Abstract
Background
Day surgery has been widely carried out in medical developed countries such as Europe and the United States with high efficiency, safety and economy. The development of thoracic day surgery started late, and currently only a few top three hospitals carry thoracic day surgery. In recent years, with the continuous in-depth application of the concept of accelerated rehabilitation surgery (ERAS) in the field of surgery, thoracic surgery ERAS has also entered clinical practice with remarkable results. At present, the application of day surgery in the field of thoracic surgery is still in its infancy, and the application of robot-assisted thoracic surgery in thoracic surgery has brought new opportunities for the popularization of day surgery in thoracic surgery.
Methods
We retrospectively reviewed 86 patients underwent thoracic day surgery under the application of robot-assisted surgery system and through systematic randomization method choose 86 patients underwent conventional thoracic surgery under the application of robot-assisted surgery system at our Institute between 2020 and 2022. We analyzed the clinical and pathological features between the two groups.
Results
The clinical feature of location of the nodules, the size of nodules, pN, histology and postoperative complications were homogenous between the two groups. The average age was significantly higher in the conventional mode group, the ratio of male patients and the patients with history of smoking were significantly lower in day-surgery mode group. The major surgical method in conventional mode group was lobectomy resection (48.8%). While the segmental resection was the major surgical in day surgery mode group. The hospital stay and the time of drain was significant longer in conventional mode group. And the total medical cost in conventional was more than day-surgery mode group. While the histology and postoperative complications were homogenous between the two groups.
Conclusion
Before this, day surgery and robotics assistant surgery in thoracic surgery had been proved feasibility and safety. However, there was no report of day surgery unit robotics assistant thoracic surgery. Our clinical practice demonstrated that the method of day surgery unit robotics thoracic surgery is feasibility and safety enough.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, the incidence and mortality of lung cancer ranks first among male malignant tumors and second among women (Mattiuzzi and Lippi 2019). Similarly, lung cancer is the most common malignant tumor in China (Yuan Ye and Hecheng 2020). At present, surgical resection combined with chemotherapy, radiotherapy, implant therapy and immunotherapy are the main treatment of lung cancer. The surgical method has gradually developed from the early thoracotomy to the minimally invasive surgery based on thoracoscopic assisted surgery, to the rapid rise of robotic assisted surgery nowadays. Da Vinci surgical system is currently a widely used in clinical applications. However, there was no report about the robotic devices and platforms implemented in day surgery. Here, we tried to using the Da Vinci surgical system in day surgery of patients with lung cancer.
Day surgery is the admission of selected patients to hospital for a planned surgical procedure after which they return home the same day. With the changing in technological advances in medicine, the need of improve the cost-effectiveness of health services, and the expectation of decreasing surgical waiting list, day-surgery stems was widely applied in practice. Day surgery is preferable for the majority of patients undergoing minor surgery and it has been shown to be safe, efficient, convenient, economical and able to soften the emotional impact of an operation (Suhonen et al. 2007, 2008).
Accelerated recovery surgery (enhanced recovery after surgery, ERAS), also known as fast-track surgery (FTS), was first proposed by the Danish scholar Kehlet in 1997 (Che 2019). ERAS aims to reduce the stress response of trauma and to promote rapid functional recovery. In the extension is reflected in clinically reducing the incidence of complications and shortening the hospital stay. The ERAS rested on several components: a multidisciplinary team working together around the patient; a multimodal approach to resolving issues that delay recovery and cause complications; a scientific, evidence-based approach to care protocols; and a change in management using interactive and continuous audit (Ljungqvist et al. 2017). Data suggest that ERAS processes can reduce complications by 10% to 20% or more by supporting units to adopt evidence-based care (Gustafsson et al. 2011; Group EC 2015; Varadhan et al. 2010; Greco et al. 2014). The successful implementation of the ERAS concept in thoracic surgery has made it possible for part of the thoracic surgery to be completed in the day ward. At the same time, the day-time operation of thoracic surgery is also a further concentrated embodiment of the implementation of the ERAS concept.
