Abstract
Patients with multiple system atrophy (MSA) frequently experience dysphagia but only few studies analyzed its characteristics. The aim of this study was to describe the swallowing characteristics in these patients using fiberoptic endoscopic evaluation of swallowing (FEES). In addition, the swallowing abilities in patients with predominantly cerebellar MSA (MSA-C) and predominantly parkinsonian MSA (MSA-P) were compared. Twenty-five patients with MSA (16 MSA-P and 9 MSA-C) were enrolled. Clinical data including age, sex, functional oral intake scale (FOIS) score, body mass index (BMI) and the results of the global disability-unified MSA rating scale (GD-UMSARS) were collected. Three different textures of food (liquid, semisolid, solid) were provided during FEES examination. The characteristics of dysphagia (safety, efficiency, phenotype) and laryngeal movement alterations were analyzed. Delayed pharyngeal phase (92%) and posterior oral incontinence (52%) were the phenotypes more frequently seen. Penetration was more frequent with Liquid (68%), while aspiration occurred only with Liquid (20%). Residues of ingested food were demonstrated both in the pyriform sinus and in the vallecula with all the consistencies. Vocal fold motion impairment was the laryngeal movement alteration most frequently encountered (56%). No significant differences between patients with MSA-P and MSA-C in the dysphagia characteristics and laryngeal movement alterations were found. Patients with MSA frequently experience swallowing impairment and altered laryngeal mobility. Dysphagia characteristics and laryngeal movements alterations seems to be similar in MSA-C and MSA-P.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple system atrophy (MSA) is an adult-onset, sporadic, progressive neurodegenerative disease caused by oligodendroglial aggregation of α-synuclein affecting predominantly the nigrostriatal, olivo-ponto-cerebellar, and autonomic systems [1,2,3,4]. MSA is characterized by varying severity of parkinsonian features, cerebellar ataxia, autonomic failure, urogenital dysfunction, and corticospinal disorders [1]. MSA progresses rapidly with a mean survival of 6 to 10 years after diagnosis [4]. The current criteria define four degrees of certainty for diagnosis, neuropathologically established MSA, clinically established MSA, clinically probable MSA, and possible prodromal MSA, and two phenotypes according to the clinical characteristics: predominantly cerebellar (MSA-C) or parkinsonian (MSA-P) [5].
In the recently developed criteria for MSA diagnosis [5], stridor, defined as respiratory sound caused by laryngeal dysfunction leading to glottal narrowing [6, 7], has been added as supportive non-motor feature. Laryngopharyngeal dysfunction is frequent and has been associated with decreased life expectancy and quality of life [1]. As far as the laryngeal dysfunction is concerned, Gandor et al. [1] analyzed laryngeal movement disorders using a specific task protocol and demonstrated their high prevalence in patients with MSA and suggested that irregular arytenoid cartilage movements could be used as a clinical marker to delineate MSA from PD with a high specificity and sensitivity. Dysphagia has been reported as a frequent and disabling symptom in MSA as well. However, despite its high prevalence (ranging from 31 to 78% [8]) and important clinical consequences such as aspiration pneumonia, sudden death due to aspiration, malnutrition, dehydration, and infectious complications [9,10,11], only few studies analyzed the swallowing characteristics in patients with MSA [12]. In particular, the dysphagia phenotype in this population has never been investigated. Scarce information regarding the differences between MSA-P and MSA-C in dysphagia features and severity are available; moreover, the majority of previous reports used videofluoroscopic swallowing study (VFSS) to assess dysphagia [13,14,15,16,17,18,19] rather than fiberoptic endoscopic evaluation of swallowing (FEES) [12], which allows a combined assessment of swallowing and laryngeal function. Consequently, few information regarding the swallowing characteristics analyzed through FEES are available so far [12, 20], even if severe dysphagia or the need for percutaneous endoscopic gastrostomy (PEG) for feeding are considered milestones of disease progression in MSA [8].
The aims of this study are: (1) to describe the dysphagia phenotype in MSA patients analyzed using FESS; (2) to compare the swallowing abilities in patients with MSA-C and MSA-P; (3) to evaluate laryngeal motility in patients with MSA; (4) to analyze the associations among the characteristics of dysphagia (safety and efficiency impairment, dysphagia phenotypes) and laryngeal motility alterations. The relevance of this study lies in the fact that a deeper knowledge of the characteristics of dysphagia in patients with MSA might be useful in the clinical practice for early diagnosis and proper dysphagia treatment.
Material and Methods
The present cross-sectional study was conducted in accordance with the Declaration of Helsinki, and it was previously approved by the Institutional Review Board of our hospital. Data were collected prospectively.
