Abstract
Background
Four Fanconi anemia (FA) genes (BRCA1, BRCA2, PALB2 and RAD51C) are defined as breast cancer (BC) susceptibility genes. Other FA genes have been inconsistently associated with BC. Thus, the role of other FA genes in BC should be explored in specific populations.
Methods
Mutations in 16 FA genes were screened with a 98-gene panel sequencing assay in a cohort of 1481 Chinese patients with high-risk hereditary BC. The association between mutations and clinicopathological characteristics as well as prognosis was analyzed. The risk of BC in carriers of FA gene mutations was assessed in the Genome Aggregation Database and the Westlake Biobank for Chinese cohort.
Results
A total of 2.57% (38/1481) BC patients were identified who had 12 other FA gene germline mutations. Among them, the most frequently mutated gene was FANCA (8/1481, 0.54%). These 38 patients carried 35 distinct pathogenic/likely pathogenic variants, of which 21 were novel. We found one rare FANCB deleterious variant (c.1327-3dupT) in our cohort. There was a statistically significant difference in lymph node status between FA gene mutation carriers and non-carriers (p = 0.041). We observed a trend that mutation carriers had larger tumor sizes, lower estrogen receptor (ER) and progesterone receptor (PR) positivity rates, and lower 3.5-year invasive disease-free survival (iDFS) and distant recurrence-free survival (DRFS) rates than non-carriers (tumor size > 2 cm: 51.43% vs. 45.63%; ER positivity rates: 51.43% vs. 60.81%; PR positivity rates: 48.57% vs. 55.16%; 3.5-year iDFS rates: 58.8% vs. 66.7%; 3.5-year DRFS rates: 58.8% vs. 68.8%). The frequency of the mutations in FANCD2, FANCM and BRIP1 trended to be higher among BC cases than that in controls (p = 0.055, 0.08 and 0.08, respectively).
Conclusion
This study comprehensively estimated the prevalence, clinicopathological characteristics, prognosis and risk of BC associated with deleterious variants in FA genes in Chinese high-risk hereditary BC patients. It enriches our understanding of the role of FA genes with BC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) is the most common malignancy that affects women worldwide. BC is highly associated with genetic factors (Castéra et al. 2014; Sung et al. 2021; Tung et al. 2016). Germline variants in 13 susceptibility genes have been shown to be related to the tumorigenesis and risk of BC. These genes are BRCA1, BRCA2, TP53, ATM, RAD51C, RAD51D, PALB2, CHEK2, NF1, BARD1, PTEN, STK11 and CDH1 (Dorling et al. 2021; Easton et al. 2015). Among them, BRCA1 and BRCA2 were the first genes reported to be associated with an increased risk of breast and ovarian cancer (Szabo et al. 1995; Wooster et al. 1994). A prospective cohort study showed a cumulative BC risk of 72% for BRCA1 carriers and 69% for BRCA2 carriers by age 80 (Kuchenbaecker et al. 2017). In a meta-analysis, the estimated relative risk of a PALB2 mutation in BC was approximately 5.3 (Easton et al. 2015). The estimated relative risk of RAD51C in BC was 1.99, with an estimated cumulative risk of 21% for the occurrence of BC up to 80 years old (Yang et al. 2020). FANCS/BRCA1, FANCD1/BRCA2, FANCN/PALB2 and FANCO/RAD51C are Fanconi anemia (FA) genes (Fang et al. 2020). Other than these, 18 genes have been described as FA genes: FANCA, FANCB, FANCC, FANCD2, FANCE, FANCF, FANCG/XRCC9, FANCI, FANCJ/BRIP1, FANCL/PHF9, FANCM, FANCP/SLX4, FANCQ/ERCC4, FANCR/RAD51, FANCT/UBE2T, FANCU/XRCC2, FANCV/REV7 (Bluteau et al. 2016) and FANCW/RFWD3 (Knies et al. 2017; Nalepa et al. 2018). The genetic susceptibility of 17 of these genes other than FANCW to BC has been much studied, but the results are conflicting and await further exploration (Gianni et al. 2022).
