Abstract
Purpose
Depiction of pelvic lymph node metastasis (LNM) sites among patients with cervical cancer facilitates accurate determination of the extent of dissection and radiotherapy regimens.
Methods
A retrospective study of 1182 cervical cancer patients who underwent radical hysterectomy and pelvic lymph node dissection between 2008 and 2018 was performed. The number of removed pelvic lymph nodes and metastasis status in different anatomical regions was analyzed. The prognostic difference of patients with lymph node involvement stratified by various factors was analyzed by Kaplan–Meier method.
Results
The median number of pelvic lymph nodes detected was 22, mainly from obturator (29.54%) and inguinal (21.14%) sites. Metastatic pelvic lymph nodes were found in 192 patients, with obturator accounting for the highest percentage (42.86%). The patients with lymph node involvement in single site had better prognosis that those in multiple sites. The overall- (P = 0.021) (OS) and progression-free (P < 0.001) survival (PFS) curves of patients with inguinal lymph node metastases were worse compared to those with obturator site. There was no difference in the OS and PFS among patients with 2 and more than 2 lymph nodes involvement.
Conclusion
An explicit map of LNM in patients with cervical cancer was presented in this study. Obturator lymph nodes tended to be involved. The prognosis of patients with inguinal lymph node involvement was poor in contrast to that with obturator LNM. In patients with inguinal lymph node metastases, clinical staging needs to be reconsidered and extended radiotherapy to the inguinal region needs to be strengthened.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the gradual decline in cervical cancer incidence and mortality with the use of HPV vaccine and cervical screening, mounting studies have shown that patients with lymph node metastasis (LNM) continue to show poor prognosis (Olthof et al. 2022; Sakuragi 2007). The 5-year overall survival (OS) and progression-free survival (PFS) rates of patients with lymph nodes positivity at early stage were significantly lower in contrast to those without lymph node involvement (Saleh et al. 2020). Previously, we reported a significantly shorter PFS in patients with positive lymph nodes than that in negative group (Ji et al. 2022); the metastatic lymph node ratio was independent predictors for PFS (Li et al. 2020). Collectively, lymph node status exerted a pivotal role in the therapy options and prognostic evaluation of cervical cancer. Therefore, accurate evaluation of metastasis status and management these metastatic pelvic lymph nodes is important for the treatment of cervical cancer.
Systematic lymph node dissection allows for a comprehensive evaluation of LNM status, but this approach is accompanied by complications such as lymphedema and lymphocytic cysts. Currently, the technology of sentinel lymph node (SLNs) biopsy is gradually applied to early-stage cervical cancer. According to a large prospective study including 356 Chinese patients with cervical cancer, common sites of SLNs included external iliac (33.38%), obturator (30.08%), common iliac (14.90%), the internal iliac (7.35%), and less frequent sites included presacral (4.33%) and gluteal (4.33%) (Ya et al. 2021). Another study included two prospective database on SLN biopsy and found that the common sites of SLNs showed as following: interiliac/external iliac area (86.3%), common iliac area (8.5%) (Balaya et al. 2020). Clearly, there are significant differences among individuals in the topography of SLNs. Therefore, it is necessary to explore the common metastatic sites of pelvic lymph nodes and to map the metastasis of pelvic lymph nodes in a real-world study. Understanding the topography of LNM in cervical cancer might help in the preoperative evaluation of patients and the development of individualized treatment strategies. In addition, it is an urgent question whether LNM in different regions exhibit a different prognosis.
Hence, the present study aims to describe the mapping of pelvic LNM in cervical cancer and then to analyze the prognostic differences in lymph node involvement in different regions so as to offer a basis for the determination of radiotherapy field or other individual treatment in cervical cancer patients.
