Abstract
Purpose
Women with BRCA1 and BRCA2 (BRCA1/2) pathogenic/likely pathogenic (P/LP) variants have a higher risk to develop breast and ovarian cancer. In structured high-risk clinics, risk-reducing measures are adopted. This study aimed at characterizing these women and identify factors that may have influenced their choice between risk reduction mastectomy (RRM) and intensive breast surveillance (IBS).
Methods
This study reviewed retrospectively 187 clinical records of affected and unaffected women with P/LP variants of the BRCA1/2 genes, from 2007 to 2022, of which 50 chose RRM, while 137 chose IBS. The research focused on personal and family history and tumor characteristics and their relation with the preventive option chosen.
Results
Among women with personal history of breast cancer, a higher proportion opted for RRM compared to those asymptomatic (34.2% vs 21.3%, p = 0.049), with younger age determining the option for RRM (38.5 years vs 44.0 years, p < 0.001). Among women with personal history of ovarian cancer, a higher proportion opted for RRM compared to those without that history (62.5% vs 25.1%, p = 0.033), with younger age determining the option for RRM (42.6 years vs 62.7 years, p = 0.009). Women who had bilateral salpingo-oophorectomy were more likely to choose RRM than those who did not (37.3% vs 18.3%, p = 0.003). Family history was not associated with preventive option (33.3% vs 25.3, p = 0.346).
Conclusions
The decision for the preventive option is multifactorial. In our study, personal history of breast or ovarian cancer, younger age at diagnosis, and previous bilateral salpingo-oophorectomy were associated with the choice of RRM. Family history was not associated with the preventive option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hereditary breast cancer corresponds to 5–10% of all breast cancer cases (Mahdavi et al. 2019). Patients with pathogenic/likely pathogenic (P/LP) variants in a high-penetrance breast cancer susceptibility gene have a significant increased risk of breast cancer. The magnitude is different according to the genes involved. The P/LP variants most frequently associated with early onset hereditary breast cancer are those affecting the BRCA1 and BRCA2 (BRCA1/2) genes. These variants also increase the risk of developing cancer in other organs, especially in the ovary (Petrucelli et al. 1993).
P/LP variants in BRCA1/2 genes have an autosomal dominant transmission pattern. BRCAs’ genes are tumor suppressor genes, whose main function is DNA repair homologous recombination (Narod and Foulkes 2004). In patients carrying pathogenic variants, the BRCA1/2 genes show incomplete penetrance and the cumulative risk at the age of 80 years is up to 72% for breast cancer in BRCA1 P/LP variants carriers and up to 69% in BRCA2 P/LP variants carriers (Kuchenbaecker et al. 2017).
The increased risk of breast cancer at earlier ages leads to particular concern about preventive strategies in carriers of P/LP variants in BRCA1/2 genes. These strategies encompass risk reduction mastectomy (RRM) or intensive breast surveillance (IBS). RRM has been shown to reduce breast cancer risk by more than 95% (Ludwig et al. 2016). It is associated with psychological distress decrease, at the cost of persistent body image problems, as it is a major and irreversible procedure (den Heijer et al. 2012). IBS consists of an annual mammogram and breast magnetic resonance imaging (MRI), interspersed, and separated by 6-month intervals and clinical breast examination every half year, starting at the age of 25 (NCCN guidelines for detection, prevention, & risk reduction. Available from: https://www.nccn.org/professionals/physician_gls/#detection).
The aim of this study is to characterize women with P/LP variants in BRCA1/2 genes who are followed in a High-Risk Breast Clinic, and to identify the factors that influence their choice for one of these breast cancer preventive options: RRM or IBS.
Patients and methods
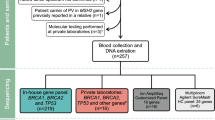
Women with known P/LP variants in BRCA1/2 genes were retrospectively identified at the Breast Center of the Centro Hospitalar Universitário de São João. The cohort consisted of women with BRCA1/2 P/LP variants diagnosed in the context of the Oncogenetic Clinics of the Centro Hospitalar Universitário de São João (genetic studies were carried out in the Genetic Department) and observed in a High-Risk Breast Clinic at the Breast Center from 30th November 2007 to 12th July 2022, who opted for a breast cancer preventive option: RRM or IBS, according to National Comprehensive Cancer Network guidelines (NCCN guidelines for detection, prevention, and risk reduction. Available from: https://www.nccn.org/professionals/physician_gls/#detection). None of them was treated with chemo-preventive agents.
