Abstract
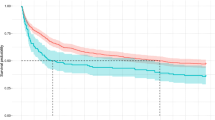
There is little evidence regarding the long-term prognosis of patients with aspiration pneumonia. This study aimed to investigate post-discharge survival time and prognostic factors in older patients hospitalized for aspiration pneumonia. This retrospective cohort study included patients aged ≥ 65 years hospitalized for aspiration pneumonia and discharged alive from a tertiary care hospital in Japan between April 2009 and September 2014. Candidate prognostic factors were patient’s age, sex, body mass index (BMI), performance status, chronic conditions, CURB-65 score, serum albumin level, hematocrit concentration, nutritional pathway at discharge, and discharge location. Kaplan–Meier curves were determined and multivariable survival analysis using Cox regression model was performed to analyze the effect of each factor on mortality. In total, 209 patients were included in this study. The median age was 85 years, 58% of the patients were males, 33% had a performance status of 4 and 34% were discharged home. Among the patients, 65% received oral intake, 23% received tube feeding, and 21% received parenteral nutrition at discharge. During the follow-up period, 77% of the patients died, and the median post-discharge survival time was 369 days. Besides male sex and low BMI, tube feeding (adjusted hazard ratio (aHR) = 1.70, 95% confidence interval (CI) 1.11–2.59) and parenteral nutrition (aHR = 4.42, 95% CI 2.57–7.60) were strongly associated with mortality. Long-term prognosis of patients hospitalized for aspiration pneumonia was extremely poor. The nutritional pathway at discharge was a major prognostic factor. These results may be useful for future care and research.



Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available because they contain information that could compromise the privacy of research participants, but are available from the corresponding author on reasonable request.
References
Bennett J, Vella C. Aspiration pneumonia. BMJ Best Practice. https://bestpractice.bmj.com/topics/en-gb/3000171 (2023). Accessed 16 Nov 2023.
Langmore SE, Terpenning MS, Schork A, Chen Y, Murray JT, Lopatin D, et al. Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia. 1998;13:69–81.
Cabre M, Serra-Prat M, Palomera E, Almirall J, Pallares R, Clavé P. Prevalence and prognostic implications of dysphagia in elderly patients with pneumonia. Age Ageing. 2009;39:39–45.
Ministry of Health, Labour and Welfare. Reiwa ni nen kanja tyōsa no gaikyō. https://www.mhlw.go.jp/toukei/saikin/hw/kanja/20/index.html. Accessed 16 Nov 2023.
Wu CP, Chen YW, Wang MJ, Pinelis E. National trends in admission for aspiration pneumonia in the United States, 2002–2012. Ann Am Thorac Soc. 2017;14:874–9.
Palacios-Ceña D, Hernández-Barrera V, López-de-Andrés A, Fernández-de-las-Peñas C, Palacios-Ceña M, de Miguel-Díez J, et al. Time trends in incidence and outcomes of hospitalizations for aspiration pneumonia among elderly people in Spain (2003–2013). Eur J Intern Med. 2017;38:61–7. https://doi.org/10.1016/j.ejim.2016.12.022.
Gupte T, Knack A, Cramer JD. Mortality from aspiration pneumonia: incidence, trends, and risk factors. Dysphagia. 2022;37:1493–500. https://doi.org/10.1007/s00455-022-10412-w.
Ministry of Health, Labour and Welfare. Reiwa yo nen jinkō dōtai tōkei no gaikyō. https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/kakutei22/index.html. Accessed 16 Nov 2023.
Teramoto S, Fukuchi Y, Sasaki H, Sato K, Sekizawa K, Matsuse T, et al. High incidence of aspiration pneumonia in community- and hospital-acquired pneumonia in hospitalized patients: a multicenter, prospective study in Japan. J Am Geriatr Soc. 2008;56:577–9.
Komiya K, Ishii H, Kadota JI. Healthcare-associated pneumonia and aspiration pneumonia. Aging Dis. 2015;6:27–37.
Momosaki R, Yasunaga H, Matsui H, Horiguchi H, Fushimi K, Abo M. Predictive factors for oral intake after aspiration pneumonia in older adults. Geriatr Gerontol Int. 2016;16:556–60.
ASPENB Directors, Jacobs DO, Helton S. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. J Parenter Enter Nutr. 2002;26:1SA-138SA.
Komiya K, Usagawa Y, Kadota JI, Ikegami N. Decreasing use of percutaneous endoscopic gastrostomy tube feeding in Japan. J Am Geriatr Soc. 2018;66:1388–91.
Taylor JK, Fleming GB, Singanayagam A, Hill AT, Chalmers JD. Risk factors for aspiration in community-acquired pneumonia: analysis of a hospitalized UK cohort. Am J Med. 2013;126:995–1001.
Kim H, Jo S, Lee JB, Jin Y, Jeong T, Yoon J, et al. Diagnostic performance of initial serum albumin level for predicting in-hospital mortality among aspiration pneumonia patients. Am J Emerg Med. 2018;36:5–11. https://doi.org/10.1016/j.ajem.2017.06.039.
Maeda K, Akagi J. Muscle mass loss is a potential predictor of 90-day mortality in older adults with aspiration pneumonia. J Am Geriatr Soc. 2017;65:e18-22.
Yoon HY, Shim SS, Kim SJ, Lee JH, Chang JH, Lee SH, et al. Long-term mortality and prognostic factors in aspiration pneumonia. J Am Med Dir Assoc. 2019;20:1098-1104.e4. https://doi.org/10.1016/j.jamda.2019.03.029.
