Abstract
Objective
To conduct a systematic review and meta-analysis of case–control and cohort human studies evaluating metabolite markers identified using high-throughput metabolomics techniques on esophageal cancer (EC), cancer of the gastroesophageal junction (GEJ), and gastric cancer (GC) in blood and tissue.
Background
Upper gastrointestinal cancers (UGC), predominantly EC, GEJ, and GC, are malignant tumour types with high morbidity and mortality rates. Numerous studies have focused on metabolomic profiling of UGC in recent years. In this systematic review and meta-analysis, we have provided a collective summary of previous findings on metabolites and metabolomic profiling associated with EC, GEJ and GC.
Methods
Following the PRISMA procedure, a systematic search of four databases (Embase, PubMed, MEDLINE, and Web of Science) for molecular epidemiologic studies on the metabolomic profiles of EC, GEJ and GC was conducted and registered at PROSPERO (CRD42023486631). The Newcastle–Ottawa Scale (NOS) was used to benchmark the risk of bias for case-controlled and cohort studies. QUADOMICS, an adaptation of the QUADAS-2 (Quality Assessment of Diagnostic Accuracy) tool, was used to rate diagnostic accuracy studies. Original articles comparing metabolite patterns between patients with and without UGC were included. Two investigators independently completed title and abstract screening, data extraction, and quality evaluation. Meta-analysis was conducted whenever possible. We used a random effects model to investigate the association between metabolite levels and UGC.
Results
A total of 66 original studies involving 7267 patients that met the required criteria were included for review. 169 metabolites were differentially distributed in patients with UGC compared to healthy patients among 44 GC, 9 GEJ, and 25 EC studies including metabolites involved in glycolysis, anaerobic respiration, tricarboxylic acid cycle, and lipid metabolism. Phosphatidylcholines, eicosanoids, and adenosine triphosphate were among the most frequently reported lipids and metabolites of cellular respiration, while BCAA, lysine, and asparagine were among the most commonly reported amino acids. Previously identified lipid metabolites included saturated and unsaturated free fatty acids and ketones. However, the key findings across studies have been inconsistent, possibly due to limited sample sizes and the majority being hospital-based case–control analyses lacking an independent replication group.
Conclusion
Thus far, metabolomic studies have provided new opportunities for screening, etiological factors, and biomarkers for UGC, supporting the potential of applying metabolomic profiling in early cancer diagnosis. According to the results of our meta-analysis especially BCAA and TMAO as well as certain phosphatidylcholines should be implicated into the diagnostic procedure of patients with UGC. We envision that metabolomics will significantly enhance our understanding of the carcinogenesis and progression process of UGC and may eventually facilitate precise oncological and patient-tailored management of UGC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgery of upper gastrointestinal cancers (UGC) such as esophageal cancer (EC), cancer of the gastroesophageal junction (GEJ) and gastric cancer (GC) are still one the most lethal types of cancer worldwide (Jin et al. 2020). Advances in surgical technique and perioperative systemic therapies have made many patients with more advanced disease or co-morbidities candidates for surgery (Bray et al. 2018; Perera et al. 2021; Siegel et al. 2022). In light of these changes, reliable measures that assess preoperative diagnostics, patient-centred outcomes and individualised follow-up tools are more important than ever to establish a precision oncology approach in diagnostics and multimodality therapy (Warburg et al. 1927; Slankamenac et al. 2013). Ideally, these measures will help guide treatment decisions and ensure treatment meets appropriate standards. Early detection and timely treatment following precise risk classification are imperative for improving patient outcomes in GC. The most frequent symptoms of UGC are very unspecific, like dysphagia, nausea, and loss of weight (Heslin, et al. 1997). The primary diagnostic tool is gastroscopy, an invasive procedure allowing tumour detection and biopsy collection in the same procedure (Heiliger et al. 2022). Conventional plasma tumour biomarkers have been proposed as valuable parameters for early detection, prognostic prediction and recurrence monitoring in EC and GC (Emoto et al. 2012). Nonetheless, because of limited specificity and sensitivity, most circulating molecular markers are not recommended for early diagnosis of UGC. Therefore, identification and validation of UGC-specific biomarkers are warranted to facilitate early diagnosis (Gurdasani et al. 2019). It is necessary to observe the progression from precancerous lesions to malignancies, and therefore, identifying diagnostic biomarkers for EC, GEJ, and GC is of great significance. A key feature of tumour cell metabolism is the ability to obtain nutrients from a frequently nutrient-poor microenvironment and utilise these nutrients to meet the demands of growth and proliferation (Lewis et al. 2021). Thereby a tumour microenvironment (TME) is sequentially formed, which comprises cancer cells, the cytokine environment, extracellular matrix, immune cell subsets and other components (Gustafsson et al. 2024). In this complex network of cancer cells and cancer derived metabolites, the pro-tumorigenic vicinity plays a pivotal role in stimulating tumour angiogenesis, promoting its invasiveness and metastatic potential (Berrell 2023). Certain tumour-associated metabolites are associated with aggressive cancer phenotypes, facilitated angiogenesis, promoted mutagenesis and suppress the immune system (Zhang et al. 2023). However, the migration of cancer derived metabolites from the tumour itself, as well as its microenvironment into the systemic blood circulation can be detected and quantified by state-of-the-art clinical mass spectrometry (Zhao et al. 2023).
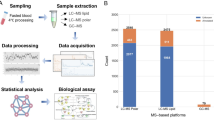
For decades, metabolic reprogramming of tumours was perceived as only increased glycolysis, as postulated by Otto Warburg almost a century ago. This simplistic view has recently been challenged and revised as we realized that tumour metabolism is more heterogeneous than initially assumed (Thompson et al. 2023). The concept of metabolic plasticity has recently emerged as we learned that some tumours are able to switch between alternative metabolic programs to meet challenges exerted by drugs targeted against a particular metabolic pathway or during tumorigenesis (Finley 2023). It is suggested that EC and GC cells may consume a large number of fatty acids to meet the needs of cell membrane synthesis and energy production (Warburg et al. 1927). The survival of cancer cells in the human body depends on lipids, and accumulated lipid droplets are found in various cancer microenvironments (Mikami et al. 2019), so lipid droplets are expected as effective targets for blocking tumour growth (Petan et al. 2018), and fatty acid metabolism-related proteins may also become diagnostic markers for early GC diagnosis and follow-up (Wu et al. 2019; Jiang et al. 2017). In addition, UGC is prone to metastasis, and adipocytes regulate fatty acid oxidation. However, fatty acid oxidation is enhanced in UGC patients, which promotes metastasis in EC, GEJ, and GC (Tsuboi 2019; Tan et al. 2018). The plasma is commonly considered a pool of metabolites and reflects the systemic metabolic regulation in cancer patients (Lopez-Bascon et al. 2016). Multiple methods have been developed for metabolome assessment, including nuclear magnetic resonance spectroscopy (NMR), liquid chromatography (LC), gas chromatography, capillary electrophoresis (CE), and mass spectroscopy (MS). To date, liquid chromatography-tandem mass spectroscopy (LC–MS/MS)-based high throughput techniques are broadly utilised in various compartments, allowing joint assessment of multiple metabolites, only requiring small amounts of biological specimens (Chan et al. 2014).
Respectively, these “omics” technologies enable the study of cancer-related alterations at both a genetic level and at proteomic and metabolomic levels with high sensitivity (Doshi et al. 2023). Among these techniques, metabolomics is a promising approach for cancer biomarker discovery, as the reprogramming of cellular metabolism is one of the hallmarks of cancer, and metabolomics as the endpoint of “omics” cascades could reflect perturbations in all biological activities with an amplified way (Stine et al. 2022). Since the beginning of metabolomic research, guidelines have been defined by the Metabolomics Standards Initiative for data reporting, outlining the minimal information content that should be reported, common syntax, defining the transmission formats that facilitate the exchange of information, and standard semantics (Sumner et al. 2007). Thus, current metabolomic research provides global data on the metabolism of tumours and can also act as a promising tool to discover biomarkers of diagnosis, metastatic surveillance, and prediction of chemotherapeutic sensitivity (Warburg 1956a).
According to The Human Metabolome Database (HMDB), lipids, carbohydrates and amino acids constitute obligate cofactors in mitochondrial fatty acid -oxidation, which represents the major step of energy production and is altered in multiple malignancies (Lu et al. 2019; Wishart, et al. 2022). On the example of lipids, excessive production of acylcarnitines has been shown to reflect altered fatty acid oxidation, contributing to metabolic diseases (Balonov, et al. 2023). In cancer, acylcarnitine metabolism is considered a gridlock to precisely promote metabolic flexibility based on its crucial function in controlling the metabolic processes of glucose and fatty acids (Warburg 1956b). Metabolic reprogramming in malignant cells modulates the production of acylcarnitines of different chain lengths (Kim et al. 2023). This intercalates with other major metabolic pathways, factors and metabolites, resulting in balanced energy production and consumption, as well as in the biosynthesis of metabolic intermediates for fast growth (Liu et al. 2018). However, studies evaluating acylcarnitine profiles associated with EC, GEJ and GC are scarce and inconsistent (Sun et al. 2023). Corona et al. found that plasma acetylcarnitine (C2), hexadecanoylcarnitine (C16) and octadecenoylcarnitine (C18:1) of UGC patients were higher than first-degree relatives (Corona, et al. 2018). A study performed by Lario et al. found that plasma hydroxytetradecadienylcarnitine (C14:2-OH) and octadecanoylcarnitine (C18) were increased in GC patients compared to precursor lesions of gastric cancer (Lario et al. 2017). Therefore, more studies are required to assess metabolic changes in UGC.
Methods
This systematic review was developed, conducted and reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and relevant recommendations; Good Clinical Practice (GCP)-compliant handling of the data is secured by adequate SOPs (Page et al. 2021; Nagendrababu et al. 2020). The review protocol was established before the initiation of the research and registered in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42023486631) (Schiavo 2019).
Literature search strategy
A systematic literature search was conducted using PubMed, Embase, Web of Science, and MEDLINE according to the PRISMA guidelines by two independent investigators (IB and SJ) (Shamseer et al. 2015). All studies published in English through January 2023 were potentially eligible for inclusion. We have performed searches using the keywords (metabolomics OR metabolomic profiling OR metabolomic fingerprinting OR oncomet) AND (gastric cancer OR cancer of the gastroesophageal junction OR esophageal cancer) present in the [Title] or [Title/Abstract], as well as combinations, and limits (humans, adults, English language etc.). The reference list of each article was searched for further relevant literature. Duplicate articles, editorials, and conference abstracts were excluded. The articles were screened and filtered by title and abstract. A full-text assessment and review of the remaining studies was conducted. In the initial screening phase the following criteria have been utilized for filtering:
-
Not population of interest
-
Not entity of interest
-
Relevant outcomes not reported
-
Did not report real patient data, and instead reported Kaplan–Meier survival estimates without real patient survival
The two reviewers independently extracted data from the included articles using double-data extraction. Inconsistencies were resolved by consensus. In the case of disagreement, a third reviewer (CH) was consulted to reach a consensus.