Materials and methods
Patients
1182 patients were diagnosed with cervical cancer from 2008 to 2018 in the First Affiliated Hospital of Wenzhou Medical University. Radical hysterectomy and pelvic lymph node dissection were performed in all patients. Patients with distant metastasis or uncertain surgical information were excluded. All resected lymph nodes were performed with histopathological examination. All patients signed informed consent and this study was approved by the ethics committee of the First Affiliated Hospital of Wenzhou Medical University.
Variables
The characteristics utilized in the present study were as follows: age at diagnosis, tumor size, grade, lympho-vascular space invasion (LVSI), anatomical region of removed lymph node, lymph node status (node positive, node negative), FIGO stage (using the FIGO classification of 2009 (Pecorelli 2009)), OS (the time from the beginning of receiving treatment to death), PFS (the time from the beginning of receiving treatment to the onset of progression) and vital status. The cut-off time for follow-up is June 24th, 2019.
Statistical analysis
The data of age at diagnosis, the number of resected and positive lymph nodes (PLNs) were shown as median (P25-P75). The corresponding curves of OS and PFS rates were analyzed by the Kaplan–Meier method, and the comparison among the curves were analyzed through Log-rank test. P < 0.05 (two sided) was considered statistically significant.
Results
Patient characteristics
Totally, 1182 patients with cervical cancer participated in the present study, and the clinicopathological characteristics of all patients are shown in Table 1. There were 724 (61.25%) patients in FIGO I stage and 458 (38.75%) patients in FIGO II stage. Lymph node metastases were found in 192/1182 (16.24%) patients and 66 patients had ≥ 2 sites of PLNs. LNM was confirmed in 85/724 patients with FIGO I stage and 107/458 patients with FIGO II stage. Lymph nodes tended to be positive in FIGO stage II patients compared with FIGO I patients (P < 0.001). All the 1182 patients underwent pelvic lymph node dissection and there was no difference in the number of resected lymph nodes between patients with or without LNM (P = 0.530).
Anatomical distribution of detected and positive lymph nodes
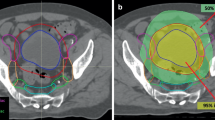
Among 1182 patients with cervical cancer, the median number of lymph nodes detected postoperatively was 22.00 (18.00–27.00). The highest percentage of resected lymph nodes were those within the obturator (29.76%), followed by those from the inguinal site (21.15%), external iliac artery (17.78%), common iliac artery (15.84%), internal iliac artery (15.47%) groups, respectively (Fig. 1).
There were 192 cervical cancer patients with PLN, of which 113 (58.85%), 47 (24.48%), 17 (8.85%), 11 (5.73%) and 4 (2.09%) patients had 1, 2, 3, 4 and 5 metastatic sites, respectively. For the number of patients with lymph node involvement in each site, the result showed that obturator group had the largest number, followed by internal iliac group (Table 2). In total, there were 617 PLNs in the 192 patients, and the distribution of LNM is shown in Fig. 2. Overall, the proportion of PLNs in the pelvic cavity were decreased from distant to proximal. The positive ratio of obturator lymph node was the highest and that of inguinal lymph node was the lowest.
Survival analysis of lymph nodes metastasis stratified by sites
As shown in Fig. 3, the OS and PFS time were higher in patients with single-site lymph node positivity than that in patients with ≥ 2 sites, respectively. Among patients with single-site lymph node involvement, the OS time and PFS time were lower in patients with inguinal involvement than in patients with obturator involvement (P < 0.05). There was no difference in prognosis between patients with inguinal metastases and iliac metastases (P > 0.05). For patients with multiple sites LNM, there was no difference in the OS or PFS among patients with distinct metastatic sites (P > 0.05).
Discussion
LNM is a common route of cervical cancer metastasis and is an independent element influencing patient survival and recurrence (Feng et al. 2021; Macdonald et al. 2009). The probability of lymph node involvement in patients with FIGO stage I and stage II has been reported to be 0–17% and 12–29%, respectively (Chen et al. 2020; Darai et al. 2008). In our study, 11.88% of patients with FIGO stage I and 23.58% of patients with FIGO stage II showed PLNs, which was consistent with the previous results. The medium dissected number of lymph nodes in the present study was 22 and was similar to previous reports (Olthof et al. 2022; Wang et al. 2020), suggesting that the extent of systematic lymphadenectomy was sufficient in our center, the quality of our procedures was assured, and our results were representative.
