Abstract
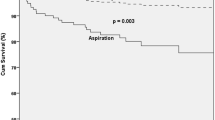
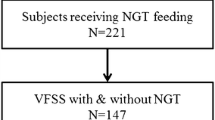
The association between impairments in swallowing safety detected via fiberoptic endoscopic evaluation of swallowing (FEES) and dysphagia complications has been evaluated in small studies that have not allowed obtaining precise estimates of the presence of such an association. The objective of this study was to evaluate the risk of dysphagia complications associated with the detection of premature spillage, residue, penetration, and aspiration via FEES. A systematic review and meta-analysis of the literature were carried out. A search strategy was established using terms of controlled and free vocabulary (free text) in the PubMed, Lilacs, Embase, Medline, and Cochrane databases. The initial search in the databases identified 3545 articles, of which 321 were excluded due to duplication, 3224 were selected for review of titles and abstracts, 45 were selected for full-text review, 37 were excluded for not meeting the selection criteria, and 8 were included for the final analysis, with a total population of 1168 patients. Aspiration increased the risk of pneumonia (OR 2.97, 95% CI 1.52–5.80, P = 0.001). The number of studies that have evaluated the relationship of other FEES findings with dysphagia complications was limited (≤ 3). One study found a higher risk of mortality in patients with aspiration (OR 4.08, 95% CI 1.60–10.27, P = 0.003). Another study that evaluated the risk of mortality in a combined group of penetration and aspiration found no higher risk of mortality. Penetration, residue, and premature spillage were not found to be associated with an increased risk of pneumonia, mortality, or other outcomes. Aspiration demonstrated via FEES was associated with an increased risk of pneumonia and mortality. There is insufficient evidence for the capacity of premature spillage, penetration, and residue to predict dysphagia complications.




Similar content being viewed by others
References
Kertscher B, Speyer R, Fong E, Georgiou AM, Smith M. Prevalence of oropharyngeal dysphagia in the Netherlands: a telephone survey. Dysphagia. 2015;30:114–20. https://doi.org/10.1007/s00455-014-9584-z.
Adkins C, Takakura W, Spiegel BMR, Lu M, Vera-Llonch M, Williams J, Almario CV. Prevalence and characteristics of dysphagia based on a population-based survey. Clin Gastroenterol Hepatol. 2020;18:1970-1979.e1972. https://doi.org/10.1016/j.cgh.2019.10.029.
Takizawa C, Gemmell E, Kenworthy J, Speyer R. A systematic review of the prevalence of oropharyngeal dysphagia in stroke, Parkinson’s disease, Alzheimer’s disease, head injury, and pneumonia. Dysphagia. 2016;31:434–41. https://doi.org/10.1007/s00455-016-9695-9.
Mateos-Nozal J, Montero-Errasquín B, Sánchez García E, Romero Rodríguez E, Cruz-Jentoft AJ. High prevalence of oropharyngeal dysphagia in acutely hospitalized patients aged 80 years and older. J Am Med Dir Assoc. 2020;21:2008–11. https://doi.org/10.1016/j.jamda.2020.04.032.
Cichero JA, Altman KW. Definition, prevalence and burden of oropharyngeal dysphagia: a serious problem among older adults worldwide and the impact on prognosis and hospital resources. Nestle Nutr Inst Workshop Ser. 2012;72:1–11. https://doi.org/10.1159/000339974.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63. https://doi.org/10.1161/01.STR.0000190056.76543.eb.
Ramsey DJ, Smithard DG, Kalra L. Early assessments of dysphagia and aspiration risk in acute stroke patients. Stroke. 2003;34:1252–7. https://doi.org/10.1161/01.STR.0000066309.06490.B8.
Langmore SE, Shatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia. 1988;2:216–9.
Langmore SE, Terpenning MS, Schork A, Chen Y, Murray JT, Lopatin D, Loesche WJ. Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia. 1998;13:69–81.
