Abstract
Objective
High-resolution manometry of the esophagus has gained worldwide acceptance, using different solid-state catheters. Thus, normal values for lower esophageal sphincter (LES) resting pressure in suspected gastroesophageal reflux disease patients have been established using water-perfused manometry. These standard values are commonly applied using also solid-state techniques, although they have never been compared before. The aim of the study was to compare LES measurements obtained with water-perfused manometry with a solid-state technique.
Methods
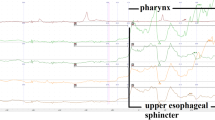
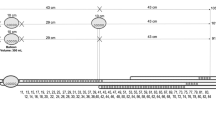
Thirty healthy subjects were studied twice on the same day: Technique 1: Station pull through using a water-perfused catheter with ports arranged at 0°, 90°, 180° and 270° which were averaged to give a mean LES pressure. Technique 2: Solid-state circumferential probe with a single station pull through. Data were collected using the same computer system and program. The LES pressures were randomly and blindly analyzed.
Results
Twenty-seven subjects out of 30 were analyzed. Using the solid-state system, the mean LES pressure was higher (15.0 vs. 23.3 mmHg, p = 0.003) and 19 of 27 (70 %) individual measurements were higher. Two subjects had a hypertensive LES by solid state (58.6 resp. 47.5 mmHg), while their pressures were normal with water-perfused manometry (21.0 resp. 23.4 mmHg). The distal esophageal pressures (mean of pressure at 3 and 8 cm above LES) were the same with the two techniques.
Conclusion
In normal control subjects, LES measurement using circumferential solid-state transducers yields higher pressures than standard water-perfused manometry. Which system yields the “true” resting pressure of the physiologic LES remains to be determined.

Similar content being viewed by others
References
Perdikis GWG, Vitito L, Stinson R (1993) The investigation of gastroesophageal reflux disease. In: R H (ed.) Gastroesophageal reflux disease. Austin, R. G. Landes Company, pp 30–58
Klingler PHP, DeVault K (1997) Gastroesophageal reflux: current controversies. In: Schein MWL (ed) Crucial controversies in surgery. Karger Landes, Basel, pp 118–131
DeMeester TR, Wang CI, Wernly JA, Pellegrini CA, Little AG, Klementschitsch P et al (1980) Technique, indications, and clinical use of 24 hour esophageal pH monitoring. J Thorac Cardiovasc Surg 79(5):656–670
Perdikis G, Lund RJ, Hinder RA, McGinn TR, Filipi CJ, Katada N et al (1997) Esophageal manometry and 24-hour pH testing in the management of gastroesophageal reflux patients. Am J Surg 174(6):634–637 discussion 7–8
Sifrim D, Blondeau K (2006) New techniques to evaluate esophageal function. Dig Dis 24(3–4):243–251
Simic AP, Skorobic ORN, Velickovic D, Ivanovic N, Pesko P (2013) Importance of ineffective esophageal motility in patients with erosive reflux disease on the long-term outcome after Nissen fundoplication. Eur Surg 45(1):15–21
Carlson DA, Pandolfino JE (2013) High-resolution manometry and esophageal pressure topography: filling the gaps of convention manometry. Gastroenterol Clin N Am 42(1):1–15
Biancani P, Zabinski MP, Behar J (1975) Pressure tension, and force of closure of the human lower esophageal sphincter and esophagus. J Clin Investig 56(2):476–483
Castell D (1993). In: Castell D (ed.) Esophageal motility testing. New York, Elsevier
Fennerty MB, Castell D, Fendrick AM, Halpern M, Johnson D, Kahrilas PJ et al (1996) The diagnosis and treatment of gastroesophageal reflux disease in a managed care environment, suggested disease management guidelines. Arch Intern Med 156(5):477–484
Wykypiel HGM, Granderath FA, Klingler PJ, Wetscher G (2002) Pathophysiology of gastro-oesophageal reflux disease (GERD) with respect to reflux-induced carcinogenisis. Eur Surg 34(5):296–302
Wykypiel HWG (2006) Surgical treatment of GERD: facts, discrepancies and recommendations. Eur Surg 38(4):225–226
Weijenborg PW, Kessing BF, Smout AJ, Bredenoord AJ (2014) Normal values for solid-state esophageal high-resolution manometry in a European population: an overview of all current metrics. Neurogastroenterol Motil 26(5):654–659
Kessing BF, Weijenborg PW, Smout AJ, Hillenius S, Bredenoord AJ (2014) Water-perfused esophageal high-resolution manometry: normal values and validation. Am J Physiol Gastrointest Liver Physiol 306(6):G491–G495
Niebisch S, Wilshire CL, Peters JH (2013) Systematic analysis of esophageal pressure topography in high-resolution manometry of 68 normal volunteers. Dis Esophagus 26(7):651–660
Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJ et al (2012) Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 24(Suppl 1):57–65
Bogte A, Bredenoord AJ, Oors J, Siersema PD, Smout AJ (2011) Reproducibility of esophageal high-resolution manometry. Neurogastroenterol Motil 23(7):e271–e276
Ayazi S, Hagen JA, Zehetner J, Ross O, Wu C, Oezcelik A et al (2009) The value of high-resolution manometry in the assessment of the resting characteristics of the lower esophageal sphincter. J Gastrointest Surg 13(12):2113–2120
Disclosures
Drs. P. Gehwolf, R. Hinder, K. DeVault, M. Edlinger, H. Wykypiel and P. Klingler have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Heinz F. Wykypiel and Paul J. Klingler are senior authors and equally contributed to this work.
Rights and permissions
About this article
Cite this article
Gehwolf, P., Hinder, R.A., DeVault, K.R. et al. Significant pressure differences between solid-state and water-perfused systems in lower esophageal sphincter measurement. Surg Endosc 29, 3565–3569 (2015). https://doi.org/10.1007/s00464-015-4109-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4109-x