The lymph of the uterine cervix drains mainly to the obturator, internal iliac, external iliac, and common iliac lymph nodes, and finally to the presacral and para-aortic lymph nodes (Ercoli et al. 2010). Accordingly, system lymph node dissection mainly includes obturator, internal iliac, external iliac, common iliac, and deep inguinal lymph nodes. Although lymph node involvement in para-aortic site deteriorated the outcomes of cervical cancer patients, the benefit of para-aortic lymph nodes dissection needed further validation (Cho et al. 2020). Owing to the potential complications of lymph node resection, SLN biopsy or selective lymph node dissection was possibly considered as one of the standard therapies for early cervical cancer (Chiyoda et al. 2022; Niu et al. 2022; Poddar and Maheshwari 2021). Consequently, understanding the pattern of LNM contributed to performing lymph node related surgery. In a study of 75 cervical cancer patients, obturator site was the most common area for positive SLNs (Tu et al. 2020). However, another research showed that 44% positive SLNs were detected in external iliac area (Diaz et al. 2011). Due to the inconsistent results, the present study analyzed the pattern of LNM and showed that obturator had the highest proportion of metastasis. In conclusion, obturator was the most common site of LNM. The obturator lymph nodes need more attention during sentinel lymphoscintigraphy and should be removed in lymphadenectomy.
Our previous study showed no difference in the prognosis between patients with unilateral and bilateral lymph node metastases (Li et al. 2020). In the current study, we further analyzed the prognostic differences among cervical cancer patients with different numbers of lymph node metastases. We demonstrated that the patients with metastasized lymph node in single site had better clinical outcomes than those in multiple sites. At present, few studies have focused on the prognostic difference in patients with gynecological tumors with LNM at different sites. Chalif et al. demonstrated that PLNs in inguinal region did not deteriorate the outcomes of ovarian patients, while resection to no gross residual disease was related to better prognosis (Chalif et al. 2022). The present study investigated the prognosis of patients with lymph node involvement in distinct sites. Interestingly, we found the patients with lymph nodes positivity in inguinal site had worse outcomes compared with those in obturator site. Due to their specific anatomical position, inguinal lymph nodes did not belong to the pelvic lymph nodes and are less involved in pelvic cancers in contrast to obturator and iliac lymph nodes (Hauspy et al. 2002; Odagiri et al. 2014). Hence, we hypothesize that the prognosis of patients with inguinal LNM may be close to that of patients in the FIGO IV stage, but we need a larger sample size to further confirm our findings. In addition, extended radiation area including inguinal nodes might increase the risk of lower limb edema (Najjari Jamal et al. 2018), the radiotherapy in inguinal site tended not to be performed. Our study suggested that an extended radiation field including inguinal nodes might be helpful for patients with inguinal lymph node metastases. Intensity-modulated radiation therapy (IMRT) is an important adjuvant therapy for cervical cancer in recent years, which could strengthen the treatment of the target field and decrease the damage to the surrounding normal tissues (Lei et al. 2019), and will improve the prognosis of patients with inguinal lymphatic metastases.
Besides, there were some limitations in the present study. Many potential confounding factors might not be excluded in our retrospective study. Next, owing to the deficiency of prospective design, SLN biopsy was not analyzed in the present study. Finally, the patients were recruited from only one center and the number of participants was limited, so the results in our study needed to be validated by more subjects from multiple centers.
Conclusion
Our study mapped pelvic LNM in patients with cervical cancer and showed that obturator was the most common site of metastatic. Therefore, more attention should be paid to obturator when performing a systematic lymphadenectomy and SLN. Patients with inguinal metastases have a worse prognosis than those with obturator metastases. In patients with inguinal LNM, clinical staging needs to be reconsidered and extended radiotherapy to the inguinal region needs to be strengthened.
