Abstract
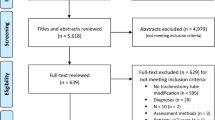
Dysphagia in Robin Sequence can be present in varying degrees, requiring multidisciplinary management and specific swallowing assessment by a specialist. Most studies published to date have evaluated only respiratory outcomes, and the available evidence on the improvement of swallowing is questionable. To conduct a systematic review and meta-analysis of studies evaluating swallowing in children with Robin Sequence before and after airway clearance procedures. The research question was developed based on the PICO strategy. The literature search was performed in electronic databases and gray literature. Studies were selected by 3 independent reviewers. The risk of bias and level of evidence of the studies were assessed. A proportion meta-analysis was performed to calculate the prevalence of dysphagia after airway clearance procedures. The search identified 4938 studies, 5 of which were included. All studies had limitations in terms of design and sample size. The prevalence of dysphagia after airway clearance was obtained by analyzing treatment subgroups: mandibular distraction osteogenesis, mandibular distraction osteogenesis + tracheostomy tube, and nasopharyngeal tube. Clinical and/or instrumental assessment was assessed by a swallowing specialist. The meta-analysis was precluded by the limitations of the studies, especially regarding sample size, which affected the accuracy of the findings. Dysphagia remained unresolved in 55% of children (95% CI 1–99%). The methodological quality of the studies indicated a high risk of bias and very low level of evidence. It was not possible to confirm that airway clearance techniques used in Robin Sequence improve dysphagia.


Similar content being viewed by others
References
Breugem CC, Evans KN, Poets CF, Suri S, Picard A, Filip C, et al. Best practices for the diagnosis and evaluation of infantswith robin sequence a clinical consensus report. JAMA Pediatr. 2016;170:894–902. https://doi.org/10.1001/jamapediatrics.2016.0796.
Côté A, Fanous A, Almajed A, Lacroix Y. Pierre Robin sequence: review of diagnostic and treatment challenges. Int J Pediatr Otorhinolaryngol. 2015;79:451–64. https://doi.org/10.1016/j.ijporl.2015.01.035.
Poets CF, Koos B, Reinert S, Wiechers C. The Tübingen palatal plate approach to Robin sequence: summary of current evidence. J Cranio-Maxillofacial Surg. 2019;47:1699–705. https://doi.org/10.1016/j.jcms.2019.08.002.
Wiechers C, Buchenau W, Arand J, Oertel A-F, Peters K, Müller-Hagedorn S, et al. Mandibular growth in infants with Robin sequence treated with the Tübingen palatal plate. Head Face Med. 2019;15:17. https://doi.org/10.1186/s13005-019-0200-1.
Marques IL, de Sousa TV, Carneiro AF, de Peres SP, Barbieri MA, Bettiol H. Seqüência de Robin: protocolo único de tratamento. J Pediatr. 2005;81:14–22. https://doi.org/10.1590/S0021-75572005000100005.
Nassar E, Marques IL, Trindade ASJ, Bettiol H. Feeding-facilitating techniques for the nursing infant with Robin sequence. Cleft Palate Craniofac J. 2006;43:55–60. https://doi.org/10.1597/04-018.1.
Breik O, If TD, Umapathysivam K, Tivey D, Anderson P. Feeding and reflux in children after mandibular distraction osteogenesis for micrognathia: a systematic review. Int J Pediatr Otorhinolaryngol. 2016;85:128–35. https://doi.org/10.1016/j.ijporl.2016.03.033.
Spring MA, Mount DL. Pediatric feeding disorder and growth decline following mandibular distraction osteogenesis. Plast Reconstr Surg. 2006;118:476–82. https://doi.org/10.1097/01.prs.0000227740.48021.c3.
Harris JA, Caprio RM, Resnick CM. Do infants with Robin sequence have improved feeding and weight gain after mandibular distraction? J Oral Maxillofac Surg. 2021;79:1331–8. https://doi.org/10.1016/j.joms.2021.01.029.
Fayoux P, Daniel SJ, Allen G, Balakrishnan K, Boudewyns A, Cheng A, et al. International Pediatric ORL Group (IPOG) Robin Sequence consensus recommendations. Int J Pediatr Otorhinolaryngol. 2020;130:109855. https://doi.org/10.1016/j.ijporl.2019.109855.
Organização Mundial da Saúde (2008) Classificação internacional de funcionalidade, incapacidade e saúde. Editora da Universidade de São Paulo, São Paulo. https://apps.who.int/iris/bitstream/handle/10665/42407/9788531407840_por.pdf?sequence=111. Accessed 18 May 2022
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions: cochrane book series. New Jersey: Wiley; 2008.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M et al (2021) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. The Ottawa Hospital. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 18 May 2022
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M (2022) Cochrane handbook for systematic reviews of interventions. Version 6.3. 2022. https://handbook-5-1.cochrane.org/chapter_9/9_5_2_identifying_and_measuring_heterogeneity.htm. Accessed 18 May 2022
Van der Plas PPJM, Streppel M, Pullens B, Koudstaal MJ, Mathijssen IMJ, van Heesch GGM, et al. Feeding and swallowing outcomes following mandibular distraction osteogenesis: an analysis of 22 non-isolated paediatric cases. Int J Oral Maxillofac Surg. 2021. https://doi.org/10.1016/j.ijom.2021.11.015.