Participants
Participants underwent a thorough neurologic assessment and were diagnosed with either clinically established or probable MSA-P or MSA-C according to criteria proposed by the Movement Disorder Society [5]. Clinical data from a total of 25 patients (14 females and 11 males) affected by MSA (16 patients with MSA-P and 9 patients with MSA-C) were evaluated. All the enrolled subjects met the following inclusion criteria: age above 18 years; full oral diet with more than a single consistency; functional oral status (all natural teeth or partial tooth loss rehabilitated with an adjusted partial dental prosthesis [21]), no medical history of gastroenterological, respiratory, rheumatologic, metabolic, hematologic disorders. Exclusion criteria were intolerance to the components of the tested foods, additional neurologic diseases, history of head and neck cancer.
The functional oral intake scale (FOIS) [22,23,24], a seven-point ordinal scale indicating limitations in oral feeding which ranges from one (nothing by mouth) to seven (total oral diet with no restriction), was used to collect information regarding patient’s oral intake. The FOIS was administered immediately before the FEES examination. Information regarding the body mass index (BMI) were also collected as well as the results of the fourth part (IV, Global Disability Scale) of the unified MSA rating scale (GD-UMSARS) [25] as a marker of disease stage. Specifically, its scores range from 1 (completely independent. Able to do to all chores with minimal difficulties or impairment. Essentially normal) to 5 (totally dependent and helpless. Bedridden). The FOIS scale was selected because it has been validated in Italian [24] and it is widely used in dysphagic population. The GD-UMSARS Item 2 of Part 1 has not been used as it focuses on swallowing impairment, while the FOIS focuses on functional oral intake. In addition, according to the results of El Fassi et al. [26] the UMSARS-based assessment of dysphagia alone seems not to completely capture the key aspects of pharyngo-laryngeal dysfunction reflecting swallowing efficiency.
All the patients received exhaustive explanations regarding aims and objectives of the research, FEES evaluation and all the possible risks involved. All the enrolled patients gave their written informed consent. The characteristics of the enrolled patients are reported in Table 1.
FEES Examination
Each FEES was conducted by a senior Phoniatrician. A XION EF-N flexible endoscope with a diameter of 3.4 mm and a length of 320 mm (XION GmbH, Berlin, Germany) mounted on an EndoSTROB E camera (XION GmbH, Berlin, Germany) was used. All the videos were processed using the software Daisy Viewer 2.0 (INVENTIS srl, Padua, Italy) and stored in an anonymous form in.AVI format.
Each patient was seated on a comfortable chair, leaning back (between 75 and 90° approximately) with his arms on the armrests and keeping the head in neutral position to obtain the best posture for the examination. No local anesthetic drugs (e.g., lidocaine spray) were used in order not to alter pharyngo-laryngeal sensibility [27]. The endoscope was introduced into the widest nasal cavity and kept at a level just inferior to the uvula to maximize the field of view, including the larynx, the glossoepiglottic valleculae and the pyriform sinuses [28,29,30]. Three different textures of food were provided during FEES examination to evaluate swallowing:
-
Liquid: room temperature skim milk (< 50 mPa·s at 50s−1 and 300s−1; International Dysphagia Diet Standardisation Iniatiative—IDDSI Level 0) [30] was used for thin Liquid trials.
-
Semisolid: room temperature Crème Line vanilla pudding (Nutrisens Medical SAS, Francheville, France) (2583.3 ± 10.41 mPa·s at 50s−1 and 697.87 ± 7.84 mPa·s at 300s−1; IDDSI Level 4) was used for semisolid trials.
-
Solid: a quarter and half of an 8-g dry biscuit (4 g per trial; IDDSI Level 7) were used for Solid trials.
FEES examinations were rated independently by three operators using the video files. All of them were speech and language therapists (SLTs) with at least 5 years of experience in FEES examinations. SLTs were blind to each other and to participants’ data, since videos were stored in an anonymous form. Two independent SLTs rated the videos using validated ordinal scales for swallowing safety and efficiency; inter-rater reliability between the 2 raters was analyzed. In case a difference > 1 level at each FEES rating scale occurred between the 2 raters, a 3rd SLT assessed the videos and decided on both ratings [27].
Different parameters were analyzed using the FEES examination:
-
Dysphagia phenotypes defined according to the videoendoscopic scenarios proposed by Desuter [29, 31]. In particular, the presence of the following six phenotypes was assessed: protective deficit, posterior oral incontinence, delayed pharyngeal phase, oropharyngeal dyspraxia, propulsion deficit, resistive issue. Protective deficits include impairment of the following mechanisms: laryngeal elevation, glottis closure, tongue propulsion. Posterior oral incontinence is defined as inability of the patient to contain the bolus in the oral cavity when asked to. Delayed pharyngeal phase is defined as a delay of at least one on the following mechanisms when the patient is asked to swallow: arytenoid approximation and glottis closure, laryngeal elevation, tongue base propulsion, resulting in a progression of the bolus in the piriform sinuses beyond the glossopharyngeal ligaments before the swallowing reflex occurs. Oropharyngeal dyspraxia is the absence of pharyngeal swallowing and consequently retention of the bolus in the mouth or the appearance of cyclical movements of aborted movements of tongue base retraction. Propulsion deficit occurs when residue in the valleculae and/or the pirifom sinuses are found with weak tongue base retraction and/or, pharyngeal peristalsis and/or laryngeal elevation. Finally, resistive issue is found when residue occur in the retrocricoid region.