Clinical information was obtained through the patients’ digital records: age at the first appointment at the High-Risk Breast Clinic; BRCA1/2 P/LP variants; parity; marital status; education level; smoking status; body mass index (BMI); age at genetic testing; personal history of breast cancer; personal history of ovarian cancer; personal history of other types of cancer; family history of breast cancer; family history of ovarian cancer; and breast cancer preventive option. In case of death, the date and cause of death was recorded.
Women with a personal history of breast cancer were considered symptomatic. In this group of women, more details concerning the breast cancer characteristics were collected: age at diagnosis, histologic type of cancer, type of surgery, other treatments, recurrence, and vital status.
The data collected from the clinical records were analyzed using the IBM® SPSS® Statistics 27 program. Descriptive statistics were used to summarize the main characteristics of the sample. Quantitative variables were summarized by measures of central tendency (mean or median, as applicable) and dispersion (standard deviation) and qualitative variables were summarized by absolute (N) and relative (%) frequency. The Chi-square or Fisher’s exact test, as appropriate, was used for comparison of proportions, while Student’s t test or Mann–Whitney test was used for comparison of means or medians, respectively. A p value < 0.05 was considered statistically significant. Groups of patients who chose IBS or RRM were compared to identify factors related to the preventive option taken.
This study was approved by the Ethics Committee of Centro Hospitalar Universitário de São João and Faculdade de Medicina da Universidade do Porto (CE 124-22). The retrospective nature of the analysis supported the informed consent waiver, for the sake of feasibility. This research ensured the privacy of patient data, since any sort of personal information that allows identification was not used or shown in the database built.
Results
Overall, 187 carriers of BRCA1/2 P/LP variants were included, with a median follow-up time of 37 months (0–168 months) from 2007 to 2022.
Patient characteristics
Table 1 summarizes the characteristics of all patients in the sample. The median age at first high-risk appointment of the women in this sample was 43 (range 18–78), and the median age at the time of genetic testing was 43 (range 18–79). Of the 187 women, 65 (34.8%) were carriers of BRCA1 P/LP variants and 122 (65.2%) were carriers of BRCA2 P/LP variants.
Of the 187 women with P/LP variants in BRCA1/2, 79 (42.2%) had a personal history of breast cancer with the median age at diagnosis of this cancer of 42 (range 24–81) and 8 (4.3%) had a personal history of ovarian cancer with the mean age at diagnosis of this cancer of 50.1 (standard deviation: 12.4). Bilateral salpingo-oophorectomy was performed in 83 (44.4%) women in this group of carriers, of which 68 (81.9%) were for risk reduction purpose. A total of 9 (4.8%) had personal history of another type of cancer (apart of breast and ovarian), including kidney, pancreas, uterus, lung, brain, and colorectal. Regarding family history, 154 (82.4%) women had a family history of breast cancer, and 18 (9.6%) women had a family history of ovarian cancer.
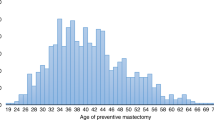
Following genetic diagnosis, this population of 187 women with BRCA1/2 P/LP variants was faced with the need to choose the preventive option for breast cancer, with 50 (26.7%) women choosing RRM and 137 (73.3%) women opting for IBS. Of the 50 women who chose RRM, 48 (84.2%) performed breast reconstruction, and of these, only one did not opt for immediate breast reconstruction. Of the women who opted for IBS, six (4.4%) developed breast cancer, with all of them being submitted to RRM of the contralateral breast. Of the asymptomatic women who opted for RRM, two (4%) developed breast cancer later.
Of the entire cohort, four (5%) women died. This corresponds to an overall survival of 95.7% (95% CI 88.3–98.5). Three deaths were not breast cancer related. The other woman died because of breast cancer progression. She belonged to the IBS group. This corresponds to a breast cancer-related mortality of 0.85% (95% CI 0.12–6.07).
Patient characteristics according to the breast cancer preventive option chosen
Table 2 compares patient characteristics between the two groups: women that opted for RRM and those who selected IBS.