Eligibility criteria
All studies reporting metabolomic profiles in patients 18 years or older who underwent either EC, GEJ or GC surgery for any malignant condition besides sarcoma were considered eligible for inclusion. Studies aiming to find metabolomics characteristics and candidate metabolic biomarkers for diagnosis in EC, GEJ, and GC were included. The study used the PECOS acronym to define the inclusion and exclusion criteria: Population, Exposure, Comparison, Outcome, and Type of Study. Studies that satisfied the requirements established using the PECOS method were included.
PECOS inclusion criteria:
-
P: adult patients (> 18 years of age) from any geographic location or gender
-
E: patients with a confirmed diagnosis of UGC
-
C: difference in the concentration of metabolites between UGC and healthy controls in preoperative plasma samples and intraoperative samples from the tumour and/or adjacent tissue
-
O: dysregulation of metabolite concentrations between the predetermined study groups reported as either mean ± standard deviation, fold change concentration or log fold change concentration
-
S: human-based observational studies (case–control, cohort, or cross-sectional) published since the inception of UGC metabolomics, i.e., January 2004 and January 2023, which used an untargeted or targeted metabolomic technique to quantify metabolite concentration
As well as metabolomics-specific inclusion criteria:
-
studies investigating either human tissues or plasma
-
the use of a detection platform including NMR, GC-MS, LC-MS, UPLC-MS/MS, HPLC-GC/MS-MS, or multiple platforms
-
the names of differential metabolites available for extraction
When duplicated reports were published from the same population, the most recent or most complete publication was included. Studies with pregnant women, children and adolescents, those that addressed a disease other than UGC, review articles, guidelines, letters and editorials were excluded.
Exclusion criteria:
-
Patients diagnosed with neoplasms other than UGC, either in past or present
-
Patients suffering from any chronic systemic illness or on medication for the same
-
components other than metabolites as biomarkers
-
animal or cell-based studies
-
non-observational study designs such as case reports, conference proceedings, and reviews
-
Metabolites quantified other than in concentration, such as field of appearance, retention time, m/z ratio, etc.
-
studies published before January 2004 or after January 2023
-
genomics and proteomics research
-
incomplete data
Data extraction
For all selected articles, information on authors, publication year, sample type, analytical platform, sample size, and differentially distributed metabolites across comparison groups were independently extracted by two investigators (IB and SJ). In addition to individual metabolites, the two investigators independently reviewed findings on alterations in central metabolic pathways associated with upper GI cancers.
We used PubChem (https://pubchem.ncbi.nlm.nih.gov/ (accessed on December 11th 2023)) to search the metabolites needed to convert their units. The quartile and median or interquartile range (IQR) were converted into mean and standard deviation (SD). For median and quartile, we tested the skewness first and applied a new piecewise function based on the sample size.
Das Manuskript sollte eine klare Erläuterung der Bedingungen enthalten, unter denen Studien mit mehreren Versuchsgruppen im Verhältnis zu einer einzigen Kontrollgruppe zusammengeführt werden. Dazu gehören die Kriterien für die Einstufung der Gruppen als experimentell, die Art der Behandlungen oder die Bedingungen der Untergruppen (z. B. pathologisches Staging und Klassifizierung) sowie Strategien für den Umgang mit erheblicher Heterogenität.
When a study matches two or more experimental groups to one control group, the mean and standard deviation of the experimental group are combined. A qualitative analysis was performed to change the direction of metabolites by counting the frequency across the studies.
Data synthesis and meta-analysis
Due to the lack of a standard procedure for meta-analysis of metabolomic data, in this study, we used SPSS software (PASW version 29.0, SPSS Inc. Chicago, IL, USA) as well as the machine learning algorithms Amanida and meta package in R (version: 4.2.2) (Egger et al. 1997). The Amanida and meta package enabled us to perform a meta-analysis of metabolomics data and combine the results of different studies addressing the same question in metabolomics profiles (Llambrich et al. 2022). A list of dysregulated metabolites was obtained from each study, considering the metabolite levels in healthy controls. Then, the input data were provided via text files containing the information of studies, including the identifiers (metabolite names), p values, fold-changes, study sizes, and references. Since different studies used different assessment methods, we used standardised mean difference (SMD) to assess the effect size. SMD was calculated using Cohen’s D. An effect size of 0.2 was considered to have a low effect, whereas 0.4 was a moderate effect, and 0.8 or more was a large effect. Alternatively, the effect measures used to determine the association between UGC and metabolite with the odds ratio (OR), hazard ratio (HR), incidence rate ratio (IRR) and summary relative risk (SRR) with respective 95% confidence intervals (CI). The significance level for this meta-analysis model was 0.05. We used Q statistic and I2 values to test for variability and assess the proportion of total variability due to heterogeneity, respectively. Heterogeneity was considered low, medium, and high, where I2 values of about 25%, 50% and 75% were present. The total amount of heterogeneity was estimated by heterogeneity variance (τ2) (Patti et al. 2012). A combination of weighted p-values, a modification of Fisher’s method, was used to evaluate the significance of a statistical result using the p-value. The fold change was logarithmically transformed (base 2) to reduce methodological bias, in which case the variation is more homogeneous, and the distribution of the sample mean matches a normal distribution. Log-transformed fold change values are averaged with weight by study size. Qualitative data analysis was performed using the vote-counting method. Vote counting involves the overall behaviour of metabolites per study. Votes are assigned as follows: a value of 1 for metabolites that are up-regulated, a value of − 1 for down-regulated, and 0 for no change in behaviour. The total votes for the composition are then added together. Herewith, our model incorporates both within-study and between-study variability (Higgins et al. 2002).
Study quality assessment
According to the recommendation of the Cochrane Collaboration, the Newcastle–Ottawa scale (NOS) was used to determine the risk of bias, assess the overall reliability of the extracted data, and evaluate the methodological quality of the included studies, respectively (Stang 2010; Lin and Chu 2018). The NOS contains eight items (nine scores in total, where 9 indicates that the study meets all nine criteria for quality assessments and 0 indicates that the study does not meet any of the requirements), which fit into three categories: selection (four scores), comparability (two scores), and exposure of a case–control study or outcome of a cohort study (three scores). The articles were classified as “poor”, “fair”, “good”, or “excellent” when achieving scores of 0–3, > 3–6, > 6–8 or > 8–9, respectively (Lo et al. 2014a). Studies with less than five points were classified as having a high risk of bias.
In our study, the diagnostic accuracy and quality assessment of the included studies were reckoned by three reviewers (IB, SJ, and CH). We independently evaluated the quality of all selected articles using the QUADOMICS tool, an adaptation of the QUADAS-2 (Quality Assessment of Diagnostic Accuracy) tool (Lumbreras et al. 2008). To evaluate the quality of studies included in this systematic review, we addressed 16 selected questions for each to assess methodological subheadings used in metabolomic investigations. Each question is either answered “yes” or “no”. The methodologies of studies that achieved 12/16 or more on the QUADOMICS tool were classified as ‘high quality’, whereas those that scored 11/16 or lower were classified as ‘low quality’. For reference, each reviewer was provided with a copy of the QUADOMICS publication (Whiting et al. 2003) and the article evaluating QUADAS-2 and providing some modifications to the items (Whiting et al. 2006). All three researchers met to compare their observations and generate the consensus rating after ten articles had been reviewed, after 30, and finally after all 66; any disagreements were solved by discussion (Long, et al. 2020). The data set supporting the results of meta-analyses presented in this study is available in Supplementary Material.
Results
The results were divided into five parts: (1) PRISMA literature research; (2) characteristics of the included studies for both qualitative (systematic review) and quantitative (meta-analysis) results; (3) systematic review results; (4) quality assurance results for the studies included; and (5) meta-analysis results.
Literature search
The search returned a total of 1509 reports from Embase (571), Web of Science (109), MEDLINE (217) and PubMed (612). A total of 981 studies were identified after de-duplication. Screening by title and abstract led to the exclusion of 866 studies, leaving 115 studies that underwent full-text assessment (Fig. 1). We then excluded studies that were reviews, conference papers, book chapters, short surveys, notes, letters, or editorials. The final list of included investigations for the systematic review (qualitative synthesis) and for quantitative synthesis in the meta-analysis contained 66 studies, which investigated the metabolome of EC or/and GEJ or/and GC and met the criteria of minimum compounds per group and matched groups by age and sex, compound identification, ethics approval, and matrix sample storage.
Characteristics of the included studies
The included records were published between 2004 and 2023, and all were cross-sectional, case–control, or cohort designs reported in English. Non-English articles were excluded from this review. Participants were from Europe, the United States, and Asia. Age and sex were well-matched in most of the studies. The studies were classified according to different sample types, including 41 blood samples and 29 tissue sample studies. All the included studies investigated the metabolome mainly using LC-MS, GC-MS, CE-MS techniques or NMR. The methodological and cohort characteristics of each study are shown in Table 1.
Systematic review
In 66 studies a total of 169 metabolites; 142 in blood samples, and 65 in tissue samples were identified to significantly differentiate patients with UGC from healthy controls. These investigations comprised 7267 samples in total, of whom 3650 were samples from a UGC and 3617 were healthy controls. 12 of the included studies were conducted in Europe, 38 in Asia, and 17 in America. Each study reported the compound name translated to InChIKey with the chemical translation service (http://cts.fiehnlab.ucdavis.edu/batch (accessed on December 11th 2023). These results were compared to match the compound identifiers between articles, as only some authors reported the same compound in the same manner. If the CTS service did not find a compound, a manual search was performed at PubChem (https://pubchem.ncbi.nlm.nih.gov/ (accessed on December 12th 2023)). In most studies, investigators used MS coupled with different chromatography techniques to generate the metabolomic data (n = 51). In 14 studies, an NMR platform was used, and two used a combination of MS and NMR platforms. The monoisotopic mass from all compounds ranged from 31.06 g/mol for methylamine with only one carbon to 859.74 g/mol for phosphatidylcholine (42:0) with 50 carbons. The compounds most repeated in the literature were branched-chain amino acids (BCAA; isoleucine, leucine, and valine) identified by 8 studies. The most repeated compounds in the literature after BCAA were phosphatidylcholines, eicosanoids, and carbohydrates from the tricarboxylic acid cycle. Based on the sample type classification, 97 metabolites showed increased concentrations, 58 showed decreased concentrations, and 14 showed inconsistent concentrations in blood and tissue samples. The details of the qualitative synthesis are given in Supplementary Table 1.
Quality assurance
Quality assurance of the included studies was performed, using the NOS and the QUADOMICS tool for evaluation. The quality assurance results are shown in Figs. 2, 3, and 4. Variables were based on the experimental methodology.
In case–control studies, the most reported domains were in “Same method of ascertainment for cases and controls”, “Ascertainment of exposure”, and “non-Response rate”, with more than 90% of studies reporting complete information. On the other hand, the least reported domains were in “Selection of Controls” and “Representativeness of the cases”, where less than 60% of the studies disclosed complete information.