-
Safety impairment (Penetration/aspiration): the severity of penetration/aspiration was rated using the Penetration Aspiration Scale (PAS) [32]. The PAS is an 8-points scale ranging from 1 (materials do not enter the airway) to 8 (materials enter the airway, passes below the vocal folds and no effort is made to eject). Penetration was defined as the bolus entering the laryngeal vestibule over the rim of the larynx (PAS score from 2 to 5). Aspiration was defined as the bolus passing below the true vocal folds (PAS score 6 or above). Safety of swallow was also evaluated similar to Tabor et al.’s study [33]. In particular, on the basis of the PAS score, each swallow was classified as unsafe if the material entered the laryngeal vestibule (PAS ≥ 3). In addition, in order to analyze the timing of unsafe swallows, each event was classified in “before”, “during” or “after” the swallow. The worst PAS score for each consistency and for each subject was considered for statistical analyses.
-
Efficiency impairment (pharyngeal residue): the amount of pharyngeal residue after the swallow was rated using the yale pharyngeal residue severity rating scale (YPRSRS) vallecula and pyriform sinus [34]. Efficiency of swallow was also evaluated. In particular, a YPRSRS scores ≥ 3 (mild residue) was considered suggestive for an inefficient swallow. The worst YPRSRS score for each consistency and for each subject was considered for statistical analyses.
-
Laryngeal movement analysis was performed using the MSA-FEES protocol used by Gandor et al. [1]. In particular, laryngeal assessment was performed at rest and during abductor and adductor tasks in order to evaluate the presence of 1 vocal fold (VF) motion impairment (VFMI); 2 VF fixation (VFF); 3 paradoxical VF motion (PVFM); 4 irregular arytenoid cartilages movements (iACM); 5 laryngeal stridor.
Statistical Analysis
Statistical tests were performed using the SPSS 23.0 statistical software (SPSS Inc., Chicago, IL). The Kolmogorov–Smirnov test was used to test the normality of the distribution of FEES parameters among the patients. Since this test demonstrated that the distribution was not normal, non-parametric tests were used. Inter-rater reliability of FEES scoring between the two SLTs was analyzed. Weighted kappa with quadratic weighting was calculated [35]; k values were interpreted as follows: ≤ 0.20 poor agreement, 0.21–0.40 fair agreement, 0.41–0.60 moderate, 0.61–0.80 good, and 0.81–1.00 very good [36]. Mann–Whitney U test was used to compare the differences in age, BMI, FOIS scores between patients with MSA-P and MSA-C. Fisher’s exact test was used to compare the distribution of sex, GD-UMSARS score, dysphagia characteristics (safety, efficiency, phenotypes) and presence of laryngeal movement alterations between the two groups of patients because the variables were considered categorical [37, 38]. The Fisher’s exact test was also used to compare the distribution of patients according to the presence of unsafe swallow, inefficient swallow, and presence of laryngeal movement alterations on one side and the different dysphagia phenotypes leading to dysphagia on the other. Considering the number of tests performed in this last comparison, in order to avoid the risk of inflation of type 1 error a Bonferroni correction was applied, and a more stringent alpha level was used (p = 0.025).
Results
Characteristics of the recruited population are reported in Table 1. There were 11 males and 5 females in the MSA-P group and 6 males and 3 females in the MSA-C group. This difference was found not significant at Fisher’s exact test (0.098). The median age was 68 and 63 years in the MSA-P and MSA-C group respectively. This difference was found not significant at Mann–Whitney test (p = 0.095). The median BMI was 23.1 and 25.9 in the MSA-P and MSA-C group respectively. Also, in this case the difference was found not significant at Mann–Whitney test (p = 0.522). No statistically significant differences in the distribution FOIS and GD-UMSARS scores were demonstrated at Fisher’s exact test between patients with MSA-P and MSA-C (p = 0.329 and p = 0.054 respectively). All the enrolled patients had a full oral diet and the median FOIS score was 7 (interquartile range 5–7). FEES protocol was performed using all the three consistencies in 19 patients, in the remaining 6 patients Solid was not tested, Liquid was not tested in 1 patient, and Semisolid was not tested in another 1 patient. One or more consistencies were not tested if there was a significant risk of choking. All the subjects included in the study completed the FEES protocol using at least one consistency. The time required to complete FEES never exceeded 15 min. FEES scoring inter-rater agreement ranged from good to very good. In particular, inter-rater agreement with each of the different consistencies for the PAS (k > 0.86) and for the YPRSRS in the vallecula and pyriform sinus (k > 0.81 and k > 0.85, respectively) was very good.
