Abstract
Background
An increasing number of cohort studies have indicated a correlation between lung diseases and esophageal cancer, but the exact causal relationship has not been definitively established. Therefore, the objective of this study is to assess the causal relationship between lung diseases and esophageal cancer.
Methods
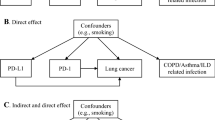
Single-nucleotide polymorphisms (SNPs) related to lung diseases such as asthma, chronic obstructive pulmonary disease (COPD), lung cancer, and idiopathic pulmonary fibrosis (IPF), along with outcomes data on esophageal cancer, were extracted from public genome-wide association studies (GWAS). A two-sample Mendelian randomization (MR) analysis was then performed using publicly available GWAS data to investigate the potential causal relationship. The effect estimates were primarily calculated using the fixed-effects inverse-variance-weighted method.
Results
Totally, 81 SNPs related to asthma among 218,792 participants in GWAS. Based on the primary causal effects model using MR analyses with the inverse variance weighted (IVW) method, asthma was demonstrated a significantly related to the risk of esophageal cancer (OR 1.0006; 95% CI 1.0003–1.0010, p = 0.001), while COPD (OR 1.0306; 95% CI 0.9504–1.1176, p = 0.466), lung cancer (OR 1.0003, 95% CI 0.9998–1.0008, p = 0.305), as well as IPF (OR 0.9999, 95% CI 0.9998–1.0000, p = 0.147), showed no significant correlation with esophageal cancer.
Conclusions
The two-sample MR analysis conducted in this study revealed a positive causal relationship between asthma and esophageal cancer. In contrast, esophageal cancer demonstrated no significant correlation with COPD, lung cancer, or IPF. Further large-sample prospective studies are needed to validate these findings and to provide appropriate recommendations regarding esophageal cancer screening among patients with asthma.




Similar content being viewed by others
Data availability
The datasets used in this study are available from the corresponding author upon reasonable request.
References
Bowden J, Davey Smith G, Burgess S (2015) Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol 44:512–525
Burgess S, Bowden J, Fall T, Ingelsson E, Thompson SG (2017) Sensitivity analyses for robust causal inference from mendelian randomization analyses with multiple genetic variants. Epidemiology 28:30–42
Chiang CL, Hu YW, Wu CH, Chen YT, Liu CJ, Luo YH, Chen YM, Chen TJ, Su KC, Chou KT (2016) Spectrum of cancer risk among Taiwanese with chronic obstructive pulmonary disease. Int J Clin Oncol 21:1014–1020
Choi YJ, Han K, Jin EH, Lim JH, Shin CM, Lee DH (2023) Allergic diseases and risk of malignancy of gastrointestinal cancers. Cancers 15:3219
Davey Smith G, Ebrahim S (2005) What can mendelian randomisation tell us about modifiable behavioural and environmental exposures? BMJ 330:1076–1079
Emdin CA, Khera AV, Kathiresan S (2017) Mendelian randomization. JAMA 318:1925–1926
Feng R, Lu M, Xu J, Zhang F, Yang M, Luo P, Xu K, Xu P (2022) Pulmonary embolism and 529 human blood metabolites: genetic correlation and two-sample Mendelian randomization study. BMC Genomic Data 23:69
Hong JT, Son DJ, Lee CK, Yoon DY, Lee DH, Park MH (2017) Interleukin 32, inflammation and cancer. Pharmacol Ther 174:127–137
Lemanske RF Jr, Busse WW (2010) Asthma: clinical expression and molecular mechanisms. J Allergy Clin Immunol 125:S95-102
Machiela MJ, Chanock SJ (2015) LDlink: a web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics 31:3555–3557
Maier RM, Visscher PM, Robinson MR, Wray NR (2018) Embracing polygenicity: a review of methods and tools for psychiatric genetics research. Psychol Med 48:1055–1067
Menon S, Nightingale P, Trudgill N (2019) Chronic obstructive pulmonary disease and the risk of esophagitis, Barrett’s esophagus, and esophageal adenocarcinoma: a primary care case-control study. J Clin Gastroenterol 53:e451–e455
Nandi B, Talluri S, Kumar S, Yenumula C, Gold JS, Prabhala R, Munshi NC, Shammas MA (2019) The roles of homologous recombination and the immune system in the genomic evolution of cancer. J Transl Sci. https://doi.org/10.15761/JTS.1000282
Song JH, Han YM, Kim WH, Park JM, Jeong M, Go EJ, Hong SP, Hahm KB (2016) Oxidative stress from reflux esophagitis to esophageal cancer: the alleviation with antioxidants. Free Radical Res 50:1071–1079
Wang D, Cabalag CS, Clemons NJ, DuBois RN (2021) Cyclooxygenases and prostaglandins in tumor immunology and microenvironment of gastrointestinal cancer. Gastroenterology 161:1813–1829
Yawn BP (2008) Factors accounting for asthma variability: achieving optimal symptom control for individual patients. Prim Care Respir J 17:138–147
Ye W, Chow WH, Lagergren J, Boffetta P, Boman G, Adami HO, Nyrén O (2001) Risk of adenocarcinomas of the oesophagus and gastric cardia in patients hospitalized for asthma. Br J Cancer 85:1317–1321
Funding
This work was supported by the National Natural Science Foundation of China (81970481, 82000514), Sichuan Science and Technology Program (2022YFS0048, 2021YFS0222), 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (2020HXFH047, ZYJC18010 and 20HXJS005, 2018HXFH020), and China Postdoctoral Science Foundation (2020M673241).
Author information
Authors and Affiliations
Contributions
YY: conceptualized the study, revised the manuscript, and supervised the study. JZ, PF, and LZ: conceptualized the study, drafted the manuscript, and made the figures. XL, SL, XX, YG, QS, HZ, YuY, LC, and XZ: collected the literature and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
432_2023_5324_MOESM1_ESM.png
Supplementary file1 Supplemental Figure S1: Leave-one-out sensitivity analysis of the association of (A) asthma, (B) COPD, (C) lung cancer and (D) IPF and esophageal cancer. COPD: chronic obstructive pulmonary disease; IPF: idiopathic pulmonary fibrosis (PNG 4426 KB)
432_2023_5324_MOESM2_ESM.png
Supplementary file2 Supplemental Figure S2: Funnel plot of the association of (A) asthma, (B) COPD, (C) lung cancer and (D) IPF and esophageal cancer. COPD: chronic obstructive pulmonary disease; IPF: idiopathic pulmonary fibrosis (PNG 2418 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, J., Fang, P., Liang, Z. et al. Causal relationship between lung diseases and risk of esophageal cancer: insights from Mendelian randomization. J Cancer Res Clin Oncol 149, 15679–15686 (2023). https://doi.org/10.1007/s00432-023-05324-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-05324-7