Logemann JA. Swallowing disorders. Best Pract Res Clin Gastroenterol. 2007;21:563–73. https://doi.org/10.1016/j.bpg.2007.03.006.
Espitalier F, Fanous A, Aviv J, Bassiouny S, Desuter G, Nerurkar N, Postma G, Crevier-Buchman L. International consensus (ICON) on assessment of oropharyngeal dysphagia. Eur Ann Otorhinolaryngol Head Neck Dis. 2018;135:S17-s21. https://doi.org/10.1016/j.anorl.2017.12.009.
Giraldo-Cadavid LF, Leal-Leaño LR, Leon-Basantes GA, Bastidas AR, Garcia R, Ovalle S, Abondano-Garavito JE. Accuracy of endoscopic and videofluoroscopic evaluations of swallowing for oropharyngeal dysphagia. Laryngoscope. 2017;127:2002–10. https://doi.org/10.1002/lary.26419.
Colli A, Fraquelli M, Casazza G, Conte D, Nikolova D, Duca P, Thorlund K, Gluud C. The architecture of diagnostic research: from bench to bedside–research guidelines using liver stiffness as an example. Hepatology (Baltimore, MD). 2014;60:408–18. https://doi.org/10.1002/hep.26948.
Lijmer JG, Leeflang M, Bossuyt PMM. Proposals for a phased evaluation of medical tests. Med Decis Making. 2009;29:E13-21. https://doi.org/10.1177/0272989x09336144.
Schmidt J, Holas M, Halvorson K, Reding M. Videofluoroscopic evidence of aspiration predicts pneumonia and death but not dehydration following stroke. Dysphagia. 1994;9:7–11.
Ding R, Logemann JA. Pneumonia in stroke patients: a retrospective study. Dysphagia. 2000;15:51–7. https://doi.org/10.1007/s004550010001.
Ota K, Saitoh E, Baba M, Sonoda S. The secretion severity rating scale: a potentially useful tool for management of acute-phase fasting stroke patients. J Stroke Cerebrovasc Dis. 2011;20:183–7. https://doi.org/10.1016/j.jstrokecerebrovasdis.2009.11.015.
Takahashi N, Kikutani T, Tamura F, Groher M, Kuboki T. Videoendoscopic assessment of swallowing function to predict the future incidence of pneumonia of the elderly. J Oral Rehabil. 2012;39:429–37. https://doi.org/10.1111/j.1365-2842.2011.02286.x.
Aviv JE. Prospective, randomized outcome study of endoscopy versus modified barium swallow in patients with dysphagia. Laryngoscope. 2000;110:563–74. https://doi.org/10.1097/00005537-200004000-00008.
Centre for Reviews Dissemination (2009) Systematic reviews: CRD's guidance for undertaking reviews in health care. York: University of York. University of York, York. https://www.york.ac.uk/crd/guidance/.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor. Cochrane. www.training.cochrane.org/handbook. 2021
Kuo P, Holloway RH, Nguyen NQ. Current and future techniques in the evaluation of dysphagia. J Gastroenterol Hepatol. 2012;27:873–81. https://doi.org/10.1111/j.1440-1746.2012.07097.x.
Lind CD. Dysphagia: evaluation and treatment. Gastroenterol Clin North Am. 2003;32:553–75.
Langmore SE. Scoring a FEES(R) examination. In: Langmore SE, editor. Endoscopic evaluation and treatment of swallowing disorders. 1st ed. New York: Thieme; 2001. p. 101–43.
Langmore SE, Schatz K, Olson N. Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol. 1991;100:678–81.
Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hrobjartsson A, Kirkham J, Juni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schunemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355: i4919. https://doi.org/10.1136/bmj.i4919.
Sterne JA, Hernán MA, McAleenan A, Reeves BC, Higgins JP (2021) Chapter 25: Assessing risk of bias in a non-randomized study. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor. Cochrane handbook for systematic reviews of interventions version 62 (updated February 2021). Cochrane. www.training.cochrane.org/handbook.