Dysphagia Phenotypes
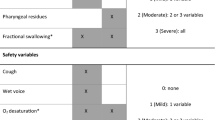
The dysphagia phenotypes have been analyzed both in the overall sample for each consistency (Fig. 1) and in MSA-C and MSA-P subgroup of patients (Fig. 2). When considering the overall sample, a Delayed pharyngeal phase represented the most common phenotype (92%) with all consistencies, followed by Posterior oral incontinence mainly for Liquids (52%) and Propulsion deficit (44%) mainly with Semisolids and Solids. Five (20%) patients showed only one isolated phenotype, nine (36%) patients showed two combined phenotype, and eight (32%) patients showed three combined phenotypes. The differences between patients with MSA-P and MSA-C were not significant at Fisher test. In particular, for both groups Delayed pharyngeal phase and Posterior oral incontinence represented the most common phenotypes.
Swallowing Safety
The differences in the distribution of the 3 PAS categories (normal, penetration, aspiration) for the 3 consistencies are reported in Table 2. Penetration was more frequent with Liquid (17 out of 24 patients, 68%), followed by Semisolid (13 out of 24 patients, 52%). Aspiration occurred only with Liquid (5 patients, 20%) and no aspiration was demonstrated for the Semisolid and Solid. The distribution of PAS categories between MSA-P and MSA-C patients was found different only for the Semisolid (p = 0.027) with penetration occurring significantly more frequently in patients with MSA-C. No statistically significant differences were found for the liquid and solid (p = 0.063 and p = 0.663 respectively).
Regarding swallowing safety, with the Liquid consistency 16 out of 24 patients (66.7%) had unsafe swallows (5 patients had aspiration and 9 had penetration). Compromised airway protection occurred across all timing zones (before vs during vs after), however, unsafe swallow with Liquid consistency was more frequent “during” the swallow (10 out of 16 patients), followed by “before” the swallow (6 out of 16 patients). With the Semisolid consistency 5 patients (20.8%) had unsafe swallows but aspiration was never documented. Unsafe swallows with Semisolids occurred more frequent “during” swallow (3 out of 5 patients), followed by “before” swallow (2 out of 5 patients). Finally, with the Solid consistency unsafe swallows were demonstrated in 2 patients. Both patients had penetration “before” swallow. The distribution of unsafe swallows in the two groups of patients is reported in Table 3. No statistically significant differences between patients with MSA-P and MSA-C were demonstrated at Fisher test (p = 0.668, p = 0.555, and p = 0.386 for the Liquid, Semisolid, and Solid consistencies respectively).
Swallowing Efficiency
The YPRSRS scores obtained in patients with MSA-P, MSA-C are reported in Table 2. The median YPRSRS vallecula score was 3 for all the consistencies, while the YPRSRS pyriform sinus score was 3 for the Liquid, 2 for the Semisolid and 1 for the Solid. No statistically significant differences in the distribution of YPRSRS was demonstrated between the two groups with the only exception for the YPRSRS pyriform sinus score obtained during Liquid trials which appeared to be significantly lower in patients with MSA-P than in those with MSA-C (p = 0.451 at Fisher test).
Regarding swallowing efficiency, with the Liquid consistency 13 and 16 out of 24 patients (54.2% and 66.7%) had at least mild residue after swallow in the valleculae and pyriform sinuses respectively. With the Semisolid consistency 16 and 11 out of 24 patients (66.7% and 45.8%) had at least mild residue after swallow in the valleculae and pyriform sinuses respectively. Finally, with the Solid consistency 10 and 4 out of 19 patients (52.6% and 21.1%) had at least mild residue after swallow in the valleculae and pyriform sinuses respectively. The distribution of inefficient swallows in the two groups of patients is reported in Table 3. No statistically significant differences between patients with MSA-P and MSA-C were demonstrated at Fisher test for the valleculae region (p = 0.300, p = 0.553, and p = 0.570 for the liquid, semisolid, and solid consistencies respectively). Similarly, no statistically significant differences between the two groups were demonstrated at Fisher test for the region of pyriform sinuses for the Semisolid (p = 0.444) and Solid (p = 0.475) consistencies, while patients with MSA-C demonstrated a significant lower swallow efficiency with the Liquid consistency (p = 0.009).
Laryngeal Movement Alterations
Laryngeal movement analysis was performed in all the enrolled subjects and the results are reported in Fig. 3. The majority of patients demonstrated at least 1 laryngeal movement alteration (19 out of 25 patients, 76%). VFMI and the iACM were the conditions most frequently encountered (14 patients, 56%, and 13 patients, 52% respectively). Six patients (24%) showed only one laryngeal movement alteration, 5 (20%) showed two combined conditions, 6 (24%) showed three combined conditions, and 2 (8%) showed four combined conditions. No statistically significant differences between patients with MSA-P and MSA-C at Fisher test were demonstrated.