Yoshimatsu Y, Melgaard D, Westergren A, Skrubbeltrang C, Smithard DG. The diagnosis of aspiration pneumonia in older persons: a systematic review. Eur Geriatr Med. 2022;13:1071–80. https://doi.org/10.1007/s41999-022-00689-3.
Komiya K, Rubin BK, Kadota JI, Mukae H, Akaba T, Moro H, et al. Prognostic implications of aspiration pneumonia in patients with community acquired pneumonia: a systematic review with meta-analysis. Sci Rep. 2016;6:1–2.
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. Infectious Diseases Society of America/American Thoracic Society Consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44:S27.
Cichero JAY, Lam P, Steele CM, Hanson B, Chen J, Dantas RO, et al. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: the IDDSI framework. Dysphagia. 2017;32:293–314.
Holter JC, Ueland T, Jenum PA, Müller F, Brunborg C, Frøland SS, et al. Risk factors for long-term mortality after hospitalization for community-acquired pneumonia: a 5-year prospective follow-up study. PLoS ONE. 2016;211:1–16.
Johnstone J, Eurich DT, Majumdar SR, Jin Y, Marrie TJ. Long-term morbidity and mortality after hospitalization with community-acquired pneumonia: a population-based cohort study. Medicine (Baltimore). 2008;87:329–34.
Noguchi S, Yatera K, Kato T, Chojin Y, Fujino Y, Akata K, et al. Impact of the number of aspiration risk factors on mortality and recurrence in community-onset pneumonia. Clin Interv Aging. 2017;12:2087–94.
Ebihara T, Miyamoto T, Kozaki K. Prognostic factors of 90-day mortality in older people with healthcare-associated pneumonia. Geriatr Gerontol Int. 2020;20:1036–43.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–55.
Lim WS, Van Der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–82.
Ministry of Health, Labour and Welfare. Dai 21 kai seimeihyō no gaikyō. https://www.mhlw.go.jp/toukei/saikin/hw/life/21th/index.html. Accessed 16 Nov 2023.
Masaki S, Kawamoto T. Comparison of long-term outcomes between enteral nutrition via gastrostomy and total parenteral nutrition in older persons with dysphagia: a propensity-matched cohort study. PLoS ONE. 2019;14:1–12. https://doi.org/10.1371/journal.pone.0217120.
Reade MC, Weissfeld L, Angus DC, Kellum JA, Milbrandt EB. The prevalence of anemia and its association with 90-day mortality in hospitalized community-acquired pneumonia. BMC Pulm Med. 2010. https://doi.org/10.1186/1471-2466-10-15.
Stauder R, Valent P, Theurl I. Anemia at older age: etiologies, clinical implications, and management. Blood. 2018;131:505–14.
Nishida T, Yamabe K, Honda S. The influence of dysphagia on nutritional and frailty status among community-dwelling older adults. Nutrients. 2021;13:1–8.
Sakai K, Nakayama E, Yoneoka D, Sakata N, Iijima K, Tanaka T, et al. Association of oral function and dysphagia with frailty and sarcopenia in community-dwelling older adults: a systematic review and meta-analysis. Cells. 2022;11:2199.
Park CM, Kim W, Rhim HC, Lee ES, Kim JH, Cho KH, et al. Frailty and hospitalization-associated disability after pneumonia: a prospective cohort study. BMC Geriatr. 2021;21:1–8.
Dorner B, Posthauer ME, Friedrich EK, Robinson GE. Enteral nutrition for older adults in nursing facilities. Nutr Clin Pract. 2011;26:261–72.
Bellelli G, Frisoni GB, Trabucchi M. Feeding tube use in Italian nursing homes: the role of cultural factors. J Am Med Dir Assoc. 2005;6:87–8.
Aita K, Takahashi M, Miyata H, Kai I, Finucane TE. Physicians’ attitudes about artificial feeding in older patients with severe cognitive impairment in Japan: a qualitative study. BMC Geriatr. 2007;7:1–9.
Komiya K, Ishii H, Teramoto S, Yasuda T, Sato S, Yamamoto H, et al. Medical professionals’ attitudes toward tube feeding for themselves or their families: a multicenter survey in Japan. J Palliat Med. 2012;15:561–6.
Acknowledgements
The authors are grateful to the hospitals and care facilities from which the patients were discharged for providing prognostic data.
Funding
This research did not receive any funding from agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors (YH, YH, MN, TO, and KS) contributed to the conception or design of the study, reviewed and edited the manuscript, contributed to the interpretation of the data and the analyses, performed a critical review of the manuscript, and gave the final approval of the manuscript before submission. YH, YH, and KS collected the patient data. YH performed the statistical analyses and drafted the manuscript. YH, MN, TO, and KS supervised the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical Approval
The Ethics Committees of the institutions approved the study protocol (research approval no. 3529 and 20–311) and waived the requirement for informed consent because of the retrospective nature of the study.
Informed Consent
Information about the study was displayed on the institution's website and refusal to participate in the study was received.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Honda, Y., Homma, Y., Nakamura, M. et al. Extremely Poor Post-discharge Prognosis in Aspiration Pneumonia and Its Prognostic Factors: A Retrospective Cohort Study. Dysphagia (2024). https://doi.org/10.1007/s00455-023-10665-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00455-023-10665-z