FA is an uncommon genetic disorder characterized by progressive aplastic anemia, congenital malformations and tumor susceptibility (Mamrak et al. 2017). FA gene products are involved in the FA-BRCA pathway, coordinating nucleolytic incision, translesion DNA synthesis and homologous recombination (HR), and they play a key role in DNA damage, particularly in DNA interstrand cross-link (ICL) repair (Kim et al. 2012; Zhang et al. 2014). In addition, FA proteins protect genomic stability by regulating the cell cycle checkpoint and replication fork remodeling (Badra Fajardo et al. 2022). FA pathway-deficient tumor cells are more sensitive to the DNA ICL inducer cisplatin after inhibition of the FA pathway (Jacquemont et al. 2012). Tumors with germline mutations in FA genes encoding HR proteins are sensitive to DNA damaging agents including cisplatin and Poly (ADP-ribose) polymerase (PARP) inhibitors due to accumulated DNA lesions (Cong et al. 2021; Ray Chaudhuri et al. 2016; Simoneau et al. 2021). This suggests that disease-causing pathogenic germline variants in FA genes may be important therapeutic targets that can get benefit from targeted alternative DNA repair pathways.
The association between FA genes (except BRCA1, BRCA2, PALB2 and RAD51C) that have not been confirmed as BC susceptibility genes has been less studied in the Chinese population. Additionally, whether pathogenic variants in FA genes have prognostic impact on clinical outcomes in patients with BC is unknown. To explore the role of FA genes in BC, we studied the mutation profile of FA genes in 1481 patients with high-risk hereditary BC and investigated whether the presence of FA gene mutations affected the clinicopathological characteristics and outcomes of BC patients. We also explored the risk of BC by comparing the FA variants identified in our cohort with non-cancer patients in the Genome Aggregation Database (GnomAD) East Asian cohort and the Westlake Biobank for Chinese (WBBC) cohort.
Materials and methods
Patients
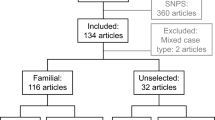
We conducted a prospective cohort study including 1481 cases with hereditary high-risk BC who underwent genetic counseling/testing at the Zhejiang Cancer Hospital from February 2008 to April 2022 to explore the role of FA genes in BC. Patients were enrolled based on the National Comprehensive Cancer Network guidelines for genetic/familial high-risk assessment on breast, ovarian and pancreatic cancer (Daly et al. 2021). High-risk hereditary BC patients fulfilled at least one of the following criteria: (1) diagnosed with BC at age ≤ 40 years; (2) diagnosed with triple-negative breast cancer (TNBC) at ≤ 50 years; (3) diagnosed with bilateral or ipsilateral multi-focal BC; (4) male BC; (5) having a minimum of one first- or second-degree relative who had BC, ovarian cancer, pancreatic cancer or distant metastatic prostate cancer; individuals with ovarian cancer and/or pancreatic cancer. Clinical information including clinicopathological data, outcome variables and familial history of cancer was collected from medical records and/or by telephone follow-up. The study was approved by the Research and Ethics Committee of Zhejiang Cancer Hospital. Written informed consent was obtained from all subjects.
FA gene variants
DNA samples were isolated from peripheral blood samples of BC patients with the QIAamp DNA Blood Mini kit (Qiagen). A panel (Yang et al. 2023) covering whole exons of 98 genes was used to identify variants in FA genes. Details of the DNA sequencing and bioinformatic analysis have been published previously (Zhu et al. 2022). Briefly, all samples were diluted and pooled in a HiSeq X-Ten (Illumina) for multiplexed sequencing.
The variants were interpreted and filtered according to the American College of Medical Genetics and Genomics Standards and Guidelines for the Interpretation of Sequence Variants. The evidence was based on databases and predictive software such as ClinVar (https://www.ncbi.nlm.nih.gov/) and the Human Gene Mutation Database (http://www.hgmd.org/). Only variants classified as pathogenic or likely pathogenic were included.
GnomAD and WBBC analysis
The GnomAD East Asian, non-cancer subpopulation (v.2.1.1, http://www.gnomad-sg.org/) and the WBBC cohort (GRCh37, https://wbbc.westlake.edu.cn/index.html) were used as control populations. Variants predicted to be loss-of-function in FA genes were exported to test the associations between FA genes and BC risk.
Statistical analysis
Variables included age at diagnosis, personal and family history of BC, personal and family history of ovarian cancer, tumor size, lymph node status, pathological type, nuclear grade (I, II and III), vascular invasion, estrogen receptor (ER) and progesterone receptor (PR) status, HER2 receptor status, age of menarche and menopause and BMI. Continuous variables were analyzed with a t test. Comparison of categorical variables was conducted using the Chi-square test or Fisher’s exact test.