Laryngeal movement analysis in the cohort of patients. VFMI vocal fold motion impairment, VFF vocal fold fixation, PVFM paradoxical vocal fold motion, iACM irregular jitter and flutter of the arytenoid region, LS laryngeal stridor, MSA-P predominantly parkinsonian multiple system atrophy, MSA-C predominantly cerebellar multiple system atrophy. The number of patients affected by laryngeal movement disorders are reported
Association Analysis
The distribution of patients according to the presence of unsafe swallow, inefficient swallow and presence of laryngeal movement alterations on one side and the different dysphagia phenotypes on the other was studied using Fisher test. The results are reported in Table 4. The only significant difference were found for patients with Propulsion deficit who demonstrated a significant lower swallow efficiency (YPRSRS valleculae score) than patients without Propulsion deficit.
Discussion
In the present study the characteristics of dysphagia in patients with MSA were analyzed using FEES. The dysphagia phenotypes have been analyzed for the first time. In addition, the laryngeal motility, as well as the associations among unsafe and not-efficient swallow and laryngeal motility impairment were evaluated.
Dysphagia Phenotypes
The large majority of patients with MSA demonstrated a swallowing impairment and in 80% of them 2 or more dysphagia phenotypes were detected. The more common were the Delayed pharyngeal phase with all the tested consistencies, followed by Posterior oral incontinence mainly visible with Liquids and Propulsion deficit with Semisolids and Solids. These data are in line with those of Warnecke et al. [20] who performed a systematic literature review in order to analyze the characteristics of neurogenic dysphagia using FEES. The authors reported that patients with atypical parkinsonian syndromes more commonly present pharyngolaryngeal movement disorders, premature bolus spillage and impaired swallowing reflex. Higo et al. [13] analyzed a total of 29 patients with MSA (22 MSA-C and 7 MSA-P) using VFS and found a delayed bolus transport in 73% of patients and impaired oral bolus control in 49%. The same author a couple of years later [14] analyzed the swallowing function in a group of 21 patients with MSA-C and found that swallowing function in the oral phase became gradually disturbed with the progression of the disease affecting both the bolus transport and bolus holding. Finally, Park et al. [15] who studied the swallowing outcomes following speech therapy in 7 patients with MSA-C using VFS found that patients suffered mainly from pharyngeal phase disturbances and premature bolus loss.
In our sample no differences between patients with MSA-C and MSA-P were demonstrated. This finding agrees with the results of Vogel et al. [12] who evaluated the endoscopic characteristics of dysphagia using FEES in 57 PD, 12 MSA-C and 45 MSA-P patients and found no differences in dysphagia pattern between MSA-C and MSA-P patients. In addition, Fernagut et al. [39] did not find any significant differences in the severity of dysphagia between patients with MSA-P and MSA-C. Lee et al. [18] analyzed the swallowing functions in a group of 31 patients with MSA-P and 21 with MSA-C using VFS. The authors did not find any significant differences in the oral and pharyngeal transit time, triggering of pharyngeal swallow, and premature bolus loss between the two groups. Moreover, Higo et al. [13, 14] demonstrated oral and pharyngeal dysfunction in both patients with MSA-P and MSA-C. The authors suggested that dysphagia in patients with MSA-P is a result of Parkinsonism which manifests with bradykinesia and rigidity of the tongue with consequent delayed bolus transport from the oral cavity to the pharynx and disturbance of bolus holding in the oral cavity, while in patients with MSA-C it is the disturbed coordination of tongue movement by cerebellar dysfunction, rather than Parkinsonism, which determines swallowing dysfunction in the oral phase at the early stage even if parkinsonism is also involved at the late stage [13, 14]. It is possible that in patients with MSA, both Parkinsonism and cerebellar dysfunction may distinctly contribute to dysphagia and consequently the absence of statistically significant differences between patients with MSA-P and MSA-C found in the present study might be related to the low number of enrolled patients. On the other hand, it is also possible that no difference exists in the dysphagia phenotypes in MSA-P and MSA-C. Further studies are needed to test these hypotheses.
Swallowing Safety
Aspiration (bolus below the true vocal folds) occurred only with Liquid and was found in the 20% of the sample, while penetration (bolus enters the airway but not below the true vocal folds) was far more frequent (68%), in particular with Liquid, followed by Semisolid. Accordingly, safety of swallow was lower with Liquid with a compromised airway protection occurring both “during” and “before” the swallow in the majority of patients. These data suggest that the viscosity of the ingested food significantly affect the swallowing safety in patients with MSA. This finding agrees with Clavé et al. [40] who found that in patients with neurogenic dysphagia, increasing viscosity brought about a dramatic improvement on safety by minimizing penetration and aspiration during swallow.