Due to the COVID-19 pandemic, almost all patients admitted to medical institutions undergo CT screening, and a large number of tiny lung nodules, some of which are suspected to be malignant tumors, have been found to further increase the detection rate of early lung cancer. The surgical operation for patients with these tiny nodules is relatively simple, coupled with the delicate operation of robotic surgery, making it possible to perform robotic thoracic surgery in the day surgery ward. Here, we summarized the experience in robotic day surgery and introduced in this paper.
Methods
Patients’ selection
Some simple thoracic surgery has been clearly indicated for day surgery, such as sympathetic nerve chain block, small and benign mediastinal tumor resection, pulmonary bulla ligation, and wedge resection of the lung. These operations can be completed using thoracoscopic surgery rather than a robot. Researchers have explicit the VATS value for day surgery in those diseases (Zhang et al. 2022; Dong et al. 2021).
From 12, 2020 to 8, 2022, a total of 86 patients underwent Robotic assisted thoracic day-surgery in this time period. In the same time, we randomly choose 86 patients that underwent conventional robotic assisted thoracic surgery in the same period.
Surgery approach
Thoracic surgery with an estimated operation time of < 3 h has the potential to perform Robotic assisted thoracic day-surgery (RATDS). These operations are mainly those with low risk, short operation time, little impact on physical function and fewer postoperative complications. Lobectomy or simple segmental resection (RS1, RS2, RS6, LS1 + 2, LS1 + 2 + 3, LS4 + 5 and LS6) can be performed using robot system in the day surgery ward. Other surgery suitable for perform RATDS includes bullectomy, thoracic duct ligation, pericardial cyst resection and esophageal leiomyoma resection. Since systemic lymph node dissection will affect the length of hospital stay, RATDS only performed among patients requiring lymph node sampling.
Pre-administration and preparation
Preparation for admission lasts 2 weeks, including pre-admission examination, physical excise, and pre-admission nutrition management. Exercise cardiopulmonary function test, PET-CT, chest CT, and lung nodules 3D reconstruction are routine examinations before admission. We recommend exercises that fit daily activities for preoperative cardiopulmonary exercises. Propaganda and education are realized through the Internet Hospital network platform. We recommended 30 min of moderate intensity exercise every day (exercise heart rate greater than 120 bpm), such as stairs climbing and jogging. Since the patients with pulmonary nodules were found by routine physical examination, the general condition of the patients was relative well, which do not require additional nutritional supplements.
Intraoperative management
The execution of surgical operations in day wards places higher demands on the surgeon and requires proficiency in robotic operations. Long-term lung air leakage can cause delay in extubation. It is necessary to prevent air leakage during the operation as much as possible. The main methods include avoiding lung traction during operation, the use of cutting closure devices, and avoiding lung tissue burning. Minimize postoperative drainage including, reduce sudden separation, use of ultrasonic scalpel, and avoid invalid surgical operations. The anatomy of the pulmonary artery and vein does not require much exposure while ensuring the clipping and the safety of the operation. Indocyanine green was used to determine the intersegment plane during the operation. The robot operation uses three surgical arms and uses a small 2 cm incision as an auxiliary incision for instrument introduction and specimen removal.
Anesthesia and pain management
The anesthesiologist participated in the pre-surgery evaluation the day before the operation. Anesthesia is routinely performed by double-lumen intubation. There are three methods for postoperative pain, intravenous non-steroidal analgesics, intercostal nerve block, patient controlled analgesi (PCA) and subcutaneous fentanyl patch. We carried out multimodal analgesia mode: self-controlled analgesia pump combined with oral medication. And minimize the use of opioids. The postoperative pain evaluation of patients used visual analogue scale (VAS).
Post-operative drain management
All patients in day-surgery mode used 16F urinary tube, while the patients of conventional mode used 28F drainage tube for drainage. In day surgery patients, the drainage volume is less than 100 ml for 24 h after surgery, so the drainage volume is not our main indication of extubation. The patients in this group were rechecked on the chest radiograph 8 h after the operation. And patients in conventional group were rechecked on the chest radiograph 24 h after the operation. If the lung recruitment is good and the patient coughs without large-scale water column fluctuations in the chest drainage bottle, the tube can be extubated. The entire day-surgery group of surgical patients does not need to insert a urinary tube but the patients of conventional group need to insert a urinary tube.