Follow-up started at the time blood was drawn. The latest date of follow-up was when patients visited the physician or received telephone call from us at the last time. Distant recurrence-free survival (DRFS) was defined as the time from the date of surgery to distant recurrence or death from any cause. Invasive disease-free survival (iDFS) was measured from the date of surgery to the date of first occurrence of ipsilateral invasive breast tumor recurrence, local/regional invasive BC recurrence, distant recurrence, death attributable to any cause, contralateral invasive BC or a second primary non-breast invasive cancer. The definition of loss to follow-up was event-free patients with a follow-up period of more than 5 years who were out of touch for over 1.5 years or event-free patients with follow-up period of within 5 years who were out of touch for more than 1 year. A total of 21% of patients were lost to follow-up until April 2022.The Kaplan–Meier method was used to assess DRFS and iDFS. Associations between FA genes and BC risk were estimated by logistic regression.
Statistical significance was defined as a two-tailed p value < 0.05. All analyses were performed using SPSS Statistics 25.0 software (IBM, Armonk, NY).
Results
Prevalence of FA gene germline mutations
Genetic testing was performed in 1481 patients with high-risk hereditary BC. A total of 313 patients were identified as carrying at least one of 13 BC susceptibility gene mutations, and 38 patients carried 35 distinct pathogenic/likely pathogenic variants in 12 FA genes (BRCA1/2, PALB2 and RAD51C were not included). Mutations in FANCF, FANCR/RAD51, FANCT/UBE2T and FANCU/XRCC2 were not found in this cohort. Among the 38 FA gene mutation carriers, the most frequently mutated gene was FANCA (8/1481, 0.54%), and other mutations found were in FANCD2 (6/1481, 0.41%), FANCM (5/1481, 0.34%), BRIP1 (5/1481, 0.34%), FANCC (4/1481, 0.27%), FANCI (2/1481, 0.14%), FANCL (2/1481, 0.14%), FANCP/SLX4 (2/1481, 0.14%), FANCQ/ERCC4 (1/1481, 0.07%), FANCE (1/1481, 0.07%), FANCG (1/1481, 0.07%) and FANCB (1/1481, 0.07%). Seven FANCA deleterious variants were detected in eight patients, including 2 (2/8, 25%) frameshift, 2 (2/8, 25%) stop-gain, 2 (2/8, 25%) splicing and 2 (2/8, 25%) missense variants. Four (4/8, 50%) novel FANCA variants were identified: c.3393dupT (p.Ala1132Cysfs*83, n = 1), c.1715 + 1G > C (n = 1), c.3342dupT (p.Glu1115Ter, n = 1) and c.1287delT (p.Ala430ArgfsTer96, n = 1). Furthermore, 17 novel variants in other FA genes was identified: BRIP1 c.3182_3189delACACATCG (p.Asn1061Ilefs*17, n = 1), BRIP1 c.3223delT (p.Ser1075Hisfs*3, n = 1), FANCB c.1327-3dupT (n = 1), FANCC c.844-1G > A (n = 1), FANCC c.887_890dupAGAT (p.Met297Ilefs*78, n = 1), FANCD2 c.1991_1992insA (p.Phe664Leufs*12, n = 1), FANCD2 c.1656 + 2 T > A (n = 1), FANCD2 c.783 + 1G > A (n = 1), FANCD2 c.2155G > T (p.Glu719Ter, n = 1), FANCI c.1954_1955dupTC (p.Thr653Ter, n = 1), FANCI c.2889 + 1G > C (n = 1), FANCL c.857 T > G (p.Leu286Ter, n = 1), FANCL c.555 + 1G > T (n = 1), FANCM c.4515 + 1G > C (n = 2), FANCM c.170_189delTGCTTGTCGCGGCGTACGAG (p.Leu57Cysfs*2, n = 1), FANCP/SLX4 c.817C > T (p.Gln273Ter, n = 1) and FANCP/SLX4 c.4481delG (p.Gly1494Alafs*13, n = 1). Notably, two patients carried two distinct variants: FANCA with BRCA1 and FANCD2 with BRCA2. One patient with three distinct mutations in ATM, BLM and FANCA was observed (see Table 1).