In contrast to case–control studies, cohort studies reported the most domains in “Adequacy of follow up of cohorts”, “Was follow-up long enough for outcomes to occur”, and “Assessment of outcome”, with more than 90% of studies reporting complete information. The least reported domains were in “Selection of the non-exposed cohort” and “Ascertainment of exposure”, where less than 60% of the studies disclosed complete information.
As a summary, of the 66 cross-sectional studies, 54 attained a NOS score of 6 or higher (“good” or “excellent”; thus, moderate to low risk of bias). We deemed 12 studies to have a relatively high risk of bias (NOS score: < 6) because of their small and unjustified sample size and lack of statistical adjustments for confounding factors. However, excluding this study did not alter our risk estimate.
According to QUADOMICS, we conducted a quality assessment process (see the score in Fig. 4). The general characteristics of the selected studies and methodological quality assessment were independently checked by IB, SJ and CH.
The quality assessment process following the QUADOMICS tool is summarised in Supplementary Table 1. 6 of the 66 studies were classified as ‘low quality’, fulfilling fewer than 12 of the 16 criteria. The most common problems were not reporting the justification, sample size calculation, and the number of non-respondents. Although the funnel plot was asymmetric on visual inspection, and a potential publication bias was also found in Egger’s test (p = 0.006, Supplementary Table 1), the effect size was not significantly changed after the trim-and-fill (OR = 1.12, 95%CI [1.01, 1.25], p < 0.05, number of trim and fill = 4), thus indicating that the publication bias had little influence on the results. The complete appraisal of the methodological quality of the articles is described in Supplementary Table 1.
Meta-analysis
Statistical analysis was performed for those groups of studies that reported the p values and fold-changes for significant compounds. Overall, we extracted the relative risk estimates for meta-analysis from a total of 169 metabolites from 66 studies. Among these, 155 metabolites were found to be significantly altered in healthy and tumour tissue by meta-analysis, while 14 were not. The forest plots for different metabolites between UGC and healthy controls and the meta-analysis results for different metabolites among UGC and controls are shown in Figs. 5, 6, 7, 8, 9, 10, 11, 12, 13 clustered in their respective biochemical classes.
Forest plot of pooled estimates of UGC associated per study-specific difference in each amino acid from case–control and cohort studies. Overall estimates were obtained from forest plots and random-effects meta-analysis of studies evaluating metabolites and incidence of UGC. Estimates were derived from the most fully adjusted model in each included analysis. Closed squares and horizontal bars represent the Summary relative risk (SRR) with corresponding 95% CIs
Forest plot of pooled estimates of UGC associated per study-specific difference in each metabolite from citrate cycle from case–control and cohort studies. Overall estimates were obtained from forest plots and random-effects meta-analysis of studies evaluating metabolites and incidence of UGC. Estimates were derived from the most fully adjusted model in each included analysis. Closed squares and horizontal bars represent the Summary relative risk (SRR) with corresponding 95% CIs
Forest plot of pooled estimates of UGC associated per study-specific difference in each metabolite from case–control and cohort studies. Overall estimates were obtained from forest plots and random-effects meta-analysis of studies evaluating metabolites and incidence of UGC. Estimates were derived from the most fully adjusted model in each included analysis. Closed squares and horizontal bars represent the Summary relative risk (SRR) with corresponding 95% CIs
Forest plot of pooled estimates of UGC associated per study-specific difference in each metabolite from purine and pyrimidine metabolism from case–control and cohort studies. Overall estimates were obtained from forest plots and random-effects meta-analysis of studies evaluating metabolites and incidence of UGC. Estimates were derived from the most fully adjusted model in each included analysis. Closed squares and horizontal bars represent the Summary relative risk (SRR) with corresponding 95% CIs
Forest plot of pooled estimates of UGC associated per study-specific difference in each metabolite from urea cycle from case–control and cohort studies. Overall estimates were obtained from forest plots and random-effects meta-analysis of studies evaluating metabolites and incidence of UGC. Estimates were derived from the most fully adjusted model in each included analysis. Closed squares and horizontal bars represent the Summary relative risk (SRR) with corresponding 95% CIs
Forest plot of pooled estimates of UGC associated per study-specific difference in each sphingolipid from case–control and cohort studies. Overall estimates were obtained from forest plots and random-effects meta-analysis of studies evaluating metabolites and incidence of UGC. Estimates were derived from the most fully adjusted model in each included analysis. Closed squares and horizontal bars represent the Summary relative risk (SRR) with corresponding 95% CIs
Forest plot of pooled estimates of UGC associated per study-specific difference in each fatty acid from case–control and cohort studies. Overall estimates were obtained from forest plots and random-effects meta-analysis of studies evaluating metabolites and incidence of UGC. Estimates were derived from the most fully adjusted model in each included analysis. Closed squares and horizontal bars represent the Summary relative risk (SRR) with corresponding 95% CIs
Forest plot of pooled estimates of UGC associated per study-specific difference in each bile acid from case–control and cohort studies. Overall estimates were obtained from forest plots and random-effects meta-analysis of studies evaluating metabolites and incidence of UGC. Estimates were derived from the most fully adjusted model in each included analysis. Closed squares and horizontal bars represent the Summary relative risk (SRR) with corresponding 95% Cis
Forest plot of pooled estimates of UGC associated per study-specific difference in each metabolite from case–control and cohort studies. Overall estimates were obtained from forest plots and random-effects meta-analysis of studies evaluating metabolites and incidence of UGC. Estimates were derived from the most fully adjusted model in each included analysis. Closed squares and horizontal bars represent the Summary relative risk (SRR) with corresponding 95% CIs
Amino acids
We performed a meta-analysis for 20 proteinogenic amino acids (Fig. 5 and Supplementary Table 1); 19 showed altered concentrations between patients with UGC and healthy controls (FDR-corrected P < 0.05) in tumour tissue and plasma. In accordance with Cohen's effect size, five metabolites were identified in the meta-analysis that exhibited both a significant difference between the cohorts and at least a moderate effect. Among these are higher circulating levels of branched-chain amino acids (BCAA, isoleucine, leucine, valine) (SRR 0.44 for leucine [95% CI 0.38–0.49], 0.44 for valine [95% CI 0.39–0.50], and 0.35 for isoleucine [95% CI 0.30–0.41]), were associated (FDR-corrected P < 0.05) with UGC. Also, lysine was associated with UGC (SRR 0.44 [95% CI 0.39–0.50]). An inverse association was observed for asparagine and UGC (SRR -0.50 [95% CI – 0.56 to – 0.45]). Decreased concentrations of glutamine were also linked to UGC (SRR -0.20 [95% CI – 0.25 to – 0.14]).
Carbohydrates and tricarboxylic acid cycle
In total, 17 carbohydrates and tricarboxylic acid cycle (TCA) metabolites in tumour tissue and plasma were included in the meta-analysis (Fig. 6 and Supplementary Table 1), and 13 of them were associated with UGC (FDR-corrected P < 0.05). In accordance with Cohen’s effect size, three metabolites were identified in the meta-analysis that exhibited both a significant difference between the cohorts and at least a moderate effect. For these metabolites, we found that notably higher flavin adenine dinucleotide (FAD) (SRR 1.10 [95% CI 1.04–1.16]) and Acetyl-CoA (SRR 1.12 [95% CI 1.06–1.19]) levels were associated with UGC. One metabolite from the citrate cycle, aconitate (SRR – 0.45 [95% CI – 0.51 to – 0.39]), was inversely associated with UGC.
Glycerophospholipids
In the biochemically heterogenous group of 54 glycerophospholipids and their direct derivates, we found 43 of them to be significantly associated with UGC (FDR-corrected P < 0.05) in tumour tissue and plasma (Fig. 7 and Supplementary Table 1). In accordance with Cohen's effect size, several metabolites were identified in the meta-analysis that exhibited both a significant difference between the cohorts and at least a moderate effect. Within the group of acylcarnitines, especially short- to medium-chain acyls, e.g., C2 (SRR -0.70 [95% CI – 0.77 to – 0.62]), C6 (SRR – 0.43 [95% CI – 0.51 to – 0.36]), and C16-OH (SRR -0.34 [95% CI – 0.42 to – 0.27]) resulted in having an inverse association with UGC. No metabolites resulted in a definitive association with UGC in the biochemical group of lysophosphatidylcholines. However, long-chained phosphatidylcholines, exemplary PC (18:1/18:1) (SRR – 0.44 [95% CI – 0.52 to – 0.37]) showed an inverse association with UGC. In Summary, these results indicate that the constellation of phosphatidylcholines, the main constituents of the cell membrane, distinctly differs between healthy cells of the upper gastrointestinal tract and tumour tissue from patients with UGC.
Purine and pyrimidine metabolism
Regarding purines and pyrimidines, essential metabolites of nucleotide metabolism, our meta-analysis resulted in 11 compounds associated with UGC in tumour tissue and plasma (Fig. 8 and Supplementary Table 1). In accordance with Cohen's effect size, five metabolites were identified in the meta-analysis that exhibited both a significant difference between the cohorts and at least a moderate effect. Higher levels of one were associated (FDR-corrected P < 0.05) with UGC. In particular, ATP (SRR – 0.73 [95% CI – 0.82 to – 0.64]) was inversely associated with UGC. However, adenosine, a nucleoside composed of adenine and D-ribose, was associated with UGC (SRR 0.83 [95% CI 0.74–0.92]).
Urea cycle
In the meta-analysis for metabolites involved in the urea cycle, six out of nine metabolites were significantly associated (FDR-corrected P < 0.05) with UGC in tumour tissue and plasma (Fig. 9 and Supplementary Table 1). In accordance with Cohen's effect size, six metabolites were identified in the meta-analysis that exhibited both a significant difference between the cohorts and at least a moderate effect. No definitive inverse associations with UGC were found for metabolites and derivates from the urea cycle. However, all six metabolites showed a direct association with UGC. Especially citrulline, also produced from arginine as a by-product, was associated with UGC (SRR 0.36 [95% CI 0.29–0.44]).
Sphingolipids
Analysing sphingolipids (SM), we found seven SMs in tumour tissue and plasma, of which one was significantly (FDR corrected P < 0.05) associated with UGC and four were inversely associated with UGC (Fig. 10 and Supplementary Table 1). In accordance with Cohen's effect size, sphinganine was identified in the meta-analysis to exhibit both a significant difference between the cohorts and at least a moderate effect. The inverse association with UGC was observed for sphinganine (SRR 0.03 [95% CI – 0.06 to 0.12]). Among the remaining sphingolipids especially SM (OH) 22:1, a sphingolipid in the membranous myelin sheath which surrounds some nerve cell axons, inversely associated with UGC (SRR -0.62 [95% CI – 0.71 to – 0.53]).