As far as the high percentage of patients who demonstrated penetration and/or aspiration found in the present paper is concerned, the results here reported are in accordance with those of Lee et al. [18] who found that penetration or aspiration occurred in 67.8% of patients with MSA. Several previous studies evaluated the prevalence of dysphagia among patients with MSA but no information regarding the PAS score were provided. For example, Vogel et al. [12] by analyzing through FEES the swallowing abilities in a group of 57 patients with MSA found that penetration and aspiration occurred in 21% and 7% of the sample respectively.
The Fisher test did not demonstrate any significant differences in the distribution of PAS categories and safety of swallow between patients with MAS-P and MSA-C with the only exception for the Semisolid. In particular, penetration occurred significantly more frequently in patients with MSA-C. A possible explanation is related to a delayed pharyngeal phase which is particularly common even in early stages in patients with MSA-C as reported by Higo et al. [14]. However, no differences in the safety of swallow between the two groups was demonstrated thus suggesting that the severity of dysphagia is similar in both phenotypes. This finding agrees with those of Do et al. [17] who did not find any significant differences in the incidence of aspiration pneumonia between patients with MSA-P and MSA-C.
Swallowing Efficiency
Residues of ingested food were demonstrated both in the pyriform sinus and in the vallecula with all the three consistencies. In addition, inefficient swallow was found in a high percentage of patients regardless of the consistency of the ingested food and of the phenotype of MSA, thus suggesting an impairment in the bolus propelling from the oropharynx to the esophagus. This finding is in accordance with the results of Higo et al. [13] who analyzed the manometric data of oropharyngeal and hypopharyngeal swallowing pressure in patients with MSA and found a decreased swallowing pressure compared to control subjects. In addition, the authors demonstrated bolus stasis at the pyriform sinuses in the 27.2% of patients with MSA. Similarly, Lee et al. [18] reported that the most common finding at VFS in patients with MSA was vallecular and pyriform sinus residues (89.8% and 63.2% respectively). Vogel et al. [12] found relevant pharyngeal residues in 50.9% of patients with MSA. Additionally, Ueha et al. [41] found abnormal hypertensive proximal esophageal contraction during swallowing, deficient upper esophageal sphincter (UES) relaxation and impaired UES relaxation in the 56%, 32% and 12% of patients with MSA.
Laryngeal Movement Alterations
FEES examination revealed that most patients with MSA demonstrated at least one laryngeal movement alteration. IACM and VFMI were the conditions most frequently encountered; in addition, more than half of the enrolled patients demonstrated more than 2 laryngeal movement alterations. These results are in line to those previously reported even if the percentages of patients affected by laryngeal movement alterations appear lower than those reported by Gandor et al. [1] and by Warnecke et al. [20]. In the former study, the authors analyzed laryngeal movement in a group of 57 patients with MSA and found that iACM was the most prevalent laryngeal findings (91.2% of the sample) followed by VFMI (75.4%) [1]. In the latter, the authors found irregular arytenoid cartilages movements and vocal fold abduction restriction in all patients with MSA [20]. It is possible that the lower percentages found in our study might be related to differences in the severity of MSA among the patients enrolled in the different studies. In our sample 9 patients scored 1 or 2 at GD-UMSARS, in the study of Gandor et al. [1] the median Hoehn and Yahr stage was 4 while in the study of Warnecke et al. [20] the mean Hoehn and Yahr stage was 3.75. On the other hand, other authors reported a lower prevalence of laryngeal movement disorders in patients with MSA. Higo et al. [19] performed laryngoscopy on 38 MSA patients to assess laryngeal function and found VFMI in 17 of them. Simpson et al. [42] reported “flickering movements of the vocal folds” in 3 of 6 MSA patients during laryngoscopy. Irregular tremulous movement of the arytenoid cartilages was detected also by Shimohata et al. [43]. As suggested by Gandor et al. [1], the systematic assessment of laryngeal function using task provoking maximum VF movement (which allowed an easier identification of motion abnormalities) might explain the higher prevalence of laryngeal movement disorders found in this study.
The underlying pathology of laryngeal symptoms in MSA still remains under debate [1]. Nonetheless, iACM seems to predict the occurrence of glottic area reduction [44] and has been suggested as a valuable clinical marker for MSA allowing for delineation from Parkinson disease [1, 20]. Therefore, as proposed by Gandor et al. [1], an early evaluation of laryngeal function should be performed when MSA is suspected.
Association Between Dysphagia Phenotypes and Laryngeal Functions
No significant differences in the safety of swallow and presence of laryngeal movement alterations on one side and the different dysphagia phenotypes on the other were demonstrated at Fisher’s exact test. This finding is difficult to compare since in none of the previous study the association among these elements was analyzed. On the other hand, patients with Propulsion deficit demonstrated a significantly lower swallow efficiency than patients without Propulsion deficit. This result agrees with those reported by Steele et al. [45]. In their systematic review the authors concluded that patients affected by poor pharyngeal contraction and tongue-base retraction experience more residues as the effort required for swallowing increases with thicker and harder foods.