Post-operative rehabilitation training
Post-operative rehabilitation training is mainly carried out by the rehabilitation department. It is mainly composed of the following aspects: (1) life guidance, including guidance on patients' diet and sleep; (2) breathing exercise training: including breathing training exercises, aerobic training, respiratory muscle training and fatigue testing; (3) postoperative cardiopulmonary function assessment.
Discharge standard
The discharge criteria are mainly completed through symptom assessment and imaging examination. On the second day after surgery, the patient can get out of bed and exercise autonomously, and the 6 min walk test is greater than 300 m. There were no hemothoraxes, pneumothorax, and atelectasis on chest radiograph.
Histopathological examination
All specimens were formalin-fixed, paraffin-embedded, and stained with hematoxylin and eosin. And the pathological classification were evaluated by at least three experienced pathologist and graded according to the World Health Organization classification for NSCLC.
Follow-up management
Taken by discharged patients. Follow-up management relies on the network and telephone mode; the network mode mainly uses the Internet hospital platform to evaluate the postoperative imaging data of patients in lower level hospitals through the network hospital mode. If the patient has serious complications such as high fever and severe chest tightness, he can be transferred to the medical consortium unit of our hospital, and the attending physician of our department will have a network remote consultation to guide the treatment.
Statistical analysis
Statistical analyses were performed using the SPSS25.0. Non-parametric tests were used for comparisons, and data were expressed as median (standard deviation). The significance threshold was p < 0.05.
Result
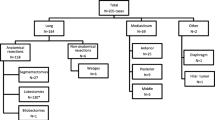
As shown in Table 1, the average age of all patients was 43.8 ± 12.1 years. 56 patients were male and 116 patients were female. There were 26 (15.1%) patients with a history of smoking while 146 (84.9%) patients without a history of smoking. The lesions of 61 (35.5%) patients were located in right upper lobe, 28 (16.3%) were located in right middle lobe, 22 (12.8%) were located in right lower lobe, 42 (24.4%) were located in left upper lobe and 19 (11.0%) were located in left lower lobe. Among the 172 patients, 62 (36.1%) patients were underwent with lobectomy resection, 89 (51.7%) patients were underwent with segmental resection and 21 (12.2%) patients were underwent with wedge resection. The average size of nodules was 16.8 ± 8.3 mm. Mostly except for five patients after postoperative staging were in stage I or II according to the 8th TNM classification.
Median hospital stay was 6.0 ± 5.5 days and the day-surgery mode group had shorter hospital stay compared with the conventional mode group (2.1 ± 0.7 days vs 9.9 ± 5.5 days). The average medical cost was 75,579.5 ± 14,060.4 yuan, and the day-surgery mode group showed to pay less medical cost compared with conventional mode group (67,049.1 ± 7520.6 yuan vs 84,109.0 ± 13,925.1 yuan). The average time of drain was 2.4 ± 1.5 days and the day-surgery mode group had shorter time of drain than conventional mode group (1.6 ± 0.5 days vs 3.2 ± 1.7 days). While the average drain value was 253.1 ± 203.3 ml, and there were no difference between the two groups. The two groups were homogeneous with histology. There were 6 (7.0) patients had postoperative complications in day-surgery mode group and 8 (9.3) patients in conventional mode group, and there was no difference between the two groups.