Non-esterified fatty acids
Among six non-esterified fatty acids included in the meta-analysis (Fig. 11 and Supplementary Table 1), two were associated with UGC, and three were inversely associated with UGC (FDR corrected P < 0.05) in tumour tissue and plasma. In accordance with Cohen’s effect size, two metabolites were identified in the meta-analysis that exhibited both a significant difference between the cohorts and at least a moderate effect. Linoleic acid (SRR 0.53 [95% CI 0.46–0.60]), a doubly unsaturated essential fatty acid, also known as an omega-6 fatty acid, was the fatty acid found to be associated the most with UGC, and linolenic acid an omega-3 fatty acids were inversely associated with UGC (SRR -0.22 [95% CI – 0.29 to – 0.16]).
Bile acid
Among seven bile acids included in the meta-analysis (Fig. 12 and Supplementary Table 1), only two levels were associated (FDR-corrected P < 0.05) with UGC in tumour tissue and plasma. In accordance with Cohen's effect size, two metabolites were identified in the meta-analysis that exhibited both a significant difference between the cohorts and at least a moderate effect. Both of them, hyocholic acid (HCA) (SRR – 0.28 [95% CI – 0.53 to – 0.03]) and hyodeoxycholic acid (HDCA) (SRR -0.39 [95% CI – 0.64– – 0.14]) resulted in inverse association with UGC.
Biogenic amines and related
Among 42 biogenic amines and related included in the meta-analysis (Fig. 13 and Supplementary Table 1), 38 levels were associated with a UGC in tumour tissue and plasma (FDR-corrected P < 0.05). In accordance with Cohen's effect size, several metabolites were identified in the meta-analysis that exhibited both a significant difference between the cohorts and at least a moderate effect. Within this biochemically heterogeneous group of metabolites, erythrose-4-phosphate (SRR – 0.59 [95% CI – 0.66 to – 0.52]), a monosaccharide comprising a phosphate group linked to the carbohydrate unit as well as putrescine a polyamine produced by the breakdown of amino acids were associated with UGC (SRR 0.65 [95% CI 0.58–0.72]).
Interestingly, Trimethylamine N-oxide (TMAO) (SRR 0.46 [95% CI 0.39–0.53]), a metabolite frequently reported to be associated with esophageal cancer, cancer of the gastroesophageal junction and gastric cancer, was associated relatively marginal in our meta-analysis.
In summary, meta-analysis for the most significant compounds in EC, GEJ, and GC vs control comparison, including the healthy average concentrations (extracted from the human metabolome database) and the projected UGC concentrations in tumour tissue and plasma, resulted in several metabolites directly or inversely associated with the risk of UGC as demonstrated in Table 2. The results showed that patients with UGC compared to healthy controls especially had increased concentrations of BCAA, lysine, FAD, Acetyl-CoA, adenosine, citrulline, sphinganine, linoleic acid, putrescine, and TMAO as well as decreased concentration of asparagine, glutamine, aconitate, short-chain acylcarnitines, ATP, SM (OH) 22:1, linolenic acid, HCA, HDCA, and erythrose-4-phosphate. However, 44 out of 169 metabolites showed no significant association between patients with UGC and healthy controls through the included studies. Substantial heterogeneity (I2 > 50%, s2 > 0.1) was observed for some metabolites. Thus, the majority of metabolites that have been identified show inconsistent results in different studies in terms of relative abundance in the cancer versus control groups.
Discussion
Several metabolites delineated in this study were found to be significantly dysregulated in the local tumour tissue of patients with UGC as well as systemically in patients’ blood compared to healthy controls. The altered metabolites in UGC can be categorised into four main biochemical classes which affect precise oncological and patient-tailored management of UGC: carbohydrates, amino acids, lipids and nucleic acids. These classes can be again separated into several specific sub-categories considering their importance in the general cancer metabolism as well as the particular metabolism of UGC.
Carbohydrates and metabolites of the tricarboxylic acid cycle
The glucose metabolism in esophageal- and gastric cancer cells is augmented differently from that of the normal gastric epithelium (Finley 2023). According to the Warburg effect, cancer cells support their growth primarily by generating energy via the anaerobic catabolism of glucose which implies the tumour microenvironment, in contrast to the oxidative catabolism of pyruvate in healthy cells (Warburg 1956a; Crabtree 1929). The accumulated lactic acid provides an acidic microenvironment that exacerbates the decomposition of the extracellular matrix by proteolytic activity (Bartman 2023; Lyssiotis and Cantley 2014). Several metabolites involved in cellular respiration, including lactic acid, glucose, citrate, and fumaric acid, have been frequently reported, but these results are inconsistent across studies (Cui et al. 2023; Bose et al. 2021). Moreover, opposite associations of some metabolites with UGI cancers are documented by different research groups (Matsumoto et al. 2023; Li et al. 2022; Wang et al. 2020; Wang et al. 2017; Hur et al. 2014; Ikeda et al. 2012). To our understanding, it has been reported that accumulated lactic acid moderates the activity of proteases that decompose extracellular matrix, which can produce some peptides and amino acids that are consumable for energy generation (Smyth et al. 2020; Stier et al. 2020). Acidosis microenvironment is also ascribed to the formation of cancer blood vessels, meeting the plentiful supply of nutrients and leading to tumour invasion and metastasis (Thompson et al. 2023). The contributions of these mechanistic alterations in aerobic glycolysis are crucial for understanding gastric carcinogenesis and progression (Warburg et al. 1927; Bartman et al. 2023).
Our review found ATP to be systemically decreased in patients with UGC. Because mitochondria are the primary source of ATP production, ATP is paramount in linking cancer cell metabolism and bioenergetics in the TME (Yuneva 2008). However, the hypoxic environment in cancer cells triggers the release of ATP. The in vivo measurement of extracellular ATP concentrations using e.g. cell surface–targeted luciferase revealed the ability of solid tumours to maintain peritumoral ATP within the range of 10–5 – 10–4 mol/l, which is much higher than the concentration of this nucleotide detected in the interstitium of healthy tissues and TME (Virgilio et al. 2018) (Marchi et al. 2019). However, because tumour cells can efficiently scavenge nucleotides, they uniquely contribute to the rapid termination of proinflammatory effects of ATP within the metabolically abnormal TME (Galon and Bruni 2019). Only the past decade has brought advances in our understanding of the complexity of mechanisms determining the duration and magnitude of purinergic signalling.
Amino acids
Amino acids are building blocks required for cellular protein biosynthesis and cytoskeleton formation, while elevated levels of amino acids in the TME are contributing aspects in carcinogenesis (Finley 2023). Alterations in essential and non-essential proteinogenic amino acids were reported for UGI cancers (Fig. 5). The availability of amino acids is pivotal for cellular protein biosynthesis and cytoskeleton formation. At the same time, it has been pointed out that amino acids, especially those linked to TCA, are an alternative energy source of cancer cell proliferation (Smyth et al. 2020). Among them, the metabolic networks of all amino acids are complex and highly interconnected with other pathways.
Increased BCAA were consistently detected in studies on GC based on tissue and plasma samples, while inconsistent findings were obtained from studies on EC and GEJ. Several studies additionally reported altered levels of primary derivatives of amino acids in UGI cancers. Our review found significantly decreased levels of glutamine, a non-essential amino acid, in almost all studies (Faubert et al. 2014). Previous investigations delineated that metabolic regulations meet the high glutamine demand of proliferating tumour cells, which supports tumour growth by facilitating both energy production and the biosynthesis of building materials (Geldermalsen et al. 2016). However, BCAAs were found to be systemically increased in patients with UGC. Most amino acids are catabolised in the liver, except BCAAs. The liver has an active branched-chain ketodehydrogenase (BCKDH) to facilitate the consumption of branched-chain ketoacids (BCKA) for gluconeogenesis or fatty acid synthesis but is deficient in branched-chain amino acid aminotransferase (BCAT), the initiator of BCAA breakdown (Neinast et al. 2019). High BCAA levels may inhibit glucose metabolism, and, in turn, high glucose levels may inhibit BCAA degradation (Shao et al. 2018). Hence, abnormal amino acid metabolism has diverse and critical roles in various cancers, and the potential impact of metabolic control and regulation in the tumour microenvironment is becoming increasingly important (Sivanand and Vander Heiden 2020).
Nucleic acids
Tumour cells are in a state of such rapid proliferation and differentiation that frequent nucleotide synthesis and metabolism are upregulated significantly. Higher uric acid or urate levels characterise accumulation of the end products of nucleotide catabolism in patients with esophageal- or gastric cancer (Wang, et al. 2021). Several studies focused on metabolites of nucleotides associated with GC and EC. However, direct evidence on the metabolic pathways of nucleotides related to UGI cancers is still unavailable (Virgilio et al. 2018). In our review, ATP has been identified to be significantly decreased in patients with UGC compared to healthy controls. The involved pathways have been delineated previously (Marchi et al. 2019).
Lipids
The notable feature of lipid metabolism in cancer cells is an increased rate of lipogenesis and the upregulation of mitochondrial fatty acid β-oxidation. At this juncture, fatty acid oxidation provides a major energy source because complete oxidation of one 16-carbon fatty acid could generate 129 ATP molecules compared with the 38 generated from one glucose molecule (Lee et al. 2019b). Especially gastric cancer shows a similar tendency and presents typical changes regarding various metabolites involved in lipid metabolism (Lien et al. 2021). The main classes of lipids of the cell membrane, including fatty acyls, glycerophospholipids, sphingolipids, and sterols, feature their very own structure and function in the cellular membrane (Yang et al. 2022b). Respectively, the recent state of research for each biochemical class has to be delineated separately.
Fatty acyls
Fatty acyls represent the most fundamental category of lipids. Primarily present in esterified form with glycerol, cholesterol or other lipid components, fatty acids are carboxylic acids, often with long, unbranched aliphatic chains of diverse lengths (Nguyen et al. 2014). Fatty acids are categorised as saturated (no carbon–carbon double bonds in the aliphatic chain) and unsaturated with one (monounsaturated fatty acid (MUFA)) or more double bonds (polyunsaturated fatty acid-(PUFA)) (Nomura et al. 2010). The human body can synthesise many of these fatty acids, except some essential fatty acids, including linoleic acid (omega-6 PUFA) and alpha-linolenic acid (omega-3 PUFA) (Shaw and Wolfe 1987). These two PUFAs are precursors for other omega-6 and omega-3 PUFAs that play crucial roles in regulating lipid metabolism and atherosclerosis. In our study, linoleic acid, a doubly unsaturated essential fatty acid, also known as an omega-6 fatty acid, was the fatty acid found to be associated the most with higher UGC risk, and linolenic acid, an omega-3 fatty acid, was associated with lower UGC risk. These characteristics have been described previously and are hence, consistent with the results of our investigation (Huerta-Yepez et al. 2016). However, the antitumor effect of omega-3 PUFAs and the tumour-promoting effect of omega-6 PUFAs are complex processes involving multiple factors and levels. They are interrelated, and there are still many issues to be elucidated (Lee et al. 2020).