Association between FA gene germline mutations and clinicopathological characteristics
According to the results of genetic testing, 35 patients (excluding the three patients carrying multiple different gene mutations) carrying one germline mutation in an FA gene (except BRCA1/2, PALB2 and RAD51C) were included in the mutation group, and 1,133 patients who did not carry any mutations in BC susceptibility genes were the control group. The differences in clinicopathological characteristics between FA mutation carriers and non-carriers were compared (Table 2). There was a statistically significant difference in lymph node status in FA gene mutations carriers when compared to the control group (p = 0.041). Mutation carriers had a trend toward larger tumor sizes and lower ER/PR positivity rates than non-carriers (tumor sizes > 2 cm: 51.43% vs. 45.63%; ER positivity rates: 51.43% vs. 60.81%; PR positivity rates: 48.57% vs. 55.16%). However, a significant statistical difference in tumor size and ER/PR status and other was not observed between the FA gene mutation carriers and non-carriers.
Comparison of survival among FA gene variant carriers and non-carriers
After a median follow-up of 38 months (range 1–200 months), we compared the survival rate between FA gene mutation carriers and non-carriers (Fig. 1). There was a trend toward a difference in the 3-year iDFS and DRFS rates between carriers and non-carriers (3.5-year iDFS rates: 58.8% vs. 66.7%; 3.5-year DRFS rates: 58.8% vs. 68.8%), but there was no statistically significant difference between the two groups (p = 0.719 and 0.417 for iDFS and DRFS, respectively).
FA gene mutations and BC risk
When comparing the mutation frequencies in FA genes in our cohort with those from the East Asian (non-cancer) GnomAD v.2.1 population, there was no association between the 11 FA genes identified in our cohort and BC risk (Table 3). The East Asian population in the GnomAD database contains Japanese, Korean and other ethnic groups. Therefore, we compared variant frequencies in the WBBC database (Table 3). Mutations in FANCD2, FANCM and BRIP1 were more common in our cohort when compared to controls (without achieving statistical significance; p = 0.055, 0.08 and 0.08, respectively). There were no deleterious variants in FANCB in the East Asian population in GnomAD or in the WBBC. Thus, we could not estimate the difference in FANCB by logistic regression.
Discussion
Approximately 15–20% of BC cases show familial aggregation or a clear pattern of inheritance (Wendt et al. 2019). In these populations, only a small percentage of patients have detectable pathogenic variants in tumor susceptibility genes (Kurian et al. 2014; LaDuca et al. 2014; Tung et al. 2016). We identified heterozygous mutations in 12 FA genes in 38 of 1481 patients with hereditary high-risk BC in this study. Among them, FANCA was the most frequently mutated gene, in agreement with previous findings (Del Valle et al. 2020; Solomon et al. 2015). Pathogenic/likely pathogenic variants in FANCF, FANCR/RAD51, FANCT/UBE2T and FANCU/XRCC2 were not found in our cohort.
To explore the relationship between FA gene mutations and clinicopathological characteristics, we analyzed pathological findings and clinical data from carriers and non-carriers, which showed significantly more lymph node metastasis in carriers (p = 0.041). Larger tumor sizes and lower ER/PR positivity rates were more common among carriers in comparison to non-carriers, although these were not statistically significant. Studies have investigated the association between FA gene expression and BC. Low FANCD2 expression is related to high histologic grade and pathologic stage in BC (Zhang et al. 2010).Hallajian et al. (2017) found that downregulated expression of RAD51 was associated with high lymph node involvement in BC. In addition, Wang et al. (2018) reported that high FANCM expression was related to low Ki-67 status (p = 0.003), and patients with upregulated expression of FANCM had better overall survival in luminal B subtype BC. Santarpia et al. (Santarpia et al. 2013) reported that FANCI was associated with poor prognosis in ER-positive/HER2-negative BC. After a median follow-up of 38 months, although there was no significant difference in iDFS and DRFS between FA gene mutation carriers and non-carriers in our cohort, the 3.5-year iDFS and DRFS rates tended to be lower in carriers than in non-carriers. These results suggest that loss-of-function variants or downregulated expression of FA genes may be associated with an aggressive phenotype and worse prognosis.