Discussion
In recent years, the spectrum of lung cancer disease has evolved, and the application of minimally invasive thoracoscopic surgery to treat small nodules and early lung cancer has basically reached a consensus, which has also laid the foundation for the development of thoracic surgery day surgery. Day surgery refers to a treatment mode that completes the patient's admission treatment, surgical treatment, postoperative observation, and rehabilitation and discharge within 24 h. The concept was proposed by pediatric surgeon James Nicoll in 1909. The definition of day surgery was formulated by International Day Surgery Association in 2003. Combined with the international experience and actual domestic medical situation, China Ambulatory Surgery Alliance (CASA) had redefined the day surgery as the patients completed the operation and was discharged within 24 h. And they emphasized: first, day surgery is a planned operation for the patient in addition to outpatient surgery. Second, for patients who need to extend the hospital stay due to changes in special conditions and the patient’s own disease progression, the longest time should not exceed 48 h. Evidences has now available to support a day-case approach to some different thoracic procedures, both diagnostic and therapeutic. In 1990s, mediastinoscopy and anterior mediastinotomy was reported as a safe and routine outpatient procedure (Vallieres et al. 1991; Cybulsky and Bennett 1994). And in the beginning of twenty-first century, thoracotomy and thoracoscopy for lung biopsies has been showed to be a safety and effectiveness day-case procedure (Blewett et al. 2001; Chang et al. 2002). More recently, video-assisted thoracoscopic surgery (VATS) has been successfully implemented in thoracic sympathectomy and surgery for pneumothorax as day-case procedures (Elia et al. 2005; Malik and Black 2009). Advances in anesthesia, surgical techniques and the development of enhances recovery pathways had allowed increasingly more complex surgical procedures to be successfully undertaken. Research had demonstrated that lung lobectomy can be safety and feasibility in day-case surgery (Tovar et al. 1998; Tovar 2001). The results fully demonstrated that the modern surgical concept of minimally invasive surgical technology and precise resection and optimization of perioperative process management has laid the theoretical and practical foundation for the development and implementation of day surgery in thoracic surgery by ERAS. It is necessary to ensure the safety and rehabilitation of people of different ages after discharge, while effectively saving resources, and which can ensure the quality and safety of patients in an all-round way. Although the day surgery model of thoracic surgery has been gradually developed, the safety and satisfaction of the patients are still most important and must be considered. That is so day surgery combined with ERAS can improve safety and increase satisfaction of patients. In our research, we compared day surgery thoracic robotic assistant surgery mode with conventional thoracic robotic assistant surgery mode. The results showed that the hospital stay and the time of drain in day surgery mode group was significantly shorter than conventional mode, while the total medical cost of day surgery group was less than conventional group. Moreover, the postoperative complication between the two groups had no difference. On the one hand, those results showed that thanks to the application of ERAS, day surgery mode can shorten the hospital stay and time of drain, and cut off the total medical cost. On the other hand, our study demonstrated that day surgery mode wound not increase the incidence rate of postoperative complications. It indicated that day surgery mode of thoracic surgery incorporating the concept of ERAS is a safe and effective surgical mode.
The feasibility of robotic thoracic day surgery is mainly reflected in the following aspects. The first is that this year's new crown epidemic has led to a large number of CT screenings for healthy people, which has further increased the detection rate of small lung nodules. The increase in early-stage patients has relatively low surgical complexity, and more anesthesia and intraoperative risks; a large number of young patients found on screening have lower perioperative risks compared to elderly lung cancer patients. Coupled with the use of robotic surgery, day-to-day lung cancer surgery is more feasible. The establishment of a robotic surgery ward for day thoracic surgery is a concrete manifestation of rapid rehabilitation of thoracic surgery. Among them, although the quality of surgery is the most important factor to ensure rapid recovery of patients, other interventions, including pre-hospital management and postoperative management are also very important.
Delicate intraoperative operation is an important factor in achieving robotic day-time lung cancer surgery. The main goals of the intraoperative operation are reduced drainage, prevent alveolar air leakage, and refine the resection. The delicate operation of robotic surgery can reduce the amount of drainage to a great extent, but it is still necessary to pay attention to reducing the number of sudden separations, reducing the skeletalization of blood vessels, and using more energy devices. It is worth noting that even with the above goals, the standard lymph node dissection is still strictly implemented in the absence of comprehensive reports in the current literature.