Glycerophospholipids
As the main subclass of phospholipids, glycerophospholipids are diacylglycerides with a phosphatidyl ester attached to the terminal carbon. The terminal ester groups are mainly ethanolamine (phosphatidylethanolamine; PE), choline (phosphatidylcholine; PC), serine (Phosphatidylserine; PS) or inositol (Phosphatidylinositol; PI) (Huybrechts, et al. 2023). In addition, several fatty acids with varying lengths and unsaturation could attach to the remaining hydroxyl groups of glycerol via either acyl-, alkyl-, or alkenyl bonds. Hydrolysis of one of the fatty acids of the phospholipids by phospholipase A2 (PLA2) generates respective lysophospholipids, adding to the diversity of the lipid pool (Behuria et al. 2022). Glycerophospholipids are the major structural component of cell membranes and are involved in various biological processes, including inflammation (Cheng et al. 2016). In the present investigation, especially phosphatidylethanolamines of different lengths have been identified to be associated with a higher risk of UGC. Our findings on alterations in PE are consistent with previous studies (Tsai et al. 2018). Furthermore, the emerging research on lipid metabolism in UGC revealed higher PC, PI and PS levels in patients with UGC compared to healthy controls (Luo et al. 2017). In Summary, these results indicate that the constellation of phosphatidylcholines, the main constituents of the cell membrane, distinctly differs between healthy cells of the upper gastrointestinal tract and tumour tissue from patients with UGC. According to the results of our meta-analysis certain phosphatidylcholines should be implicated into the diagnostic procedure of patients with UGC. At this point an investigation of the relevance of phosphatidylcholines in certain stages of the oncological treatment should be performed at pace.
Sphingolipids
Sphingolipids are a wide range of complex lipids defined by an 18-carbon sphingoid base, usually sphingosine (SPH), found in the outer leaflet of cell membranes and in the membranous myelin sheath, which surrounds axons (Behuria et al. 2022). Condensation of SPH and free fatty acid generates the simplest sphingolipids, ceramides which function as precursors for complex sphingolipids produced by the modification of hydroxyl group with phosphocholine (in sphingomyelins) or carbohydrates (in gangliosides) (Janneh and Ogretmen 2022). Sphingolipids constitute hundreds of species originating from the combinations of varying sphingoid bases, various fatty acids that can attach to the bases and numerous carbohydrates in gangliosides. Ceramide regulates numerous cellular processes, such as proliferation, differentiation, and cell signalling (Ogretmen 2018; Zhu, et al. 2023). In UGC, there is a noticeably increased rate of lipogenesis and the upregulation of mitochondrial fatty acid β-oxidation utilising the sphingolipids to meet the demand of cell membrane synthesis, mainly for lipid raft and lipid-modified signalling molecules. The intensive fatty acid degradation via β-oxidation causes significantly larger build-ups of sphingomyelins and gangliosides in cancer tissues (Taniguchi and Okazaki 2021). Notably, in esophageal and gastric cancer tissue, there is some evidence that there are also sphingomyelins in the inner leaflet of the membrane. In addition, the overall accelerated lipid metabolism might explain the severe weight loss observed in patients with late stages of UGC (Benedetti et al. 2023). Sphinganine, a sphingoid base lipid molecule, has been identified to be increased in patients with UGC, while SM (OH) 22:1, a sphingolipid implicated in the initiation of carcinogenesis and promotion of metastasis, has been identified to be decreased in our meta-analysis. Hence, these results indicate an inconsistency in the literature (Tallima et al. 2021).
Bile acids
Bile acids are physiological detergents that facilitate the excretion, absorption, and transport of fats and sterols in the intestine and liver, derived from catabolism of cholesterol (Fu et al. 2021). Previously, bile reflux has been shown to be an independent risk factor for precancerous gastric lesions and GC (Zhang et al. 2021). Especially, HCA a primary bile acid and HDCA, a secondary bile acid, play a crucial role in regulating energy expenditure and were both identified to be decreased in patients with UGC (Pan et al. 2022). However, our results are inconsistent with previous literature as multiple authors described primary bile acids to be reduced and secondary bile acids to be increased in patients with UGC (Rezen et al. 2022).
Biogenic amines and related
Biogenic amines are mainly produced by the breakdown or transformation of amino acids, typically containing one or more amino groups. As such, they comprise a wide range of very heterogeneous metabolites involved in various cellular processes (Fernandez-Reina et al. 2018). A much-discussed metabolite which has been demonstrated to be a prerequisite for cell proliferation to occur is Trimethylamine N-oxide (TMAO). There is evidence suggesting that higher levels of TMAO and its precursors in blood can indicate either a higher risk of malignancy or its presence (Stonans, et al. 2023). TMAO is anticipated to have significance as a biomarker of—or even an independent risk factor for UGC (Oellgaard et al. 2017). More studies confirmed the association of microbiota with TMAO production, resulting in higher risk of colorectal, breast, and gastric cancer (Khodabakhshi et al. 2023). Another metabolite in this heterogenous field is the polyamine putrescine, a polycationic alkylamine commonly found in all living cells and essential for cellular growth and survival. Physiologically, it is sequentially synthesised from the catabolism of the amino acids L-arginine and L-methionine (Janne et al. 2004). However, the putrescine concentrations were significantly increased in patients with UGC and their TME compared to the adjacent normal gastric mucosa from the same individuals (McNamara et al. 2021). Respectively, with the inhibition of the growth of human gastric tumour; putrescine levels were significantly decreased in the tumour tissue (Xie et al. 2023). Consistent with previous findings, we found both TMAO and putrescine to be significantly increased in patients with UGC.
The majority of metabolites that have been identified show inconsistent results in different studies in terms of relative abundance in the cancer and its microenvironment versus control groups. Accordingly, it infers that cancer cells gain growth superiority over their regular counterparts by switching metabolic energy patterns to anaerobic glycolysis and possibly fumarate respiration instead of securing more ATP. These studies, including ours, collectively support that understanding the metabolic risk of many malignancies, including esophageal cancer, cancer of the gastroesophageal junction, and gastric cancer, could improve the development of precise oncological and patient-tailored management of UGC (Han and Lee 2024). Overall, these data justify the evaluation of existing models of amino acid, lipid, carbohydrates and nucleic acid metabolism and their role in tumour growth, metastasis, and immunosurveillance. The measurement of soluble and exosomal activities in the blood of cancer patients might represent a compelling addition to the ‘liquid biopsy’ arsenal (Jaras et al. 2023). Although the described literature reports elevated levels of several oncometabolites such as acetylcarnitine (C2), hexadecanoylcarnitine (C16), octadecenoylcarnitine (C18:1), hydroxytetradecadienylcarnitine (C14:2–OH), and octadecanoylcarnitine (C18) in patients with UGC, our comprehensive meta-analysis encompassing a larger dataset did not corroborate these findings. This discrepancy suggests a need for further investigation to reconcile these conflicting results and to understand the underlying factors contributing to these differences (Corona, et al. 2018; Lario et al. 2017).
Strengths and limitations
To the best of our knowledge, our study provides the most comprehensive meta-evidence on the associations of single metabolites with UGC. This systematic review’s particular strength is the large number of included studies conducted in different populations and the adoption of metabolomics profiling using various biospecimens and analytic techniques. We have performed meta-analysis for a large number of metabolites to facilitate the development of precise oncological and patient-tailored management of UGC. Narrowing the review’s focus to studies with open-access data allowed us to limit the influence of reverse causality and selection bias, and most of the included studies were evaluated to be of high quality.
There are several limitations to be considered. First, our search covered only four databases. However, relevant studies are usually indexed in those databases. Second, the majority of metabolites for which we performed meta-analysis showed considerable between-study heterogeneity and resulted in inconsistent results in our meta-analysis. Possible reasons why certain oncometabolites show inconsistent results may lie both in the pre-analysis and in the analysis of the respective study. The metabolites ATP, UTP and NADH, for example, reflect metabolites that can be measured in different concentrations even when there are small differences in the pre-analytical procedures, such as different biopsy sampling or lyophilization due to the energetic instability of the cells after biopsy sampling (Jang et al. 2018; Tomita et al. 2012). Third, the observational nature of the studies included in the meta-analysis impedes inferences about potential causal mechanisms underlying the observed UGC associations or the histology of particular UGC such as the differentiation of GC in adenocarcinoma and signet-cell carcinoma. Forth, in this meta-analysis, only metabolites were considered that exhibited a relevant difference between tumor patients and healthy controls both in local tumor tissue and systemically in blood plasma and can therefore actually be classified as oncometabolites. However, the investigation was not subdivided into the separate entities of UGCs. In this respect, a further limitation of the study is that metabolites that are exclusively elevated locally in tumor tissue or exclusively elevated systemically in blood plasma were not investigated in detail. Nevertheless, a subgroup analysis of metabolites that are elevated locally in tumor tissue or exclusively systemically should be performed in future studies. We only considered evidence from metabolomics studies, which implies that we disregarded potentially relevant data from targeted assays for selected metabolites by design. In this respect, it is crucial that methods currently experiencing significant interest in oncometabolomics research should also be considered in a subsequent investigation. These methods particularly include, matrix-assisted laser desorption ionization (MALDI) – mass spectrometry imaging (MSI) and the field of spatial metabolomics.
Also, we did not study the relationship between the identified metabolites and oncological outcome parameters such as the response to chemotherapy within each study and the relationship with the TNM – or the UICC classification. However, the necessity of an investigation of the relationship between the metabolome and oncological outcome parameters has been highlighted by the results. Finally, misclassification of the reports during study selection and publication bias are essential sources of bias for evidence summaries, which we mitigated through an independent review of the included studies by three authors and detailed analyses of publication bias.
Conclusion and perspectives
The present systematic review and meta-analysis provides an updated overview of the associations between many metabolites and UGC. We performed a meta-analysis for 169 tissue and plasma metabolites associated with the risk of UGC, detecting 155 significant risk associations. The UGC–associated compounds reflect dysregulation of various processes, such as proteolysis, gluconeogenesis, mitochondrial function, and fatty acid oxidation. Many discrepancies were found between the studies, for example, in metabolite behaviour. A small number of studies in each group correctly evaluated the results. The necessity of an investigation of the relationship between the metabolome and oncological outcome parameters has been highlighted by the results of this systematic review and meta-analysis.
Although the patients included in these studies are from across the globe, a targeted multicentric study is necessary to develop a precise oncological and patient-tailored management of UGC. Another point that should be considered is the analysis and research of the same cohort with techniques to account for metabolomics compounds. Finally, the reproduction of some of these studies would enable the use of these metabolites as biomarkers and is highly desirable. We encourage the metabolomics communities to fully disclose their ethics approvals and samples’ storage conditions, report compound names with at least one identifier and include p-values and fold changes for the relevant compounds. With additional investigations published by the scientific community, some of the relevant metabolites found might be reaffirmed as applicable, and others may become irrelevant for UGC pathophysiology. According to the results of our meta-analysis especially BCAA and TMAO as well as certain phosphatidylcholines should be implicated into the diagnostic procedure of patients with UGC. At this point an investigation of the relevance of phosphatidylcholines in certain stages of the oncological treatment should be performed at pace.