No significant sociodemographic differences were observed between the two groups.
Among those women with personal history of breast cancer, there was a higher proportion who opted for RRM compared to those without personal history of breast cancer (34.2% vs 21.3%, p = 0.049). These women were younger at breast cancer diagnosis in the group that chose RRM compared to those who selected IBS (38.5 years old vs 44.0 years oçd, p < 0.001).
Likewise, among carriers with personal history of ovarian cancer, there was a higher proportion of women who opted for RRM compared to those without personal history of ovarian cancer (62.5% vs 25.1%, p = 0.033). Younger age at diagnosis in women with a history of ovarian cancer also influenced the choice of RRM (42.6 years vs 62.7 years, p = 0.009).
Women who had bilateral salpingo-oophorectomy also opted for RRM in a higher proportion compared to those who had not been submitted to bilateral salpingo-oophorectomy (37.3% vs 18.3%, p = 0.003).
Among carriers of BRCA1 P/LP variants, there was a higher proportion that opted for RRM compared to carriers of BRCA2 P/LP variants (35.4% vs 22.1%, p = 0.051), although this was a borderline result.
Breast cancer characteristics
Table 3 describes the characteristics of breast cancer in women with personal history of breast cancer (n = 79). Of the 79 women with a personal history of breast cancer, 52 (65.8%) had P/LP variants in BRCA2 gene, while 27 (34.2%) had P/LP variants in BRCA1 gene. Regarding the breast cancer preventive option, 27 (34.2%) opted for RRM, while 52 (65.8%) opted for IBS. Of the 79 breast cancers, 61 (77.2%) were invasive and 18 (22.8%) were ductal in situ. Concerning laterality of the breast cancer, 62 (78.5%) were unilateral and 17 (21.5%) were bilateral.
All these symptomatic women underwent surgery, with 52 (65.8%) having therapeutic mastectomy and 27 (34.2%) having breast-conserving surgery. Of the 52 women who underwent therapeutic mastectomy, 36 (69.2%) had reconstruction, and of these, 25 (69.4%) were immediate reconstructions. In the group who underwent mastectomy as treatment for their breast cancer (n = 52), three mastectomies had an initially risk reduction intention, considering that only in the final pathology result of the surgical specimen, the cancer diagnosis was revealed. In addition to surgical treatment, 67 (84.8%) of the symptomatic women performed chemotherapy, 51 (64.6%) radiotherapy, and 49 (62.0%) hormone therapy.
Of these 79 women with a personal history of breast cancer, seven (8.9%) had disease recurrence, three of them with local recurrence, one with regional recurrence, and three with distant recurrence (one bone, one lung, and one pelvic). Of these seven patients, five chose RRM after the initial diagnosis of breast cancer, therefore before recurrence, and two opted for RRM only after recurrence.
Family history
Table 4 compares family history according to the breast cancer preventive option chosen.
All of those who had male family members with breast cancer chose IBS (p = 0.008). While all carriers with more than one second-degree relative with ovarian cancer also opted for IBS, only 25% of those with only one second-degree relative with ovarian cancer chose the same breast cancer preventive approach (p = 0.033).
There were no significant differences related neither to family history of breast cancer nor ovarian cancer.
Discussion
This study reviewed retrospectively women with these P/LP variants in BRCA1/2 followed in a High-Risk Breast Clinic, including patients with breast cancer, with the aim to characterize this population and identify whether there are clinical, demographic, or family characteristics that could be determinant when choosing the preventive strategy.
Previous studies have shown that decision-making regarding options for coping with increased risk of breast cancer is strongly influenced by whether women know they are carriers of P/LP variants in BRCA1/2 or not. It has been clear that these women prefer more aggressive treatments, including risk-reducing surgeries compared to women without P/LP variants in BRCA1/2 (Stolier and Corsetti 2005). In our patient population, consisting only of BRCA1/2 P/LP variants carriers, 26.7% underwent RRM, compared to the literature that shows percentages that can reach 50% (Metcalfe et al. 2019). However, this number is expected to grow in the future, because data illustrate that rates of RRM have been rising over the past 20 years (Jung et al. 2020). In our sample, a more marked increase has been observed especially in more recent years, with nearly 1/4 being performed before 2015 and the other 3/4 since then.