In this study, we evaluated susceptibility to BC for carriers of FA gene mutations and found that FANCD2, FANCM and BRIP1 were nearly statistically significant (p = 0.055, 0.08 and 0.08, respectively). FANCD2 knockout causes animals to develop BC (Houghtaling et al. 2003). Mantere et al. (Mantere et al. 2017) identified that FANCD2 c.2715 + 1G > A was 2.6-fold more frequent in Finnish BC patients than in controls (p = 0.131). In our study, the incidence of FANCD2 mutation also was trend to more common than that in WBBC controls. The association with BC for FANCM mutations has been well investigated, especially for TNBC (Peterlongo et al. 2021). In the Finnish population, FANCM c.5101C > T was associated with BC (odds ratio [OR] = 1.86, 95% confidence interval [CI]: 1.26–2.75; p = 0.0018), especially with TNBC (OR = 3.56, 95% CI 1.81–6.98, p = 0.0002) (Kiiski et al. 2014). However, FANCM c.5791C > T was not statistically significantly associated with BC (OR = 1.94, 95% CI 0.87–4.32, p = 0.11), but it was associated with increased risk of TNBC (OR = 5.14, 95% CI 1.65–16.0, p = 0.005) (Kiiski et al. 2017). Figlioli et al. (2019) reported that FANCM c.1972C > T was associated with ER-negative BC and TNBC (OR = 2.44, 95% CI 1.12–5.34, p = 0.034 and OR = 3.79, 95% CI 1.56–9.18, p = 0.009, respectively). In our cohort, FANCM showed a trend with increased BC risk (OR = 3.032, 95% CI 0.877–10.487, p = 0.08). These suggest that some FA genes could be candidates for BC susceptibility genes. BRIP1 was first reported to be associated with BC in 2006 (OR = 2.0, 95% CI 1.2–3.2, p = 0.012) (Seal et al. 2006). However, several large-scale studies did not identify BRIP1 as a BC susceptibility gene (Easton et al. 2016; Hanson et al. 2022; Hu et al. 2021; Weber-Lassalle et al. 2018).
FANCB is the only known FA gene on the X chromosome (Kato et al. 2015). Deleterious variants in FANCB are rare, and none is registered in the East Asian population of GnomAD and WBBC. Additionally, no pathogenic/likely pathogenic variants in FANCB have been reported in BC patients. However, a novel FANCB frameshift variant c.1327-3dupT was identified in our cohort. This finding suggests that FANCB may be a susceptibility gene for BC.
Additionally, the association between germline mutations in other FA genes (except for FANCW/RFWD3) and BC risk has been studied. Thompson et al. (Thompson et al. 2012) identified three truncating variants in FANCC in 438 familial BC patients that were not found in healthy controls. Palmer et al. (2020) observed moderate risk for African American women carrying FANCC mutations with ER-positive BC (OR = 2.42, 95% CI 1.00–5.97, p = 0.05). Pan et al. (2019) found that FANCC c.339G > A (p.W113X) might contribute to susceptibility in Chinese familial breast and/or ovarian cancer. However, some studies showed different conclusions, that FANCC truncation variants (p.R158X and p.R548X) were not associated BC risk (OR = 0.64, 95% CI 0.32–1.29, p = 0.215 and OR = 1.03, 95% CI 0.41–2.56, p = 0.942, respectively) (Dörk et al. 2019). There was also no significant association between FANCC and BC in our cohort. A larger sample may be needed to verify the relationship of mutations in this gene and BC susceptibility.
Several studies have found that polymorphisms in FA genes are relevant to BC risk. FANCD2 c.4098 T > G (p.Leu1366_Leu1367, rs2272125) was associated with sporadic BC (OR = 1.35, 95% CI 1.09–1.67; p = 0.005) (Barroso et al. 2006). In a cohort of Sri Lankan women, XRCC2 c.*1772G > A (rs3218550) increased the risk of BC (OR = 1.525, 95% CI 1.107–2.101, p = 0.0098) (Sirisena et al. 2018). However, RAD51 c.-1271A > G (rs503078) was found to significantly reduce BC risk (OR = 0.5, 95% CI 0.3–1.0, p < 0.05) (Grešner et al. 2020). ERCC4 c.*971C > G (rs2276466) and other mutations have not been associated with BC risk (Sahaba et al. 2022). In conclusion, germline mutations in FA genes may be related to increased BC risk. Some FA genes may be moderate-penetrance susceptibility genes, and other FA genes have low penetrance. Validation should be performed in studies with larger sample sizes.