Key messages
What is already known on this topic
The prognosis of patients with upper gastrointestinal cancers, i.e. esophageal cancer, cancer of the gastroesophageal junction, and gastric cancer (UGC), is poor in advanced stages. The concept of metabolic plasticity in tumours and their tumour microenvironment (TME) has recently emerged as we started to realize that tumours alter their metabolism to meet the high demands of energy and biomass to fuel their rapid growth and metastasis. In this study, we aimed to characterize differences in concentrations of plasma and tissue metabolites across patients with UGC and healthy controls. Using a statistical approach for vague clustering, we classify groups of metabolites into biochemical and functional categories.
What this study adds
This research summed up the metabolites previously identified to be either increased or decreased in patients with UGC in a systematic review and meta-analysis to create a metanarrative of the current association between metabolites and UGC. In conclusion, summarizing the metabolic profile of patients with upper GI tumours using LC-MS/MS and 1H NMR spectroscopy resulted in the identification of an upper GI cancer-specific signatures driven by increased concentrations of BCAA, lysine, FAD, Acetyl-CoA, adenosine, citrulline, sphinganine, linoleic acid, putrescine, and TMAO as well as decreased concentration of asparagine, glutamine, aconitate, short-chain acylcarnitines, ATP, SM (OH) 22:1, linolenic acid, HCA, HDCA, and erythrose-4-phosphate in plasma, tumour tissue and tissue from the TME compared to healthy controls. The necessity of an investigation of the relationship between the metabolome and oncological outcome parameters has been highlighted by the results of this systematic review and meta-analysis.
How this study might affect research, practice or policy
These data demonstrate the promising potential for plasma and tissue metabolome analyses to dissect the molecular mechanisms of metabolic plasticity of tumours and develop a precise oncological and patient-tailored management of UGC as well as a first approach to metabolism-based cancer therapy. However, further analyses with larger patient cohorts are required to validate this observation. According to the results of our meta-analysis especially BCAA and TMAO as well as certain phosphatidylcholines should be implicated into the diagnostic procedure of patients with UGC.
Data availability
All the data are provided in the supplements.
Abbreviations
- EC:
-
Esophageal cancer
- GEJ:
-
Cancer of the gastroesophageal junction
- GC:
-
Gastric cancer
- UGC:
-
Upper gastrointestinal cancers
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- NOS:
-
Newcastle–Ottawa Scale
- QUADOMICS:
-
An adaptation of the QUADAS-2 (Quality Assessment of Diagnostic Accuracy)
- BCAA:
-
Branched-chain Amino Acids
- BCKDH:
-
Branched-chain alpha-Keto Acid Dehydrogenase Complex
- BCAT:
-
Branched-chain Amino Acid Aminotransferase
- NMR:
-
Nuclear magnetic resonance spectroscopy
- MS:
-
Mass spectroscopy
- LC:
-
Liquid Chromatography
- GC:
-
Gas Chromatography
- CE:
-
Capillary Electrophoresis
- LC–MS/MS:
-
Liquid Chromatography-Tandem Mass Spectroscopy
- HMDB:
-
The Human Metabolome Database
- UPLC-MS/MS:
-
Ultra-Performance-Liquid Chromatography-Tandem Mass Spectroscopy
- HPLC-GC/MS–MS:
-
High-Performance-Liquid Chromatography-Tandem Mass Spectroscopy
- GI:
-
Gastrointestinal
- 1H NMR:
-
Proton Nuclear Magnetic Resonance or Hydrogen-1 NMR
- UPLC-TQ-MS:
-
Ultra-Performance Liquid Chromatography-Triple Quadruple Mass Spectrometry
- UHPLC-MS:
-
Ultra-Performance Liquid Chromatography- Mass Spectrometry
- UHPLC-Q-TOF/MS:
-
Ultra-High Performance Liquid Chromatography-Quadrupole Time-of-Flight Mass Spectrometry
- CE-TOF/MS:
-
Capillary Electrophoresis Time-of-Flight Mass Spectrometry
- GC/TOF–MS:
-
Gas Chromatography–Time-of-Flight Mass Spectrometry
- HPLC/ESI/Q-TOF/MS:
-
High-Performance Liquid Chromatography coupled to Electrospray Ionization Quadrupole Time-of-Flight Mass Spectrometry
- UPLC–TOF/MS:
-
Ultra-Performance Liquid Chromatography- Time-of-Flight Mass Spectrometry
- MRB–CE–MS:
-
Moving Reaction Boundary Capillary Electrophoresis-Mass Spectrometry
- MALDI MS:
-
Matrix-Assisted Laser Desorption/Ionization- Mass Spectrometry
- MALDI MSI:
-
Matrix-Assisted Laser Desorption/Ionization- Mass Spectrometry Imaging
- SIFT-MS:
-
Selected Ion Flow Tube Mass Spectrometry
- SPME-GC/MS:
-
Solid-Phase Microextraction-Gas Chromatography-Mass Spectrometry
- HR-MAS NMR:
-
High-Resolution Magic Angle Spinning-Nuclear Magnetic Resonance
- InChIKey:
-
International Chemical Identifier
- CTS service:
-
Chemical Translation Service
- FAD:
-
Flavin Adenine Dinucleotide
- SM:
-
Sphingolipids
- HCA:
-
Hyocholic acid
- HDCA:
-
Hyodeoxycholic acid
- TCA:
-
Tricarboxylic acid cycle
- MUFA:
-
Monounsaturated Fatty acid
- PUFA:
-
Polyunsaturated Fatty acid
- MG:
-
Monoacylglycerol
- DG:
-
Diacylglycerol
- TG:
-
Triacylglycerol
- PLA2:
-
Phospholipase A2
- Me:
-
Means in experimental group
- Se:
-
Standard deviation in experimental group
- Ne:
-
Headcount in experimental group
- Mc:
-
Means in control group
- Sc:
-
Standard deviation in control group
- Nc:
-
Headcount in control group
References
Aa J et al (2012) Metabolic features of the tumor microenvironment of gastric cancer and the link to the systemic macroenvironment. Metabolomics 8:164–173
Balonov I et al (2023) Changes in plasma metabolomic profile following bariatric surgery, lifestyle intervention or diet restriction-insights from human and rat studies. Int J Mol Sci 24(3):2354
Bartman CR (2023) Thrifty energy metabolism in solid tumours. Nature. https://doi.org/10.1042/bj0230536
Bartman CR et al (2023) Slow TCA flux and ATP production in primary solid tumours but not metastases. Nature 614(7947):349–357
Behuria HG, Dash S, Sahu SK (2022) Phospholipid scramblases: role in cancer progression and anticancer therapeutics. Front Genet 13:875894
Benedetti E et al (2023) A multimodal atlas of tumour metabolism reveals the architecture of gene-metabolite covariation. Nat Metab 5(6):1029–1044
Berrell N et al (2023) Metabolomics at the tumor microenvironment interface: decoding cellular conversations. Med Res Rev. https://doi.org/10.1002/med.22010
Bose S, Zhang C, Le A (2021) Glucose metabolism in cancer: the Warburg effect and beyond. Adv Exp Med Biol 1311:3–15
Bray F et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Buszewski B et al (2008) Identification of volatile organic compounds secreted from cancer tissues and bacterial cultures. J Chromatogr B Analyt Technol Biomed Life Sci 868(1–2):88–94
Cai Z et al (2010) A combined proteomics and metabolomics profiling of gastric cardia cancer reveals characteristic dysregulations in glucose metabolism. Mol Cell Proteom 9(12):2617–2628
Calabrese C et al (2008) Biochemical alterations from normal mucosa to gastric cancer by ex vivo magnetic resonance spectroscopy. Cancer Epidemiol Biomarkers Prev 17(6):1386–1395
Chan AW et al (2014) Potential role of metabolomics in diagnosis and surveillance of gastric cancer. World J Gastroenterol 20(36):12874–12882
Chan AW et al (2016) (1)H-NMR urinary metabolomic profiling for diagnosis of gastric cancer. Br J Cancer 114(1):59–62
Chen JL, Fan J, Lu XJ (2014) CE-MS based on moving reaction boundary method for urinary metabolomic analysis of gastric cancer patients. Electrophoresis 35(7):1032–1039
Cheng M, Bhujwalla ZM, Glunde K (2016) Targeting phospholipid metabolism in cancer. Front Oncol 6:266
Cheng J et al (2017) Towards tyrosine metabolism in esophageal squamous cell carcinoma. Comb Chem High Throughput Screen 20(2):133–139
Choi JM et al (2016) Development of simultaneous analysis of tryptophan metabolites in serum and gastric juice - an investigation towards establishing a biomarker test for gastric cancer diagnosis. Biomed Chromatogr 30(12):1963–1974
Corona G et al (2018) Use of metabolomics as a complementary omic approach to implement risk criteria for first-degree relatives of gastric cancer patients. Int J Mol Sci 19(3):750
Crabtree HG (1929) Observations on the carbohydrate metabolism of tumours. Biochem J 23(3):536–545
Cui Y et al (2023) The crosstalk among the physical tumor microenvironment and the effects of glucose deprivation on tumors in the past decade. Front Cell Dev Biol 11:1275543
Davis VW et al (2012) Urinary metabolomic signature of esophageal cancer and Barrett’s esophagus. World J Surg Oncol 10:271
De Marchi E et al (2019) The P2X7 receptor modulates immune cells infiltration, ectonucleotidases expression and extracellular ATP levels in the tumor microenvironment. Oncogene 38(19):3636–3650
Deng K et al (2011) Three aromatic amino acids in gastric juice as potential biomarkers for gastric malignancies. Anal Chim Acta 694(1–2):100–107
Di Virgilio F et al (2018) Extracellular ATP and P2 purinergic signalling in the tumour microenvironment. Nat Rev Cancer 18(10):601–618
Djukovic D et al (2010) Targeted serum metabolite profiling of nucleosides in esophageal adenocarcinoma. Rapid Commun Mass Spectrom 24(20):3057–3062
Doshi MB et al (2023) Disruption of sugar nucleotide clearance is a therapeutic vulnerability of cancer cells. Nature 623(7987):625–632
Egger M, Smith GD, Phillips AN (1997) Meta-analysis: principles and procedures. BMJ 315(7121):1533–1537
Emoto S et al (2012) Clinical significance of CA125 and CA72-4 in gastric cancer with peritoneal dissemination. Gastric Cancer 15(2):154–161
Faubert B et al (2014) Loss of the tumor suppressor LKB1 promotes metabolic reprogramming of cancer cells via HIF-1alpha. Proc Natl Acad Sci U S A 111(7):2554–2559
Fernandez-Reina A, Urdiales JL, Sanchez-Jimenez F (2018) What we know and what we need to know about aromatic and cationic biogenic amines in the gastrointestinal tract. Foods 7(9):145
Finley LWS (2023) What is cancer metabolism? Cell 186(8):1670–1688
Fu J et al (2021) Research progress of bile acids in cancer. Front Oncol 11:778258
Galon J, Bruni D (2019) Approaches to treat immune hot, altered and cold tumours with combination immunotherapies. Nat Rev Drug Discov 18(3):197–218
Gurdasani D et al (2019) Genomics of disease risk in globally diverse populations. Nat Rev Genet 20(9):520–535
Gustafsson J et al (2024) Metabolic collaboration between cells in the tumor microenvironment has a negligible effect on tumor growth. Innovation (camb) 5(2):100583