In this study, among carriers of P/LP variants in BRCA1, there was a higher proportion who opted for RRM compared to carriers of P/LP variants in BRCA2, in line with the previous findings (Gilbert et al. 2017), although it was a borderline result. P/LP variants in BRCA1 confer a higher risk for breast cancer compared to P/LP variants in BRCA2 (Saslow et al. 2007) and RRM in women with asymptomatic BRCA1 P/LP variants has been shown to have improved survival compared to those who opted for IBS (Heemskerk-Gerritsen et al. 2019).
Women in our study population opted for RRM more often than IBS when they had personal history of breast cancer. The same occurred to women who had personal history of ovarian cancer. Also, the majority and the most recent studies corroborate our finding (Gilbert et al. 2017; Wei et al. 2021). Only about one-third of women submitted to chemotherapy opted for RRM. Due to the morbidity associated with chemotherapy, we expected that more women who underwent this treatment would opt for RRM as a preventive option for contralateral breast cancer.
Bilateral salpingo-oophorectomy not only reduces the risk of ovarian cancer of up to 80%, but also decreases the risk of developing breast cancer, especially in women before menopause who carry P/LP variants in BRCA 1/2 (Eisen et al. 2005). The literature showed that the combination of bilateral salpingo-oophorectomy and RRM provides a significant survival benefit (Ingham et al. 2013). We also found that a higher proportion of women with a bilateral salpingo-oophorectomy opted for RRM when compared to those who did not, probably justified by the predisposition of women to undergo risk reduction surgeries (Gilbert et al. 2017).
Of all the factors studied, the presence of males with breast cancer in the family and more than one second-degree relative with ovarian cancer were associated with the choice for undergoing IBS. Although these were statistically significant results, the analysis was based on a very low number of cases.
A stronger family history confers a higher lifetime risk to develop breast cancer among carriers of P/LP variants in BRCA 1/2 (Petrucelli et al. 1993; Kuchenbaecker et al. 2017), and this can impact decision-making regarding preventive choice. In addition, seeing family members undergoing cancer treatment or dying from breast cancer may also impact emotional decision-making (Henry et al. 2019). In this study, family history up to third-degree in breast cancer and second-degree in ovarian cancer did not have the expected impact in this population regarding the choice for the preventive option, as described. These results suggested that family history did not play an important role in self-risk perception in these women.
In this study, there were no significant differences in the age of genetic testing between the two groups, although younger women opted for RRM. These women were only proposed for RRM after the age of 40 years, as this is the age after which a significant increase in the development of breast cancer has been demonstrated, and normally, the reproductive project is completed (Mavaddat et al. 2013). Some studies showed that younger patients tend to choose IBS because of their desire to keep their breasts, for breastfeeding or to keep the body appearance, or because providers may not recommend RRM to young population, due to improvement in the early breast cancer detection capacity of MRI screening and in the overall risk reduction of IBS (Daly et al. 2021). Others have shown that younger age is a positive predictor for performing RRM (Manoukian et al. 2019).
Some trials concluded that women in the RRM group were more likely to be married or living with someone and having children compared to those in the surveillance group. This was also showed by us and, although the results were not statistically significant, this could be clinically relevant. The fear of leaving young children behind and the desire to live longer for the family is a significant factor in decision to undergo RRM (Haroun et al. 2011).
Women with a personal history of breast cancer accounted for almost half of the study population. There was no difference regarding bilateral carcinoma between BRCA1 and BRCA2 carriers (22.2% vs 23.1%, respectively). This was not predictable considering some studies that showed a 15-year actuarial risk of contralateral breast cancer of 36.1% for women with P/LP variants BRCA1 and 28.5% for women with P/LP variants in BRCA2 (Metcalfe et al. 2011). Another reason why women with P/LP variants in BRCA1/2 tend to undergo therapeutic mastectomy in greater proportion compared to women who do not carry these pathogenic variants is because of the higher risk of local failure to control the disease (King et al. 2015). In this symptomatic women population, 65.8% performed therapeutic mastectomy. Breast cancer recurrence in our population (8.9%) was higher than in the sporadic population undergoing mastectomy (2–3% local recurrence, 2–3% regional recurrence, and 7–9% distant recurrence) (Bargon et al. 2022). An important aspect is that these seven patients had chosen RRM after the initial breast cancer diagnosis, and five out of the seven made their choice before the recurrence, so in these women, recurrence did not seem to be an influential factor in choosing preventive surgery.