McGuinness LA, Higgins JPT. Risk-of-bias visualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synthesis Methods. 2020;2020:1–7. https://doi.org/10.1002/jrsm.1411.
Higgins J, Deeks JJ, Altman DG, on behalf of the Cochrane Statistical Methods Group. Special topics in statistics. In: Higgins JPT, Green S editor. Cochrane handbook for systematic reviews of interventions, version 5.1.0 [updated March 2011]. The Cochrane Collaboration (2011).
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. https://doi.org/10.1186/s13643-016-0384-4.
Giraldo-Cadavid LF, Pantoja JA, Forero YJ, Gutiérrez HM, Bastidas AR. Aspiration in the fiberoptic endoscopic evaluation of swallowing associated with an increased risk of mortality in a cohort of patients suspected of oropharyngeal dysphagia. Dysphagia. 2020;35:369–77. https://doi.org/10.1007/s00455-019-10036-7.
Imaizumi M, Suzuki T, Ikeda M, Matsuzuka T, Goto A, Omori K. Implementing a flexible endoscopic evaluation of swallowing at elderly care facilities to reveal characteristics of elderly subjects who screened positive for a swallowing disorder. Auris Nasus Larynx. 2020;47:602–8. https://doi.org/10.1016/j.anl.2020.02.004.
Lindner-Pfleghar B, Neugebauer H, Stösser S, Kassubek J, Ludolph A, Dziewas R, Prosiegel M, Riecker A. Management of dysphagia in acute stroke: a prospective study for validation of current recommendations. Nervenarzt. 2017;88:173–9. https://doi.org/10.1007/s00115-016-0271-1.
Masiero S, Pierobon R, Previato C, Gomiero E. Pneumonia in stroke patients with oropharyngeal dysphagia: a six-month follow-up study. Neurol Sci. 2008;29:139–45. https://doi.org/10.1007/s10072-008-0925-2.
Lim SH, Lieu PK, Phua SY, Seshadri R, Venketasubramanian N, Lee SH, Choo PW. Accuracy of bedside clinical methods compared with fiberoptic endoscopic examination of swallowing (FEES) in determining the risk of aspiration in acute stroke patients. Dysphagia. 2001;16:1–6. https://doi.org/10.1007/s004550000038.
Armstrong JR, Mosher BD. Aspiration pneumonia after stroke: intervention and prevention. Neurohospitalist. 2011;1:85–93. https://doi.org/10.1177/1941875210395775.
Gandolfi M, Smania N, Bisoffi G, Squaquara T, Zuccher P, Mazzucco S. Improving post-stroke dysphagia outcomes through a standardized and multidisciplinary protocol: an exploratory cohort study. Dysphagia. 2014;29:704–12. https://doi.org/10.1007/s00455-014-9565-2.
Shanahan TK, Logemann JA, Rademaker AW, Pauloski BR, Kahrilas PJ. Chin-down posture effect on aspiration in dysphagic patients. Arch Phys Med Rehabil. 1993;74:736–9. https://doi.org/10.1016/0003-9993(93)90035-9.
Luk JK, Chan DK (2014) Preventing aspiration pneumonia in older people: do we have the 'know-how'? Hong Kong Med J 20: 421–427. https://doi.org/10.12809/hkmj144251
Caldeira D, Alarcão J, Vaz-Carneiro A, Costa J. Risk of pneumonia associated with use of angiotensin converting enzyme inhibitors and angiotensin receptor blockers: systematic review and meta-analysis. BMJ. 2012;345: e4260. https://doi.org/10.1136/bmj.e4260.
Sarin J, Balasubramaniam R, Corcoran AM, Laudenbach JM, Stoopler ET. Reducing the risk of aspiration pneumonia among elderly patients in long-term care facilities through oral health interventions. J Am Med Dir Assoc. 2008;9:128–35. https://doi.org/10.1016/j.jamda.2007.10.003.