Study Limitations
There are several limitations in this study. First, the number of enrolled patients is quite small, even if in line with previous studies. Because of the rarity of the disease, it was difficult to collect a large number of patients. For this reason, the results here reported should be considered with caution. For example, even if there is no statistically significant difference between MSA-P and MSA-C for GD-UMSARS, it doesn't seem that the two groups are homogenous populations. In fact, according to a power calculation a difference of about 40% in the percentage of patients with GD-UMSARS less than 4, will have a power of 80% with alpha equal to 5% with 32 and 16 patients in MSA-P and MSA-C groups, respectively (hypothesizing a 2 to 1 ratio). This further stress the need to take with extreme caution the results of the comparison between patients with MSA-P and MSA-C. In addition, a larger number of enrolled patients would have allowed to perform subgroup analysis on the basis of the severity of the disease. Dysphagia phenotypes were judged as present or absent, according to the classification proposed by Desuter [31], whose psychometric properties still need to be analyzed.
In conclusion even in MSA patients under full oral nutrition with more than one consistency unsafe and inefficient swallow are quite frequent. The most common dysphagia phenotypes are delayed pharyngeal phase and posterior oral incontinence. Propulsion deficit is associated with lower swallow efficiency. Swallowing function and abnormal laryngeal movements seems to be similar in patients with MSA-C and patients with MSA-P.
References
Gandor F, Vogel A, Claus I, et al. Laryngeal movement disorders in multiple system atrophy: a diagnostic biomarker? Mov Disord. 2020;35:2174–83.
Fanciulli A, Wenning GK. Multiple-system atrophy. N Engl J Med. 2015;372:249–63.
Koga S, Aoki N, Uitti RJ, et al. When DLB, PD, and PSP masquerade as MSA: an autopsy study of 134 patients. Neurology. 2015;85:404–12.
Wenning GK, Geser F, Krismer F, et al. The natural history of multiple system atrophy: a prospective European cohort study. Lancet Neurol. 2013;12:264–74.
Wenning GK, Stankovic I, Vignatelli L, et al. The movement disorder society criteria for the diagnosis of multiple system atrophy. Mov Disord. 2022;37:1131–48.
Gilman S, Wenning GK, Low PA, et al. Second consensus statement on the diagnosis of multiple system atrophy. Neurology. 2008;781:670–6.
Cortelli P, Calandra-Buonaura G, Benarroch EE, et al. Stridor in multiple system atrophy: consensus statement on diagnosis, prognosis, and treatment. Neurology. 2019;93:630–9.
Calandra-Buonaura G, Alfonsi E, Vignatelli L, et al. Dysphagia in multiple system atrophy consensus statement on diagnosis, prognosis and treatment. Parkinsonism Relat Disord. 2021;86:124–32.
Rommel N, Hamdy S. Oropharyngeal dysphagia: manifestations and diagnosis. Nat Rev Gastroenterol Hepatol. 2016;13:49–59.
Tada M, Onodera O, Tada M, et al. Early development of autonomic dysfunction may predict poor prognosis in patients with multiple system atrophy. Arch Neurol. 2007;64:256–60.
Lieto M, Roca A, Bruzzese D. Longitudinal study of a cohort of MSA-C patients in South Italy: survival and clinical features. Neurol Sci. 2019;40:2105–9.
Vogel A, Claus I, Ahring S, et al. Endoscopic characteristics of dysphagia in multiple system atrophy compared to Parkinson’s disease. Mov Disord. 2022;37:535–44.
Higo R, Tayama N, Watanabe T, et al. Videofluoroscopic and manometric evaluation of swallowing function in patients with multiple system atrophy. Ann Otol Rhinol Laryngol. 2003;112:630–6.
Higo R, Nito T, Tayama N. Swallowing function in patients with multiple-system atrophy with a clinical predominance of cerebellar symptoms (MSA-C). Eur Arch Otorhinolaryngol. 2005;262:646–50.
Park A, Jang SJ, Kim NE, et al. Swallowing outcomes following voice therapy in multiple system atrophy with dysphagia: comparison of treatment efficacy with Parkinson’s disease. Dysphagia. 2022;37:198–206.
Umemoto G, Furuya H, Tsuboi Y, et al. Dysphagia in multiple system atrophy of cerebellar and parkinsonian types. J Neurol Neurosci. 2017;8:1.
Do HJ, Seo HG, Lee HH, et al. Progression of oropharyngeal dysphagia in patients with multiple system atrophy. Dysphagia. 2020;35:24–31.
Lee HH, Seo HG, Kim KD, et al. Characteristics of early oropharyngeal dysphagia in patients with multiple system atrophy. Neurodegener Dis. 2018;18:84–90.
Higo R, Tayama N, Watanabe T, et al. Vocal fold motion impairment in patients with multiple system atrophy: evaluation of its relationship with swallowing function. J Neurol Neurosurg Psychiatry. 2003;74:982–4.