Data availability
The data that support the findings of this study are available from the corresponding author on reasonable request.
References
Balaya V, Guani B, Benoit L et al (2020) Diagnostic value of frozen section examination of sentinel lymph nodes in early-stage cervical cancer at the time of ultrastaging. Gynecol Oncol 158(3):576–583. https://doi.org/10.1016/j.ygyno.2020.05.043
Chalif J, Yao M, Gruner M et al (2022) Incidence and prognostic significance of inguinal lymph node metastasis in women with newly diagnosed epithelial ovarian cancer. Gynecol Oncol 165(1):90–96. https://doi.org/10.1016/j.ygyno.2022.01.026
Chen Y, Fang C, Zhang K et al (2020) Distribution patterns of lymph node metastasis in early stage invasive cervical cancer. Medicine (Baltimore) 99(42):e22285
Chiyoda T, Yoshihara K, Kagabu M et al (2022) Sentinel node navigation surgery in cervical cancer: a systematic review and metaanalysis. Int J Clin Oncol 27(8):1247–1255. https://doi.org/10.1007/s10147-022-02178-w
Cho WK, Kim YJ, Kim H et al (2020) Significance of para-aortic lymph node evaluation in patients with FIGO IIIC1 cervical cancer. Jpn J Clin Oncol 50(10):1150–1156. https://doi.org/10.1093/jjco/hyaa091
Darai E, Rouzier R, Ballester M et al (2008) Sentinel lymph node biopsy in gynaecological cancers: the importance of micrometastases in cervical cancer. Surg Oncol 17(3):227–235. https://doi.org/10.1016/j.suronc.2008.04.002
Diaz JP, Gemignani ML, Pandit-Taskar N et al (2011) Sentinel lymph node biopsy in the management of early-stage cervical carcinoma. Gynecol Oncol 120(3):347–352. https://doi.org/10.1016/j.ygyno.2010.12.334
Ercoli A, Delmas V, Iannone V et al (2010) The lymphatic drainage of the uterine cervix in adult fresh cadavers: anatomy and surgical implications. Eur J Surg Oncol 36(3):298–303. https://doi.org/10.1016/j.ejso.2009.06.009
Feng Y, Wang Y, Xie Y et al (2021) Nomograms predicting the overall survival and cancer-specific survival of patients with stage IIIC1 cervical cancer. BMC Cancer 21(1):450. https://doi.org/10.1186/s12885-021-08209-5
Hauspy J, Verkinderen L, De Pooter C et al (2002) Sentinel node metastasis in the groin detected by technetium-labeled nannocolloid in a patient with cervical cancer. Gynecol Oncol 86(3):358–360. https://doi.org/10.1006/gyno.2002.6770
Ji M, Liu Y, Hu Y et al (2022) Comparison of recurrence patterns in cervical cancer patients with positive lymph nodes versus negative. Cancer Med. https://doi.org/10.1002/cam4.4860
Lei C, Ma S, Huang M et al (2019) Long-Term survival and late toxicity associated with pelvic intensity modulated radiation therapy (IMRT) for cervical cancer involving CT-based positive lymph nodes. Front Oncol 9:520. https://doi.org/10.3389/fonc.2019.00520
Li A, Wang L, Jiang Q et al (2020) Risk stratification based on metastatic pelvic lymph node status in stage IIIC1p cervical cancer. Cancer Manag Res 12:6431–6439. https://doi.org/10.2147/CMAR.S253522
Macdonald OK, Chen J, Dodson M et al (2009) Prognostic significance of histology and positive lymph node involvement following radical hysterectomy in carcinoma of the cervix. Am J Clin Oncol 32(4):411–416. https://doi.org/10.1097/COC.0b013e31819142dc
Najjari Jamal D, Potter R, Haie-Meder C et al (2018) Physician assessed and patient reported lower limb edema after definitive radio(chemo)therapy and image-guided adaptive brachytherapy for locally advanced cervical cancer: a report from the EMBRACE study. Radiother Oncol 127(3):449–455. https://doi.org/10.1016/j.radonc.2018.03.026