Han HS, Lee KW (2024) Liquid biopsy: an emerging diagnostic, prognostic, and predictive tool in gastric cancer. J Gastric Cancer 24(1):4–28
Hasim A et al (2012) Revealing the metabonomic variation of EC using 1H-NMR spectroscopy and its association with the clinicopathological characteristics. Mol Biol Rep 39:8955–8964
Heiliger C et al (2022) Gastroesophageal junction: implementations of reflux and cancer. MMW Fortschr Med 164(18):46–48
Heslin MJ et al (1997) A prospective, randomized trial of early enteral feeding after resection of upper gastrointestinal malignancy. Ann Surg 226(4):567–577
Higgins J et al (2002) Statistical heterogeneity in systematic reviews of clinical trials: a critical appraisal of guidelines and practice. J Health Serv Res Policy 7(1):51–61
Hirayama A et al (2009) Quantitative metabolome profiling of colon and stomach cancer microenvironment by capillary electrophoresis time-of-flight mass spectrometry. Cancer Res 69(11):4918–4925
Huang S et al (2021) Identification and validation of plasma metabolomic signatures in precancerous gastric lesions that progress to cancer. JAMA Netw Open 4(6):e2114186
Huerta-Yepez S, Tirado-Rodriguez AB, Hankinson O (2016) Role of diets rich in omega-3 and omega-6 in the development of cancer. Bol Med Hosp Infant Mex 73(6):446–456
Hur H et al (2014) Quantitative measurement of organic acids in tissues from gastric cancer patients indicates increased glucose metabolism in gastric cancer. PLoS ONE 9(6):e98581
Huybrechts I et al (2023) Associations between fatty acid intakes and plasma phospholipid fatty acid concentrations in the European prospective investigation into cancer and nutrition. Nutrients 15(17):3695
Ikeda A et al (2012) Serum metabolomics as a novel diagnostic approach for gastrointestinal cancer. Biomed Chromatogr 26(5):548–558
Jang C, Chen L, Rabinowitz JD (2018) Metabolomics and isotope tracing. Cell 173(4):822–837
Janne J et al (2004) Genetic approaches to the cellular functions of polyamines in mammals. Eur J Biochem 271(5):877–894
Janneh AH, Ogretmen B (2022) Targeting sphingolipid metabolism as a therapeutic strategy in cancer treatment. Cancers (basel) 14(9):2183
Jaras J, Navaruckiene A, Ostrauskaite J (2023) Thermoresponsive shape-memory biobased photopolymers of tetrahydrofurfuryl acrylate and tridecyl methacrylate. Materials (basel) 16(6):2156
Jiang Z et al (2017) Quantitative proteomic analysis reveals that proteins required for fatty acid metabolism may serve as diagnostic markers for gastric cancer. Clin Chim Acta 464:148–154
Jin G et al (2020) Genetic risk, incident gastric cancer, and healthy lifestyle: a meta-analysis of genome-wide association studies and prospective cohort study. Lancet Oncol 21(10):1378–1386
Jing F et al (2018) Discriminating gastric cancer and gastric ulcer using human plasma amino acid metabolic profile. IUBMB Life 70(6):553–562
Jung J et al (2014) Noninvasive diagnosis and evaluation of curative surgery for gastric cancer by using NMR-based metabolomic profiling. Ann Surg Oncol 21(Suppl 4):S736–S742
Kaji S et al (2020) Metabolomic profiling of gastric cancer tissues identified potential biomarkers for predicting peritoneal recurrence. Gastric Cancer 23(5):874–883
Khodabakhshi A et al (2023) Association between levels of trimethylamine N-oxide and cancer: a systematic review and meta-analysis. Nutr Cancer 75(2):402–414
Kim DH, Song NY, Yim H (2023) Targeting dysregulated lipid metabolism in the tumor microenvironment. Arch Pharm Res. https://doi.org/10.1007/s12272-023-01473-y
Kuligowski J et al (2016) Metabolomic analysis of gastric cancer progression within the Correa’s cascade using ultraperformance liquid chromatography-mass spectrometry. J Proteome Res 15(8):2729–2738
Kumar S et al (2012) Selected ion flow tube-MS analysis of headspace vapor from gastric content for the diagnosis of gastro-esophageal cancer. Anal Chem 84(21):9550–9557
Kwon SY et al (2014) Lipid MALDI MS profiles of gastric cancer. Open Proteom J 7(1):1–4
Kwon HN et al (2020) Screening for early gastric cancer using a noninvasive urine metabolomics approach. Cancers (basel) 12(10):2904
Lario S et al (2017) Plasma sample based analysis of gastric cancer progression using targeted metabolomics. Sci Rep 7(1):17774
Lee GB, Lee JC, Moon MH (2019a) Plasma lipid profile comparison of five different cancers by nanoflow ultrahigh performance liquid chromatography-tandem mass spectrometry. Anal Chim Acta 1063:117–126
Lee JS et al (2019b) Gastric cancer depends on aldehyde dehydrogenase 3A1 for fatty acid oxidation. Sci Rep 9(1):16313
Lee JY et al (2020) Polyunsaturated fatty acid biosynthesis pathway determines ferroptosis sensitivity in gastric cancer. Proc Natl Acad Sci U S A 117(51):32433–32442
Lewis SM et al (2021) Spatial omics and multiplexed imaging to explore cancer biology. Nat Methods 18(9):997–1012
Li D et al (2022) Targeted metabolomic profiles of serum amino acids and acylcarnitines related to gastric cancer. PeerJ 10:e14115
Li B et al (2023) Plasma metabolome identifies potential biomarkers of gastric precancerous lesions and gastric cancer risk. Metabolomics 19(8):73
Liang Q, Wang C, Li B (2015) Metabolomic analysis using liquid chromatography/mass spectrometry for gastric cancer. Appl Biochem Biotechnol 176(8):2170–2184
Lien EC et al (2021) Low glycaemic diets alter lipid metabolism to influence tumour growth. Nature 599(7884):302–307
Ligor T et al (2007) Preliminary study of volatile organic compounds from breath and stomach tissue by means of solid phase microextraction and gas chromatography-mass spectrometry. J Breath Res 1(1):016001
Lin L, Chu H (2018) Quantifying publication bias in meta-analysis. Biometrics 74(3):785–794
Liu R et al (2013) Identification of plasma metabolomic profiling for diagnosis of esophageal squamous-cell carcinoma using an UPLC/TOF/MS platform. Int J Mol Sci 14(5):8899–8911
Liu J et al (2018) Free amino acid profiling of gastric juice as a method for discovering potential biomarkers of early gastric cancer. Int J Clin Exp Pathol 11(5):2323–2336
Llambrich M et al (2022) Amanida: an R package for meta-analysis of metabolomics non-integral data. Bioinformatics 38(2):583–585
Lo CK, Mertz D, Loeb M (2014a) Newcastle-Ottawa scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol 14:45
Lo WY et al (2014b) Urinary cytidine as an adjunct biomarker to improve the diagnostic ratio for gastric cancer in Taiwanese patients. Clin Chim Acta 428:57–62
Long NP et al (2020) Toward a standardized strategy of clinical metabolomics for the advancement of precision medicine. Metabolites 10(2):51
Lopez-Bascon MA et al (2016) Influence of the collection tube on metabolomic changes in serum and plasma. Talanta 150:681–689
Lu X et al (2019) Metabolic profiling analysis upon acylcarnitines in tissues of hepatocellular carcinoma revealed the inhibited carnitine shuttle system caused by the downregulated carnitine palmitoyltransferase 2. Mol Carcinog 58(5):749–759
Lumbreras B et al (2008) QUADOMICS: an adaptation of the quality assessment of diagnostic accuracy assessment (QUADAS) for the evaluation of the methodological quality of studies on the diagnostic accuracy of ’-omics’-based technologies. Clin Biochem 41(16–17):1316–1325
Luo X et al (2017) Emerging roles of lipid metabolism in cancer metastasis. Mol Cancer 16(1):76
Lyssiotis CA, Cantley LC (2014) Acetate fuels the cancer engine. Cell 159(7):1492–1494
Ma W et al (2018) Activation of choline kinase drives aberrant choline metabolism in esophageal squamous cell carcinomas. J Pharm Biomed Anal 155:148–156
Matsumoto T et al (2023) Targeted metabolomic profiling of plasma samples in gastric cancer by liquid chromatography-mass spectrometry. Digestion 104(2):97–108
McNamara KM, Gobert AP, Wilson KT (2021) The role of polyamines in gastric cancer. Oncogene 40(26):4399–4412
Mikami H et al (2019) A multicentre clinical validation of aminoindex cancer screening (AICS). Sci Rep 9(1):13831
Mir SA et al (2015) LC-MS-based serum metabolomic analysis reveals dysregulation of phosphatidylcholines in esophageal squamous cell carcinoma. J Proteom 127(Pt A):96–102
Mun CW et al (2004) Ex vivo proton MR spectroscopy (1H-MRS) for evaluation of human gastric carcinoma. Magn Reson Imaging 22(6):861–870
Nagendrababu V et al (2020) Glossary for systematic reviews and meta-analyses. Int Endod J 53(2):232–249
Neinast M, Murashige D, Arany Z (2019) Branched chain amino acids. Annu Rev Physiol 81:139–164
Nguyen C et al (2014) Trapping the dynamic acyl carrier protein in fatty acid biosynthesis. Nature 505(7483):427–431
Nomura DK et al (2010) Monoacylglycerol lipase regulates a fatty acid network that promotes cancer pathogenesis. Cell 140(1):49–61
Oellgaard J et al (2017) Trimethylamine N-oxide (TMAO) as a new potential therapeutic target for insulin resistance and cancer. Curr Pharm Des 23(25):3699–3712
Ogretmen B (2018) Sphingolipid metabolism in cancer signalling and therapy. Nat Rev Cancer 18(1):33–50
Ouyang T et al (2023) (1)H NMR-based metabolomics of paired tissue, serum and urine samples reveals an optimized panel of biofluids metabolic biomarkers for esophageal cancer. Front Oncol 13:1082841
Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Pan G et al (2020) Discovering biomarkers in peritoneal metastasis of gastric cancer by metabolomics. Onco Targets Ther 13:7199–7211
Pan C et al (2022) Metabolomics study identified bile acids as potential biomarkers for gastric cancer: a case control study. Front Endocrinol (lausanne) 13:1039786
Patti GJ, Tautenhahn R, Siuzdak G (2012) Meta-analysis of untargeted metabolomic data from multiple profiling experiments. Nat Protoc 7(3):508–516
Perera SK et al (2021) Global demand for cancer surgery and an estimate of the optimal surgical and anaesthesia workforce between 2018 and 2040: a population-based modelling study. Lancet Oncol 22(2):182–189
Petan T, Jarc E, Jusovic M (2018) Lipid droplets in cancer: guardians of fat in a stressful world. Molecules 23(8):1941
Reed MAC et al (2017) Metabolomic evidence for a field effect in histologically normal and metaplastic tissues in patients with esophageal adenocarcinoma. Neoplasia 19(3):165–174
Rezen T et al (2022) The role of bile acids in carcinogenesis. Cell Mol Life Sci 79(5):243
Schiavo JH (2019) PROSPERO: An international register of systematic review protocols. Med Ref Serv Q 38(2):171–180