Marques IL, Prado-Oliveira R, Leirião VHV, Jorge JC, de Souza L. Clinical and fiberoptic endoscopic evaluation of swallowing in Robin sequence treated with nasopharyngeal intubation: the importance of feeding facilitating techniques. Cleft Palate Craniofac J. 2010;47:523–9. https://doi.org/10.1597/09-002.
Monasterio FO, Molina F, Berlanga F, López ME, Ahumada H, Takenaga RH, et al. Swallowing disorders in pierre robin sequence: its correction by distraction. J Craniofac Surg. 2004;15:934–41. https://doi.org/10.1097/00001665-200411000-00009.
Hong P, Brake MK, Cavanagh JP, Bezuhly M, Magit AE. Feeding and mandibular distraction osteogenesis in children with Pierre Robin sequence: a case series of functional outcomes. Int J Pediatr Otorhinolaryngol. 2012;76:414–8. https://doi.org/10.1016/j.ijporl.2011.12.023.
Smith MC, Senders CW. Prognosis of airway obstruction and feeding difficulty in the Robin sequence. Int J Pediatr Otorhinolaryngol. 2006;70:319–24. https://doi.org/10.1016/j.ijporl.2005.07.003.
Lidsky ME, Lander TA, Sidman JD. Resolving feeding difficulties with early airway intervention in Pierre Robin sequence. Laryngoscope. 2008;118:120–3. https://doi.org/10.1097/MLG.0b013e31815667f3.
Glynn F, Fitzgerald D, Earley MJ, Rowley H. Pierre Robin sequence: an institutional experience in the multidisciplinary management of airway, feeding and serous otitis media challenges. Int J Pediatr Otorhinolaryngol. 2011;75:1152–5. https://doi.org/10.1016/j.ijporl.2011.06.009.
McNair C, Campbell-Yeo M, Johnston C, Taddio A. Nonpharmacologic management of pain during common needle puncture procedures in infants: current research evidence and practical considerations: an update. Clin Perinatol. 2019;46:709–30. https://doi.org/10.1016/j.clp.2019.08.006.
Wiechers C, Thjen T, Koos B, Reinert S, Poets CF. Treatment of infants with craniofacial malformations. Arch Dis Child Fetal Neonatal Ed. 2021;106:104–9. https://doi.org/10.1136/archdischild-2019-317890.
Wiechers C, Arand J, Koos B, Poets CF. Evidence and practical aspects of treatment with the Tübingen palatal plate. Semin Fetal Neonatal Med. 2021;26:101281. https://doi.org/10.1016/j.siny.2021.101281.
Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387:475–90. https://doi.org/10.1016/S0140-6736(15)01024-7.
Arvedson J, Clark H, Lazarus C, Schooling T, Frymark T. The effects of oral-motor exercises on swallowing in children: an evidence-based systematic review. Dev Med Child Neurol. 2010;52:1000–13. https://doi.org/10.1111/j.1469-8749.2010.03707.x.
Zhang Y, Lyu T, Hu X, Shi P, Cao Y, Latour JM. Effect of nonnutritive sucking and oral stimulation on feeding performance in preterm infants: a randomized controlled trial. Pediatr Crit Care Med. 2014;15:608–14. https://doi.org/10.1097/PCC.0000000000000182.
Rocha AD, Moreira MEL, Pimenta HP, Ramos JRM, Lucena SL. A randomized study of the efficacy of sensory-motor-oral stimulation and non-nutritive sucking in very low birthweight infant. Early Hum Dev. 2007;83:385–8. https://doi.org/10.1016/j.earlhumdev.2006.08.003.
Pimenta HP, Moreira MEL, Rocha AD, Gomes SC, Pinto LW, Lucena SL. Efeitos da sucção não-nutritiva e da estimulação oral nas taxas de amamentação em recém-nascidos pré-termo de muito baixo peso ao nascer: um ensaio clínico randomizado. J Pediatr. 2008;84:423–7. https://doi.org/10.2223/JPED.1839.
Bache M, Pizon E, Jacobs J, Vaillant M, Lecomte A. Effects of pre-feeding oral stimulation on oral feeding in preterm infants: a randomized clinical trial. Early Hum Dev. 2014;90:125–9. https://doi.org/10.1016/j.earlhumdev.2013.12.011.
da Rosa Pereira K, Levy DS, Procianoy RS, Silveira RC. Impact of a pre-feeding oral stimulation program on first feed attempt in preterm infants: double-blind controlled clinical trial. PLoS ONE. 2020;15:e0237915. https://doi.org/10.1371/journal.pone.0237915.
Acknowledgements
The study was carried out at Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, Rio Grande do Sul, Brazil.
Author information
Authors and Affiliations
Contributions
Study conception and design: MG, MIS, DSL, PJCM. Data acquisition: MG, FLB, LFP. Analysis and data interpretation: MG, RINF, CS, DSL, PJCM. Drafting of the manuscript: MG, DSL, PJCM. Critical revision: MG, FLB, DSL, PJCM. Final approval of the article: MG, FLB, LFP, MIS, RINF, CS, DSL, PJCM. Statistical analysis: MG, RINF, CS, DSL, PJCM. Overall responsibility: MG, FLB, LFP, MIS, RINF, CS, DSL, PJCM. All authors have read and approved the final version of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gasparin, M., Barth, F.L., Pauletti, L.F. et al. Therapeutic Management with Airway Clearance in Children with Robin Sequence and Association with Swallowing Outcomes: A Systematic Review and Meta-analysis. Dysphagia 38, 1267–1276 (2023). https://doi.org/10.1007/s00455-023-10561-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-023-10561-6