PARP inhibitors have been successfully used in patients with breast or ovarian cancer who carry BRCA1/2 germline mutations (Litton et al. 2018; Robson et al. 2017; Weil et al. 2011). TBCRC 048 was an extended study to explore the therapeutic effect of Olaparib monotherapy in metastatic BC with germline or somatic variants in HR-related genes. Mutations in FA genes other than BRCA1/2, PALB2 and RAD51C were not identified in the study subjects (NCT03344965) (Litton et al. 2018). A clinical study evaluating the efficacy and safety of Olaparib combination immunotherapy in patients with solid tumors carrying HR-related gene mutations is ongoing (NCT04169841) (Fumet et al. 2020). Although conclusive clinical evidence for the utilization of PARP inhibitors in FA gene-mutated cancers is still lacking, a case report provided evidence that one ovarian cancer patient carrying a FANCA mutation benefitted from a PARP inhibitor (Qian et al. 2022), which suggests a potential therapeutic option for FA gene-mutated cancers.
There were some limitations in our study. First, this study focused on high-risk hereditary BC cases, which may lead to selection bias in determining the mutation frequencies of FA genes. Second, the median follow-up time was 38 months, and a longer follow-up time is needed to assess prognosis. Third, the number of FA gene mutation carriers was small, so the association between mutations and BC risk could not be confidently evaluated. Fourth, the panel did not cover FANCV/REV7 (Bluteau et al. 2016) and FANCW/RFWD3 (Knies et al. 2017) because this study was designed before they were identified as FA genes.
Conclusions
To our knowledge, this is the first study to comprehensively investigate FA gene mutations in a relatively large cohort of Chinese BC patients with high genetic risk. This study estimated the prevalence, clinicopathological characteristics, prognosis and risk of BC associated with deleterious variant in FA genes. This exploration enriches our understanding of the role of FA genes in Chinese BC patients. Studies with larger samples are needed to confirm these findings and aid clinical management.
Data availability
The data that support the findings of this study are available upon request from the corresponding author.
References
Badra Fajardo N et al (2022) Fanconi anemia proteins and genome fragility: unraveling replication defects for cancer therapy. Trends Cancer 8(6):467–481
Barroso E et al (2006) FANCD2 associated with sporadic breast cancer risk. Carcinogenesis 27(9):1930–1937
Bluteau D et al (2016) Biallelic inactivation of REV7 is associated with Fanconi anemia. J Clin Invest 126(9):3580–3584
Castéra L et al (2014) Next-generation sequencing for the diagnosis of hereditary breast and ovarian cancer using genomic capture targeting multiple candidate genes. Eur J Hum Genet 22(11):1305–1313
Cong K et al (2021) Replication gaps are a key determinant of PARP inhibitor synthetic lethality with BRCA deficiency. Mol Cell 81(15):3128-3144.e3127
Daly MB et al (2021) Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 19(1):77–102
Del Valle J et al (2020) Exploring the role of mutations in fanconi anemia genes in hereditary cancer patients. Cancers (basel) 12(4):829
Dörk T et al (2019) Two truncating variants in FANCC and breast cancer risk. Sci Rep 9(1):12524
Dorling L et al (2021) Breast cancer risk genes—association analysis in more than 113,000 women. N Engl J Med 384(5):428–439
Easton DF et al (2015) Gene-panel sequencing and the prediction of breast-cancer risk. N Engl J Med 372(23):2243–2257
Easton DF et al (2016) No evidence that protein truncating variants in BRIP1 are associated with breast cancer risk: implications for gene panel testing. J Med Genet 53(5):298–309
Fang CB et al (2020) Fanconi anemia pathway: mechanisms of breast cancer predisposition development and potential therapeutic targets. Front Cell Dev Biol 8:160
Figlioli G et al (2019) The FANCM:p.Arg658* truncating variant is associated with risk of triple-negative breast cancer. NPJ Breast Cancer 5:38