Warnecke T, Vogel A, Ahring S, et al. The shaking palsy of the larynx-potential biomarker for multiple system atrophy: a pilot study and literature review. Front Neurol. 2019;10:241.
Rech RS, Baumgarten A, Colvara BC, et al. Association between oropharyngeal dysphagia, oral functionality, and oral sensorimotor alteration. Oral Dis. 2018;24:664–72.
Crary MA, Carnaby-Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86:1516–20.
Battel I, Calvo I, Walshe M. Cross-cultural validation of the italian version of the functional oral intake scale. Folia Phoniatr Logop. 2018;70:117–23.
Ninfa A, Pizzorni N, Eplite A, et al. Validation of the Italian version of the functional oral intake scale (FOIS-It) against fiberoptic endoscopic evaluation of swallowing and nutritional status. Dysphagia. 2022;37:137–47.
Wenning GK, Tison F, Seppi K, et al. Development and validation of the unified multiple system atrophy rating scale (UMSARS). Mov Disord. 2004;19:1391–402.
El Fassi N, Pavy le Traon A, Mouchon E, et al. UMSARS versus laryngoscopy-based assessment of dysphagia. Mov Disord Clin Pract. 2023;10(6):974–9.
Mozzanica F, Pizzorni N, Scarponi L, et al. Mixed consistencies in dysphagic patients: a myth to dispel. Dysphagia. 2022;37:116–24.
Logemann JA, Rademarker AW, Pauloski BR, et al. Normal swallowing physiology viewed by videofluoroscopy and videoendoscopy. Folia Phoniatr Logop. 1998;50:311–9.
Schindler A, Baijens LWJ, Geneid A, et al. Phoniatricians and otorhinolaryngologists approaching oropharyngeal dysphagia: an update on FEES. Eur Arch Otorhinolaryngol. 2022;279:2727–42.
Leder SB, Acton LM, Lisitano HL, et al. Fiberoptic endoscopic evaluation of swallowing (FEES) with and without blue-dyed food. Dysphagia. 2005;20:157–62.
Desuter G. Video-endoscopy by screenplays. In: Desuter G, editor. Oropharyngeal dysphagia. Cham: Springer Nature; 2019. p. 9–41.
Rosenbek JC, Robbins JA, Roecker EB, et al. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Tabor LC, Plowman EK, Romero-Clark C, et al. Oropharyngeal dysphagia profiles in individuals with oculopharyngeal muscular dystrophy. Neurogastroenterol Motil. 2018;30: e13251.
Neubauer PD, Rademaker AW, Leder SB. The yale pharyngeal residue severity rating scale: an anatomically defined and image-based tool. Dysphagia. 2015;30:521–8.
Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull. 1968;70:213–20.
Altman DG. Practical statistics for medical research. London: Chapman and Hall; 1991.
Steele CM, Grace-Martin K. Reflections on clinical and statistical use of the penetration-aspiration scale. Dysphagia. 2017;32:601–16.
Borders JC, Brates D. Use of the penetration-aspiration scale in dysphagia research: a systematic review. Dysphagia. 2020;35:583–97.
Fernagut PO, Vital A, Canron MH, et al. Ambiguous mechanisms of dysphagia in multiple system atrophy. Brain. 2012;135: e205.
Clavé P, de Kraa M, Arreola V, et al. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther. 2006;24:1385–94.
Ueha R, Goto T, Sato T, et al. High resolution manofluorographic study in patients with multiple system atrophy: possible early detection of upper esophageal sphincter and proximal esophageal abnormality. Front Med (Lausanne). 2018;5:286.
Simpson D, Kaufman H, Sanders I, et al. Laryngeal dystonia in multiple system atrophy. Muscle Nerve. 1992;15:1213–5.
Shimohata T, Shinoda H, Nakayama H, et al. Daytime hypoxemia, sleep-disordered breathing, and laryngopharyngeal findings in multiple system atrophy. Arch Neurol. 2007;64:856–61.
Ozawa T, Shinoda H, Tomita M, et al. Tremulous arytenoid movements predict severity of glottic stenosis in multiple system atrophy. Mov Disord. 2010;25:1418–23.
Steele CM, Alsanei WA, Ayanikalath S, et al. The influence of food texture and liquid consistency modification on swallowing physiology and function: a systematic review. Dysphagia. 2015;30:2–26.
Acknowledgements
None.
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by DG, GM, AE and AC, analysis was performed by FA, NP and TW. The first draft of the manuscript was written by FM and AS. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Research Involving Human and Animal Participants
The study was conducted in accordance with the Declaration of Helsinki, and it was previously approved by the Institutional Review Board of H. Sacco Hospital, Milan.
Informed Consent
All the enrolled patients gave their written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mozzanica, F., Pizzorni, N., Eplite, A. et al. Swallowing Characteristics in Patients with Multiple System Atrophy Analyzed Using FEES Examination. Dysphagia 39, 387–397 (2024). https://doi.org/10.1007/s00455-023-10619-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-023-10619-5