Preoperative and postoperative management is also a key step in day robotic surgery. It needs to be emphasized that preoperative and postoperative management requires the cooperation of a multidisciplinary team. Summarizing the experience of standardized management of patients undergoing robotic lung cancer surgery requires at least the multidisciplinary cooperation of anesthesiology, pain, rehabilitation, day surgery ward, and thoracic surgery. The anesthesiology department conducts preoperative evaluation and develops anesthesia methods. The pain department conducts perioperative pain management programs. The Rehabilitation Department is responsible for preoperative exercise cardiopulmonary function assessment, cardiopulmonary function rehabilitation, and guidance for discharge rehabilitation. It must be emphasized that teamwork plays an important role in the entire perioperative period of day robotic thoracic surgery.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Blewett CJ, Bennett WF, Miller JD et al (2001) Open lung biopsy as an outpatient procedure. Ann Thorac Surg [j] 71:1113–1115
Chang AC, Yee J, Orringer MB et al (2002) Diagnostic thoracoscopic lung biopsy: an outpatient experience. Ann Thorac Surg 74:1942–1946
Che G (2019) Proper selection of enhanced recovery after surgery programs between the medical service and medical intervence - is it time to do? Zhongguo Fei Ai Za Zhi 22:681–686
Cybulsky IJ, Bennett WF (1994) Mediastinoscopy as a routine outpatient procedure. Ann Thorac Surg 58:176–178
Dong Y, Shen C, Wang Y et al (2021) Safety and feasibility of video-assisted thoracoscopic day surgery and inpatient surgery in patients with non-small cell lung cancer: a single-center retrospective cohort study. Front Surg 8:779889
Elia S, Guggino G, Mineo D et al (2005) Awake one stage bilateral thoracoscopic sympathectomy for palmar hyperhidrosis: a safe outpatient procedure. Eur J Cardiothorac Surg 28:312–317
Greco M, Capretti G, Beretta L et al (2014) Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg 38:1531–1541
Group EC (2015) The impact of enhanced recovery protocol compliance on elective colorectal cancer resection: results from an international registry. Ann Surg 261:1153–1159
Gustafsson UO, Hausel J, Thorell A et al (2011) Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg 146:571–577
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: a review. JAMA Surg 152:292–298
Malik M, Black EA (2009) Fast-track video-assisted bullectomy and pleurectomy for pneumothorax: initial experience and description of technique. Eur J Cardiot Surg 36:906–909
Mattiuzzi C, Lippi G (2019) Current cancer epidemiology. J Epidemiol Glob Health 9:217–222
Suhonen RA, Iivonen MK, Valimaki MA (2007) Day-case surgery patients’ health-related quality of life. Int J Nurs Pract [j] 13:121–129
Suhonen R, Virtanen H, Heikkinen K et al (2008) Health-related quality of life of day-case surgery patients: a pre/posttest survey using the EuroQoL-5D. Qual Life Res 17:169–177
Tovar EA, Roethe RA, Weissig MD et al (1998) One-day admission for lung lobectomy: an incidental result of a clinical pathway. Ann Thorac Surg 65:803–806
Tovar EA (2001) One-day admission for major lung resections in septuagenarians and octogenarians: a comparative study with a younger cohort. Eur J Cardiothorac Surg 20:449–453
Vallieres E, Page A, Verdant A (1991) Ambulatory mediastinoscopy and anterior mediastinotomy. Ann Thorac Surg 52:1122–1126
Varadhan KK, Neal KR, Dejong CH et al (2010) The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr 29:434–440
Yuan Ye JR, Hecheng L (2020) Robotic surgery in lung cancer treatment: current status and prospects. J Clin Surg 28:601–604 (in Chinese)
Zhang G, Fan J, Yu Z et al (2022) Video-assisted thoracoscopic treatment as two-day surgery for lung neoplasms: a propensity-matched analysis. BMC Cancer [j] 22:832
Funding
This work is supported by the Natural Science Foundation General Program of Hunan Province (2018JJ3821), Project of scientific research plan of Hunan provincial health commission (C2019185), and Innovation-Driven Project of Central South University (2020CX043),and National Multidisciplinary Cooperative Diagnosis and Treatment Capacity Building Project for Major Diseases (Lung Cancer).
Author information
Authors and Affiliations
Contributions
All authors have contributed to the preparation of this manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests. Drs. Xin Li, Yuanqi Liu, Yanwu Zhou, Professors Yang Gao, Chaojun Duan and Chunfang Zhang have no conflicts of interest or financial ties to disclose.
Ethical approval
This is an observational study. The ethics committee of Xiangya Hospital, Central South University (CSU; Changsha, China) has confirmed that no ethical approval is required.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, X., Liu, Y., Zhou, Y. et al. Day surgery unit robotics thoracic surgery: feasibility and management. J Cancer Res Clin Oncol 149, 7831–7836 (2023). https://doi.org/10.1007/s00432-023-04731-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-04731-0