Fumet JD et al (2020) Precision medicine phase II study evaluating the efficacy of a double immunotherapy by durvalumab and tremelimumab combined with olaparib in patients with solid cancers and carriers of homologous recombination repair genes mutation in response or stable after olaparib treatment. BMC Cancer 20(1):748
Gianni P et al (2022) The Fanconi anemia pathway and Breast Cancer: a comprehensive review of clinical data. Clin Breast Cancer 22(1):10–25
Grešner P et al (2020) Rad51 paralogs and the risk of unselected breast cancer: a case-control study. PLoS ONE 15(1):e0226976
Hallajian Z et al (2017) Simultaneous ATM/BRCA1/RAD51 expression variations associated with prognostic factors in Iranian sporadic breast cancer patients. Breast Cancer 24(4):624–634
Hanson H et al (2022) UK consensus recommendations for clinical management of cancer risk for women with germline pathogenic variants in cancer predisposition genes: RAD51C, RAD51D, BRIP1 and PALB2. J Med Genet 60(5):417–429
Houghtaling S et al (2003) Epithelial cancer in Fanconi anemia complementation group D2 (Fancd2) knockout mice. Genes Dev 17(16):2021–2035
Hu C et al (2021) A population-based study of genes previously implicated in breast cancer. N Engl J Med 384(5):440–451
Jacquemont C et al (2012) Non-specific chemical inhibition of the Fanconi anemia pathway sensitizes cancer cells to cisplatin. Mol Cancer 11:26
Kalb R et al (2007) Hypomorphic mutations in the gene encoding a key Fanconi anemia protein, FANCD2, sustain a significant group of FA-D2 patients with severe phenotype. Am J Hum Genet 80(5):895–910
Kato Y et al (2015) FANCB is essential in the male germline and regulates H3K9 methylation on the sex chromosomes during meiosis. Hum Mol Genet 24(18):5234–5249
Kiiski JI et al (2014) Exome sequencing identifies FANCM as a susceptibility gene for triple-negative breast cancer. Proc Natl Acad Sci U S A 111(42):15172–15177
Kiiski JI et al (2017) FANCM mutation c.5791C>T is a risk factor for triple-negative breast cancer in the Finnish population. Breast Cancer Res Treat 166(1):217–226
Kim H et al (2012) Regulation of DNA cross-link repair by the Fanconi anemia/BRCA pathway. Genes Dev 26(13):1393–1408
Knies K et al (2017) Biallelic mutations in the ubiquitin ligase RFWD3 cause Fanconi anemia. J Clin Invest 127(8):3013–3027
Kuchenbaecker KB et al (2017) Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA 317(23):2402–2416
Kurian AW et al (2014) Clinical evaluation of a multiple-gene sequencing panel for hereditary cancer risk assessment. J Clin Oncol 32(19):2001–2009
LaDuca H et al (2014) Utilization of multigene panels in hereditary cancer predisposition testing: analysis of more than 2,000 patients. Genet Med 16(11):830–837
Litton JK et al (2018) Talazoparib in patients with advanced breast cancer and a germline BRCA mutation. N Engl J Med 379(8):753–763
Mamrak NE et al (2017) Recent discoveries in the molecular pathogenesis of the inherited bone marrow failure syndrome Fanconi anemia. Blood Rev 31(3):93–99
Mantere T et al (2017) Case-control analysis of truncating mutations in DNA damage response genes connects TEX15 and FANCD2 with hereditary breast cancer susceptibility. Sci Rep 7(1):681
Nalepa G et al (2018) Fanconi anaemia and cancer: an intricate relationship. Nat Rev Cancer 18(3):168–185
Palmer JR et al (2020) Contribution of germline predisposition gene mutations to breast cancer risk in african american women. J Natl Cancer Inst 112(12):1213–1221
Pan ZW et al (2019) Deleterious mutations in DNA repair gene FANCC exist in BRCA1/2-negative Chinese familial breast and/or ovarian cancer patients. Front Oncol 9:169
Peterlongo P et al (2021) Protein truncating variants in FANCM and risk for ER-negative/triple negative breast cancer. NPJ Breast Cancer 7(1):130
Qian B et al (2022) Clinical benefit with PARP inhibitor for pathogenic germline FANCA-mutated relapsed epithelial ovarian cancer: a case report. Front Oncol 12:778545
Ray Chaudhuri A et al (2016) Replication fork stability confers chemoresistance in BRCA-deficient cells. Nature 535(7612):382–387
Robson M et al (2017) Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med 377(6):523–533
Sahaba SA et al (2022) The link of ERCC2 rs13181 and ERCC4 rs2276466 polymorphisms with breast cancer in the Bangladeshi population. Mol Biol Rep 49(3):1847–1856