Klompas M, Branson R, Eichenwald EC, Greene LR, Howell MD, Lee G, Magill SS, Maragakis LL, Priebe GP, Speck K, Yokoe DS, Berenholtz SM. Strategies to prevent ventilator-associated pneumonia in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(Suppl 2):S133-154. https://doi.org/10.1017/s0899823x00193894.
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM Jr, Musher DM, Niederman MS, Torres A, Whitney CG. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clin Infect Dis. 2007;44:S27–72.
Logemann JA. Mechanisms of normal and abnormal swallowing. In: Flint PW, Haughey BH, Lund V, Niparko JK, Robbins KT, Thomas JR, Lesperance MM, editors. Cummings: otolaryngology: head & neck surgery. 6th ed. Philadelphia: Elsevier; 2015. p. 1500–6.
Langmore SE, Krisciunas GP, Warner H, White SD, Dvorkin D, Fink D, McNally E, Scheel R, Higgins C, Levitt JE, McKeehan J, Deane S, Siner JM, Vojnik R, Moss M. Abnormalities of aspiration and swallowing function in survivors of acute respiratory failure. Dysphagia. 2021;36:831–41. https://doi.org/10.1007/s00455-020-10199-8.
Farneti D. Pooling score: an endoscopic model for evaluating severity of dysphagia. Acta Otorhinolaryngol Ital. 2008;28:135–40.
Braun T, Juenemann M, Viard M, Meyer M, Reuter I, Prosiegel M, Kaps M, Tanislav C. Adjustment of oral diet based on flexible endoscopic evaluation of swallowing (FEES) in acute stroke patients: a cross-sectional hospital-based registry study. BMC Neurol. 2019;19:282. https://doi.org/10.1186/s12883-019-1499-8.
Lijmer JG, Mol BW, Heisterkamp S, Bonsel GJ, Prins MH, van der Meulen JH, Bossuyt PM. Empirical evidence of design-related bias in studies of diagnostic tests. JAMA. 1999;282:1061–6.
Warnecke T, Teismann I, Oelenberg S, Hamacher C, Ringelstein EB, Schabitz WR, Dziewas R. Towards a basic endoscopic evaluation of swallowing in acute stroke—identification of salient findings by the inexperienced examiner. BMC Med Educ. 2009;9:13. https://doi.org/10.1186/1472-6920-9-13.
Pisegna JM, Borders JC, Kaneoka A, Coster WJ, Leonard R, Langmore SE. Reliability of untrained and experienced raters on FEES: rating overall residue is a simple task. Dysphagia. 2018;33:645–54. https://doi.org/10.1007/s00455-018-9883-x.
Pilz W, Vanbelle S, Kremer B, van Hooren MR, van Becelaere T, Roodenburg N, Baijens LW. Observers’ agreement on measurements in fiberoptic endoscopic evaluation of swallowing. Dysphagia. 2016;31:180–7. https://doi.org/10.1007/s00455-015-9673-7.
Funding
Funding was provided by Universidad de La Sabana.
Author information
Authors and Affiliations
Contributions
LFGC and ARB: study conception and design, material preparation, search strategy, selection of studies, results and statistical analysis, revision and editing of the manuscript. JML, DAGZ, MJAF, LBT: study design, search strategy, selection of studies, data retrieval, and writing of the first manuscript. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical Approval and Informed Consent
Not required for a systematic review (personal, sensitive, or confidential information from participants was not collected).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Giraldo-Cadavid, L.F., Bastidas, A.R., Maldonado-Lancheros, J. et al. Pneumonia, Mortality, and Other Outcomes Associated with Unsafe Swallowing Detected via Fiberoptic Endoscopic Evaluation of Swallowing (FEES) in Patients with Functional Oropharyngeal Dysphagia: A Systematic Review and Meta-analysis. Dysphagia 37, 1662–1672 (2022). https://doi.org/10.1007/s00455-022-10427-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-022-10427-3