Shamseer L et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350:g7647
Shao D et al (2018) Glucose promotes cell growth by suppressing branched-chain amino acid degradation. Nat Commun 9(1):2935
Shaw JH, Wolfe RR (1987) Fatty acid and glycerol kinetics in septic patients and in patients with gastrointestinal cancer. The response to glucose infusion and parenteral feeding. Ann Surg 205(4):368–376
Shu X et al (2021) A prospective investigation of circulating metabolome identifies potential biomarkers for gastric cancer risk. Cancer Epidemiol Biomarkers Prev 30(9):1634–1642
Siegel RL et al (2022) Cancer statistics, 2022. CA Cancer J Clin 72(1):7–33
Sivanand S, Vander Heiden MG (2020) Emerging roles for branched-chain amino acid metabolism in cancer. Cancer Cell 37(2):147–156
Slankamenac K et al (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258(1):1–7
Smyth EC et al (2020) Gastric cancer. Lancet 396(10251):635–648
Song H et al (2012) Serum metabolic profiling of human gastric cancer based on gas chromatography/mass spectrometry. Braz J Med Biol Res 45(1):78–85
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Stier C et al (2020) Endoscopic management of clinically severe obesity: primary and secondary therapeutic procedures. Curr Obes Rep 9(3):339–347
Stine ZE et al (2022) Targeting cancer metabolism in the era of precision oncology. Nat Rev Drug Discov 21(2):141–162
Stonans I et al (2023) The association of circulating L-carnitine, gamma-butyrobetaine and trimethylamine N-oxide levels with gastric cancer. Diagnostics (basel) 13(7):1341
Sumner LW et al (2007) Proposed minimum reporting standards for chemical analysis chemical analysis working group (CAWG) metabolomics standards initiative (MSI). Metabolomics 3(3):211–221
Sun C et al (2023) Spatially resolved multi-omics highlights cell-specific metabolic remodeling and interactions in gastric cancer. Nat Commun 14(1):2692
Tallima H, Azzazy HME, El Ridi R (2021) Cell surface sphingomyelin: key role in cancer initiation, progression, and immune evasion. Lipids Health Dis 20(1):150
Tan Y et al (2018) Adipocytes fuel gastric cancer omental metastasis via PITPNC1-mediated fatty acid metabolic reprogramming. Theranostics 8(19):5452–5468
Taniguchi M, Okazaki T (2021) Role of ceramide/sphingomyelin (SM) balance regulated through “SM cycle” in cancer. Cell Signal 87:110119
Thompson CB et al (2023) A century of the Warburg effect. Nat Metab 5(11):1840–1843
Tokunaga M et al (2018) Metabolome analysis of esophageal cancer tissues using capillary electrophoresis-time-of-flight mass spectrometry. Int J Oncol 52(6):1947–1958
Tomita M, Kami K (2012) Cancer. Systems biology, metabolomics, and cancer metabolism. Science 336(6084):990–991
Tsai CK et al (2018) Metabolomic alterations and chromosomal instability status in gastric cancer. World J Gastroenterol 24(33):3760–3769
Tsuboi K (2019) 2-Hydroxylated fatty acids as candidates of novel drugs to promote chemosensitivity of gastric cancer. EBioMedicine 41:19–20
Tugnoli V et al (2006) Ex vivo HR-MAS magnetic resonance spectroscopy of human gastric adenocarcinomas: a comparison with healthy gastric mucosa. Oncol Rep 16(3):543–553
van Geldermalsen M et al (2016) ASCT2/SLC1A5 controls glutamine uptake and tumour growth in triple-negative basal-like breast cancer. Oncogene 35(24):3201–3208
Wang L et al (2013) 1H-NMR based metabonomic profiling of human esophageal cancer tissue. Mol Cancer 12:25
Wang H et al (2016) Tissue metabolic profiling of human gastric cancer assessed by (1)H NMR. BMC Cancer 16:371
Wang D et al (2017) Serum metabolomic profiling of human gastric cancer and its relationship with the prognosis. Oncotarget 8(66):110000–110015
Wang D et al (2020) Association of serum levels of deoxyribose 1-phosphate and S-lactoylglutathione with neoadjuvant chemotherapy sensitivity in patients with gastric cancer: a metabolomics study. Oncol Lett 19(3):2231–2242
Wang Y et al (2021) Tissue-based metabolomics reveals metabolic signatures and major metabolic pathways of gastric cancer with help of transcriptomic data from TCGA. Biosci Rep 41(10):BSR20211476
Warburg O (1956a) On the origin of cancer cells. Science 123(3191):309–314
Warburg O (1956b) On respiratory impairment in cancer cells. Science 124(3215):269–270
Warburg O, Wind F, Negelein E (1927) The metabolism of tumors in the body. J Gen Physiol 8(6):519–530
Whiting P et al (2003) The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 3:25
Whiting PF et al (2006) Evaluation of QUADAS, a tool for the quality assessment of diagnostic accuracy studies. BMC Med Res Methodol 6:9
Wishart DS et al (2022) HMDB 5.0: the human metabolome database for 2022. Nucleic Acids Res 50(D1):D622–D631
Wu H et al (2010) Metabolomic investigation of gastric cancer tissue using gas chromatography/mass spectrometry. Anal Bioanal Chem 396(4):1385–1395
Wu H et al (2019) Lipid droplet-dependent fatty acid metabolism controls the immune suppressive phenotype of tumor-associated macrophages. EMBO Mol Med 11(11):e10698
Wu X et al (2022) Metabolite biomarker discovery for human gastric cancer using dried blood spot mass spectrometry metabolomic approach. Sci Rep 12(1):14632
Xie L et al (2023) Determination of polyamines in urine via electrospun nanofibers-based solid-phase extraction coupled with GC-MS and application to gastric cancer patients. J Sep Sci 46(3):e2200629
Xu J et al (2016) Global metabolomics reveals potential urinary biomarkers of esophageal squamous cell carcinoma for diagnosis and staging. Sci Rep 6:35010
Yakoub D et al (2010) Metabolic profiling detects field effects in nondysplastic tissue from esophageal cancer patients. Cancer Res 70(22):9129–9136
Yang Y et al (2013) Study of metabonomic profiles of human esophageal carcinoma by use of high-resolution magic-angle spinning 1H NMR spectroscopy and multivariate data analysis. Anal Bioanal Chem 405(10):3381–3389
Yang XL et al (2022a) Untargeted serum metabolomics reveals potential biomarkers and metabolic pathways associated with esophageal cancer. Front Oncol 12:938234
Yang T et al (2022b) Untargeted metabolomics analysis of esophageal squamous cell cancer progression. J Transl Med 20(1):127
Ye W et al (2021) (1) H NMR-based metabolomics of paired esophageal tumor tissues and serum samples identifies specific serum biomarkers for esophageal cancer. NMR Biomed 34(6):e4505
Yu L et al (2011) Metabolomic phenotype of gastric cancer and precancerous stages based on gas chromatography time-of-flight mass spectrometry. J Gastroenterol Hepatol 26(8):1290–1297
Yu L et al (2021) Serum metabolic profiling analysis of chronic gastritis and gastric cancer by untargeted metabolomics. Front Oncol 11:636917
Yu J et al (2023) Metabolomics reveals novel serum metabolic signatures in gastric cancer by a mass spectrometry platform. J Proteome Res 22(3):706–717
Yuan Q et al (2022) Integration of transcriptomics, proteomics, and metabolomics data to reveal HER2-associated metabolic heterogeneity in gastric cancer with response to immunotherapy and neoadjuvant chemotherapy. Front Immunol 13:951137
Yuneva M (2008) Finding an "Achilles’ heel" of cancer: the role of glucose and glutamine metabolism in the survival of transformed cells. Cell Cycle 7(14):2083–2089
Zhang J et al (2011) Metabolomics study of esophageal adenocarcinoma. J Thorac Cardiovasc Surg 141(2):469-75-475e1-4
Zhang J et al (2012) Esophageal cancer metabolite biomarkers detected by LC-MS and NMR methods. PLoS ONE 7(1):e30181
Zhang X et al (2013) Metabolic signatures of esophageal cancer: NMR-based metabolomics and UHPLC-based focused metabolomics of blood serum. Biochim Biophys Acta 1832(8):1207–1216
Zhang H et al (2017) Metabolomic profiling reveals potential biomarkers in esophageal cancer progression using liquid chromatography-mass spectrometry platform. Biochem Biophys Res Commun 491(1):119–125
Zhang LY et al (2021) Bile reflux is an independent risk factor for precancerous gastric lesions and gastric cancer: an observational cross-sectional study. J Dig Dis 22(5):282–290
Zhang Z et al (2023) Mitochondrial energy metabolism correlates with an immunosuppressive tumor microenvironment and poor prognosis in esophageal squamous cell carcinoma. Comput Struct Biotechnol J 21:4118–4133
Zhao X et al (2023) Metabolic codependencies in the tumor microenvironment and gastric cancer: difficulties and opportunities. Biomed Pharmacother 162:114601
Zhu X et al (2017) Metabolic perturbation and potential markers in patients with esophageal cancer. Gastroenterol Res Pract 2017:5469597
Zhu H et al (2023) Engineered Lipidic nanomaterials inspired by sphingomyelin metabolism for cancer therapy. Molecules 28(14):5366
Acknowledgements
We acknowledge the contribution in data documentation and the valuable scientific input from Eva Trivaks. All authors contributed to the article and approved the submitted version.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research was supported by the German Research Foundation (DFG), grant number DFG; DI 2915/2-1 to I.B.
Author information
Authors and Affiliations
Contributions
IB: Conceived the study, took part in study design and coordination, performed statistical tests and drafted the manuscript. MM: Participated in and validated statistical analysis. STJ: Helped in its design and coordination and statistical analysis. BK: Helped in its design and coordination, and drafted the manuscript. KH: Helped in its design and coordination and statistical analysis. JN: Conceived the study, provided funding, helped design and coordination, and drafted the manuscript. JW: Conceived the study, provided funding, and helped in its design. MKA: Conceived the study, provided funding, helped in its design and coordination, and drafted the manuscript. CH: Took part in study design and coordination, performed statistical tests and drafted the manuscript.SJ: Took part in study design and coordination, performed statistical tests and drafted the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no related conflicts of interest to declare. No external is to be declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Balonov, I., Mattis, M., Jarmusch, S. et al. Metabolomic profiling of upper GI malignancies in blood and tissue: a systematic review and meta-analysis. J Cancer Res Clin Oncol 150, 331 (2024). https://doi.org/10.1007/s00432-024-05857-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00432-024-05857-5