To the best of our knowledge, this is the first characterization of women with P/LP variants in BRCA1/2 in Portugal, regarding the choice for the preferred breast cancer preventive option.
These women were diagnosed, followed, and treated at a certified center, annually audited with several quality indicators (Biganzoli et al. 2017, 2020). Another strength of this study is the long follow-up (with a median of 37 months) of the patients in this high-risk clinic. Besides, it is important to emphasize some of the patients are followed since 2007.
The guidelines for the risk management of women with P/LP variants in BRCA1/2 have remained stable since the beginning of the follow-up period for the patients in this study.
However, the study has some limitations. This study is retrospective in nature. The guidelines for genetic testing and integration into the High-Risk Breast Clinic have changed over the patients' follow-up time, so it is possible that some patients who would currently make sense to be part of the study population may have been missed. The fact that this study was carried out with a population from only one institution may potentially limit the generalizability to other populations, from different geographic locations, with different cultures and/or with limited access to specialized health care. Another limitation of this study was the incomplete recording of several of the variables investigated as possible determinants of the decision-making process.
Conclusions
The choice of RRM over IBS was significantly associated with the existence of personal history of breast cancer, personal history of ovarian cancer, previous bilateral salpingo-oophorectomy, younger age at breast cancer diagnosis, and younger age at ovarian cancer diagnosis.
Family history of breast cancer and family history of ovarian cancer did not have the impact that we had expected and described by most of the literature, regarding the choice for the breast cancer preventive option. Therefore, contrary to what was predicted, family history did not play an important role in these women's perceived risk.
The data from this study highlight factors that may be important in women carrying P/LP variants in BRCA1/2 and that may help to advise these women when they are faced with this decision.
Data availability
Data are not freely available as genetic data are sensitive data, for which we are obliged legally and ethically in our country to restrict the access due to preserving patient privacy.
References
Bargon CA, Young-Afat DA, Ikinci M, Braakenburg A, Rakhorst HA, Mureau MAM et al (2022) Breast cancer recurrence after immediate and delayed postmastectomy breast reconstruction—a systematic review and meta-analysis. Cancer 128(19):3449–3469. https://doi.org/10.1002/cncr.34393
Biganzoli L, Marotti L, Hart CD, Cataliotti L, Cutuli B, Kuhn T et al (2017) Quality indicators in breast cancer care: an update from the EUSOMA working group. Eur J Cancer 86:59–81. https://doi.org/10.1016/j.ejca.2017.08.017
Biganzoli L, Cardoso F, Beishon M, Cameron D, Cataliotti L, Coles CE et al (2020) The requirements of a specialist breast centre. Breast 51:65–84. https://doi.org/10.1016/j.breast.2020.02.003
Daly MB, Pal T, Berry MP, Buys SS, Dickson P, Domchek SM et al (2021) Genetic/familial high-risk assessment: breast, ovarian, and pancreatic, version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw 19(1):77–102. https://doi.org/10.6004/jnccn.2021.0001
den Heijer M, Seynaeve C, Timman R, Duivenvoorden HJ, Vanheusden K, Tilanus-Linthorst M et al (2012) Body image and psychological distress after prophylactic mastectomy and breast reconstruction in genetically predisposed women: a prospective long-term follow-up study. Eur J Cancer 48(9):1263–1268. https://doi.org/10.1016/j.ejca.2011.10.020