Santarpia L et al (2013) DNA repair gene patterns as prognostic and predictive factors in molecular breast cancer subtypes. Oncologist 18(10):1063–1073
Seal S et al (2006) Truncating mutations in the Fanconi anemia J gene BRIP1 are low-penetrance breast cancer susceptibility alleles. Nat Genet 38(11):1239–1241
Simoneau A et al (2021) The trans cell cycle effects of PARP inhibitors underlie their selectivity toward BRCA1/2-deficient cells. Genes Dev 35(17–18):1271–1289
Sirisena ND et al (2018) Genetic determinants of sporadic breast cancer in Sri Lankan women. BMC Cancer 18(1):180
Solomon PJ et al (2015) A case report and literature review of Fanconi Anemia (FA) diagnosed by genetic testing. Ital J Pediatr 41:38
Sung H et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Szabo CI et al (1995) Inherited breast and ovarian cancer. Hum Mol Genet 4 Spec:1811–1817
Thompson ER et al (2012) Exome sequencing identifies rare deleterious mutations in DNA repair genes FANCC and BLM as potential breast cancer susceptibility alleles. PLoS Genet 8(9):e1002894
Tung N et al (2016) Frequency of germline mutations in 25 cancer susceptibility genes in a sequential series of patients with breast cancer. J Clin Oncol 34(13):1460–1468
Wang Y et al (2018) Correlation of FANCM expression with clinical factors in luminal B breast cancer. Breast Cancer 25(4):431–437
Weber-Lassalle N et al (2018) BRIP1 loss-of-function mutations confer high risk for familial ovarian cancer, but not familial breast cancer. Breast Cancer Res 20(1):7
Weil MK et al (2011) PARP inhibitor treatment in ovarian and breast cancer. Curr Probl Cancer 35(1):7–50
Wendt C et al (2019) Identifying breast cancer susceptibility genes - a review of the genetic background in familial breast cancer. Acta Oncol 58(2):135–146
Wooster R et al (1994) Localization of a breast cancer susceptibility gene, BRCA2, to chromosome 13q12-13. Science 265(5181):2088–2090
Yang X et al (2020) Ovarian and breast cancer risks associated with pathogenic variants in RAD51C and RAD51D. J Natl Cancer Inst 112(12):1242–1250
Yang Z et al (2023) Resistance to anti-HER2 therapy associated with the TSC2 nonsynonymous variant c.4349 C > G (p.Pro1450Arg) is reversed by CDK4/6 inhibitor in HER2-positive breast cancer. NPJ Breast Cancer 9(1):36
Zhang B et al (2010) Expression of FANCD2 in sporadic breast cancer and clinicopathological analysis. J Huazhong Univ Sci Technolog Med Sci 30(3):322–325
Zhang J et al (2014) Mechanism and regulation of incisions during DNA interstrand cross-link repair. DNA Repair (amst) 19:135–142
Zhu L et al (2022) High chromosome instability identified by low-pass whole-genome sequencing assay is associated with TP53 copy loss and worse prognosis in BRCA1 germline mutation breast cancer. Breast Cancer 29(1):103–113
Acknowledgements
We thank all those who participated in this study.
Funding
This study was funded by the Natural Science Foundation of Zhejiang Province (Grant number: LY21H160005), Basic Public Welfare Research Plan of Zhejiang Province (Grant number: LTGY23H160012), Medical and Health Science and Technology Plan Project of Zhejiang Province (Grant number: 2021KY566).
Author information
Authors and Affiliations
Contributions
WC contributed to conceptualization; RW contributed to methodology; XL contributed to software; WY involved in formal analysis; PL and JP involved in investigation; QZ, YZ and PL involved in writing—original draft preparation; QZ, PL, YZ, XW and WC involved in writing—review and editing; WC involved in supervision; WC involved in project administration; WC and XD involved in funding acquisition; all authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki and approved by Ethics Committee of Zhejiang Cancer Hospital (protocol code IRB-2017–1999, 7 December 2017).
Consent to participate
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, QY., Li, PC., Zhu, YF. et al. A comprehensive analysis of Fanconi anemia genes in Chinese patients with high-risk hereditary breast cancer. J Cancer Res Clin Oncol 149, 14303–14313 (2023). https://doi.org/10.1007/s00432-023-05236-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-05236-6