Niu G, Ren Y, Zhai Y (2022) Association study between the sentinel lymph node biopsy and the clinicopathological features of patients with cervical cancer. Dis Markers 2022:9697629. https://doi.org/10.1155/2022/9697629
Odagiri T, Watari H, Kato T et al (2014) Distribution of lymph node metastasis sites in endometrial cancer undergoing systematic pelvic and para-aortic lymphadenectomy: a proposal of optimal lymphadenectomy for future clinical trials. Ann Surg Oncol 21(8):2755–2761. https://doi.org/10.1245/s10434-014-3663-0
Olthof EP, Mom CH, Snijders MLH et al (2022) The prognostic value of the number of positive lymph nodes and the lymph node ratio in early-stage cervical cancer. Acta Obstet Gynecol Scand 101(5):550–557. https://doi.org/10.1111/aogs.14316
Pecorelli S (2009) Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet 105(2):103–104. https://doi.org/10.1016/j.ijgo.2009.02.012
Poddar P, Maheshwari A (2021) Surgery for cervical cancer: consensus and controversies. Indian J Med Res 154(2):284–292. https://doi.org/10.4103/ijmr.IJMR_4240_20
Sakuragi N (2007) Up-to-date management of lymph node metastasis and the role of tailored lymphadenectomy in cervical cancer. Int J Clin Oncol 12(3):165–175. https://doi.org/10.1007/s10147-007-0661-2
Saleh M, Virarkar M, Javadi S et al (2020) Cervical cancer: 2018 revised international federation of gynecology and obstetrics staging system and the role of imaging. AJR Am J Roentgenol 214(5):1182–1195. https://doi.org/10.2214/AJR.19.21819
Tu H, Wan T, Zhang X et al (2020) Potential risks in sentinel lymph node biopsy for cervical cancer: a single-institution pilot study. World J Surg Oncol 18(1):133. https://doi.org/10.1186/s12957-020-01905-9
Wang R, Tao X, Wu X et al (2020) Number of removed pelvic lymph nodes as a prognostic marker in FIGO stage IB1 cervical cancer with negative lymph nodes. J Minim Invasive Gynecol 27(4):946–952. https://doi.org/10.1016/j.jmig.2019.08.002
Ya X, Qian W, Huiqing L et al (2021) Role of carbon nanoparticle suspension in sentinel lymph node biopsy for early-stage cervical cancer: a prospective study. BJOG 128(5):890–898. https://doi.org/10.1111/1471-0528.16504
Funding
This work was supported by National Natural Science Foundation of China (82272778), Suzhou Science and Technology Development Project (SYS2020175), Suzhou Special Project of Diagnosis and Treatment for key Clinical Disease (LCZX202013) and the Research Project of Gusu School of Nanjing Medical University (GSKY20210203).
Author information
Authors and Affiliations
Contributions
CW, HZ, SX and JZ organized and led this study, including the plan of the study, statistical analysis and manuscript draft; XW and YH contributed to statistical analysis and revision of the manuscript; CW and HZ supervised this study and revised the manuscript. All authors participated in the process of article completion and agreed the final version.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have declared no conflicts of interest.
Ethical approval
This study was approved by the Ethics Committee of the First Affiliated Hospital of Wenzhou Medical University (KY2022-R218) and informed consent was signed by the patients before taking part in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xie, S., Zhao, J., Wang, X. et al. The distribution pattern of pelvic lymph nodal metastases in cervical cancer. J Cancer Res Clin Oncol 149, 9671–9677 (2023). https://doi.org/10.1007/s00432-023-04810-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-04810-2