Abstract
Background
Eradication of Helicobacter pylori prior to Roux-en-Y gastric bypass (RYGB) has been advocated as a measure to reduce the complications of anastomotic ulceration. However, evidence to support a causal relationship between preoperative H. pylori status and postoperative anastomotic ulceration is weak.
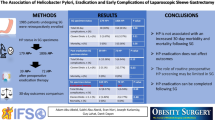
Methods
Intraoperative gastric biopsies were obtained on consecutive patients who underwent laparoscopic RYGB at our institution from December 2007 to June 2010. These samples were analyzed by Warthin–Starry stain for H. Pylori organisms. Retrospective chart review was conducted to determine the preoperative presence of acid dyspepsia and acid suppression therapy and to determine postoperative ulcer symptoms, smoking, NSAID or steroid use, and compliance with ulcer prophylaxis. The incidence of ulcer visualization, perforation, and stricture were obtained from a prospectively collected database. Fisher’s exact test was used for analyzing associations between discrete groups. Multiple logistic regression was used to assess associations between anastomotic ulcer complications and potential predictors.
Results
Histologic evaluation for H. pylori was available in 708 of the 728 patients who underwent RYGB. Fourteen patients were lost to follow up leaving 694 patients available for review. H. pylori was positive in 66 (9.5 %) patients who did not go on to receive definitive treatment for eradication. Marginal ulcers or related late complications were seen in a total of 113 (16.3 %) patients. In the H. pylori positive group, five patients (7.6 %) developed ulcer complications compared to 108 (17.1 %) in the H. pylori negative group (p = 0.05). Groups were not different in terms of preoperative demographics, postoperative ulcer prophylaxis compliance, steroid, NSAIDs, and cigarette use.
Conclusion
The presence of H. pylori infection at the time of RYGB was found to be associated with a significantly lower incidence of anastomotic ulcer complications postoperatively. This study brings into question efforts and expense allocated to identify and eradicate H. pylori prior to RYGB.
Similar content being viewed by others
References
Garrido AB Jr., Rossi M, Lim SE Jr. et al (2010) Early marginal ulcer following Roux-en-Y gastric bypass under proton pump inhibitor treatment: prospective multicentric study. Arg Gastroenterol. 47(2):130–134
Buschwald H, Cowan G, Pories W (2007) Surgical management of obesity. WB Saunders, Philadelphia, pp 297–303
Bhayani NH, Oyetunji TA, Chang DC et al (2012) Predictors of marginal ulcers after laparoscopic Roux-en-Y gastric bypass. J Surg Res 177(2):224–227
Rasmussen JJ, Fuller W, Ali MR (2007) Marginal ulceration after laparoscopic gastric bypass: an analysis of predisposing factors in 260 patients. Surg Endosc 21(7):1090–1094
Schirmer B, Erenoglu C, Miller A (2002) Flexible endoscopy in the management of patients undergoing Roux-en-Y gastric bypass. Obes Surg 12:634–638
Cleator IG, Rae A, Birmingham CL (1996) Ulcerogenesis following gastric procedure for obesity. Obes Surg 6(3):260–261
Papasavas PK, Gagne DJ, Donnelly PE, Salgado J et al (2008) Prevalence of Helicobacter pylori infection and value of preoperative testing and treatment in patients undergoing laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 4(3):383–388
Yang CS, Lee WJ, Wang HH, Huang SP (2006) The Influence of Helicobacter pylori infection on the development of gastric ulcer in symptomatic patients after bariatric surgery. Obes Surg 16(6):735–739
Hartin CW Jr., ReMine DS, Lucktong TA (2009) Preoperative bariatric screening and treatment of Helicobacter pylori. Surg Endosc 23(11):2531–2534
Rawlins L, Rawlins MP, Brown CC, Schumacher DL (2013) Effect of Helicobacter pylori on marginal ulcer and stomal stenosis after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 9(5):760–764
Renshaw AA, Rabaza JR, Gonzalez AM, Verdeja JC (2001) Helicobacter pylori infection in patients undergoing gastric bypass for morbid obesity. Obes Surg 11(3):281–283
Verma S, Sharma D, Kanwar P et al (2013) Prevalence of Helicobacter pylori infection in bariatric patients: a histologic assessment. Surg Obes Relat Dis. 9(5):679–685
Peterson WL, Fendrick AM, Cave DR et al (2000) Helicobacter pylori-related disease: guidelines for testing and treatment. Arch Intern Med 160:1285–1291
Chey WD, Wong BCY (2007) Practice parameters committee of the American College of Gastroenterology. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol 102:1808–1825
Malfertheiner P, Megraud F, O’Morain C et al (2007) Current concepts in the management of Helicobacter pylori infection: the Maastricht III concensus report. Gut 56(6):772–781
Labenz J, Blum AL, Bayerdorffer E et al (1997) Curing Helicobacter pylori infection in patients with duodenal ulcer may provoke reflux esophagitis. Gastroenterology 112:1442–1447
McKesson Corporation. Interqual Smart Sheets. 2006–Procedure Criteria Bariatric Surgery. San Francisco, CA, McKesson Corporation 2006
Kim EunYoung et al (2012) A case of small bowel ulcer associated with Heliocobacter pylori. Pediatric Gastroenterol Hepatol Nutr. 159(4):266–271
Cerqueira RM, Correia MR, Fernandes DC, Vilar H et al (2013) Cumulative Helicobacter pylori eradication therapy in obese patients undergoing gastric bypass surgery. Obes Surg 23(2):145–149
Csendes A, Smok G, Burgos AM, Canobra M (2012) Prospective sequential endoscopic and histologic studies of the gastric pouch in 130 morbidly obese patients submitted to Roux-en-Y gastric bypass. Arq Bras Cir Dig. 25(4):245–249
el-Zimaity HM (2000) Accurate diagnosis of Helicobacter pylori with biopsy. Gastroenterol Clin N Am 29:863–869
Woo JS, el-Zimaity HM, Genta RM et al (1996) The best gastric site for obtaining a positive rapid urease test. Helicobacter 1:256–259
Vanek VW, Catania M, Triveri K, Woodruff RW Jr. (2006) Retrospective review of the preoperative biliary and gastrointestinal evaluation for gastric bypass surgery. Surg Obes Relat Dis 2:17–23
Acknowledgments
Dr. Fred Anderson and the Center for Outcomes Research for statistical analysis.
Disclosures
Richard A. Perugini, Qi L. Wang, Donald R. Czerniach, Julie Flahive, Philip A. Cohen, and John J. Kelly have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kelly, J.J., Perugini, R.A., Wang, Q.L. et al. The presence of Helicobacter pylori is not associated with long-term anastomotic complications in gastric bypass patients. Surg Endosc 29, 2885–2890 (2015). https://doi.org/10.1007/s00464-014-4022-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-4022-8