2006) Endoscopic management of pancreatic pseudocysts or abscess after an EUS-guided 1-step procedure for initial access. Gastrointest Endosc 63:409–416
Bhattacharya D, Ammori BJ (2003) Minimally invasive approaches to the management of pancreatic pseudocysts. Surg Laparosc Endosc Percutan Tech 13:141–148
Rische S, Riecken B, Degenkolb J et al (2013) Transmural endoscopic necrosectomy of infected pancreatic necroses and drainage of infected pseudocysts: a tailored approach. Scand J Gastroenterol 48:231–240
Trevino J, Tamhane A, Varadarajulu S (2010) Successful stenting in ductal disruption favorably impacts treatment outcomes in patients undergoing transmural drainage of peripancreatic fluid collections. J Gastroenterol Hepatol 25:526–531
Varadarajulu S, Bang JY, Phadnis MA et al (2011) Endoscopic transmural drainage of peripancreatic fluid collections: outcomes and predictors of treatment success in 211 consecutive patients. J Gastrointest Surg 15:2080–2088
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Angela Saul, Miguel Angel Ramirez Luna, Carlos Chan, Luis Uscanga, Francisco Valdovinos Andraca, Jorge Hernandez Calleros, Javier Elizondo, Felix Tellez Avila report that there is no conflict of interest in this publication.
Rights and permissions
About this article
Cite this article
Saul, A., Luna, M.A.R., Chan, C. et al. EUS-guided drainage of pancreatic pseudocysts offers similar success and complications compared to surgical treatment but with a lower cost. Surg Endosc 30, 1459–1465 (2016). https://doi.org/10.1007/s00464-015-4351-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4351-2