Eisen A, Lubinski J, Klijn J, Moller P, Lynch HT, Offit K et al (2005) Breast cancer risk following bilateral oophorectomy in BRCA1 and BRCA2 mutation carriers: an international case-control study. J Clin Oncol 23(30):7491–7496. https://doi.org/10.1200/JCO.2004.00.7138
Gilbert E, Zabor EC, Stempel M, Mangino D, Heerdt A, Pilewskie M (2017) Differences among a modern cohort of BRCA mutation carriers choosing bilateral prophylactic mastectomies compared to breast surveillance. Ann Surg Oncol 24(10):3048–3054. https://doi.org/10.1245/s10434-017-5976-2
Haroun I, Graham T, Poll A, Sun P, Hill K, Weitzner E et al (2011) Reasons for risk-reducing mastectomy versus MRI-screening in a cohort of women at high hereditary risk of breast cancer. Breast 20(3):254–258. https://doi.org/10.1016/j.breast.2011.01.006
Heemskerk-Gerritsen BAM, Jager A, Koppert LB, Obdeijn AI, Collee M, Meijers-Heijboer HEJ et al (2019) Survival after bilateral risk-reducing mastectomy in healthy BRCA1 and BRCA2 mutation carriers. Breast Cancer Res Treat 177(3):723–733. https://doi.org/10.1007/s10549-019-05345-2
Henry DA, Lee MC, Almanza D, Ahmed KA, Sun W, Boulware DC et al (2019) Trends in use of bilateral prophylactic mastectomy vs high-risk surveillance in unaffected carriers of inherited breast cancer syndromes in the Inherited Cancer Registry (ICARE). Breast Cancer Res Treat 174(1):39–45. https://doi.org/10.1007/s10549-018-5057-7
Ingham SL, Sperrin M, Baildam A, Ross GL, Clayton R, Lalloo F et al (2013) Risk-reducing surgery increases survival in BRCA1/2 mutation carriers unaffected at time of family referral. Breast Cancer Res Treat 142(3):611–618. https://doi.org/10.1007/s10549-013-2765-x
Jung SM, Ryu JM, Park HS, Park JS, Kang E, Lee S et al (2020) Trends in risk-reducing mastectomy and risk-reducing salpingo-oophorectomy in Korean carriers of the BRCA1/2 Mutation. J Breast Cancer 23(6):647–655. https://doi.org/10.4048/jbc.2020.23.e61
King TA, Pilewskie M, Morrow M (2015) Optimal surgical management for high-risk populations. Breast 24(Suppl 2):S91–S95. https://doi.org/10.1016/j.breast.2015.07.022
Kuchenbaecker KB, Hopper JL, Barnes DR, Phillips KA, Mooij TM, Roos-Blom MJ et al (2017) Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA 317(23):2402–2416. https://doi.org/10.1001/jama.2017.7112
Ludwig KK, Neuner J, Butler A, Geurts JL, Kong AL (2016) Risk reduction and survival benefit of prophylactic surgery in BRCA mutation carriers, a systematic review. Am J Surg 212(4):660–669. https://doi.org/10.1016/j.amjsurg.2016.06.010
Mahdavi M, Nassiri M, Kooshyar MM, Vakili-Azghandi M, Avan A, Sandry R et al (2019) Hereditary breast cancer; genetic penetrance and current status with BRCA. J Cell Physiol 234(5):5741–5750. https://doi.org/10.1002/jcp.27464
Manoukian S, Alfieri S, Bianchi E, Peissel B, Azzollini J, Borreani C (2019) Risk-reducing surgery in BRCA1/BRCA2 mutation carriers: are there factors associated with the choice? Psychooncology 28(9):1871–1878. https://doi.org/10.1002/pon.5166
Mavaddat N, Peock S, Frost D, Ellis S, Platte R, Fineberg E et al (2013) Cancer risks for BRCA1 and BRCA2 mutation carriers: results from prospective analysis of EMBRACE. J Natl Cancer Inst 105(11):812–822. https://doi.org/10.1093/jnci/djt095
Metcalfe K, Gershman S, Lynch HT, Ghadirian P, Tung N, Kim-Sing C et al (2011) Predictors of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. Br J Cancer 104(9):1384–1392. https://doi.org/10.1038/bjc.2011.120
Metcalfe K, Eisen A, Senter L, Armel S, Bordeleau L, Meschino WS et al (2019) International trends in the uptake of cancer risk reduction strategies in women with a BRCA1 or BRCA2 mutation. Br J Cancer 121(1):15–21. https://doi.org/10.1038/s41416-019-0446-1
Narod SA, Foulkes WD (2004) BRCA1 and BRCA2: 1994 and beyond. Nat Rev Cancer 4(9):665–676. https://doi.org/10.1038/nrc1431
NCCN guidelines for detection, prevention, & risk reduction. https://www.nccn.org/professionals/physician_gls/#detection. Accessed 20 Nov 2022
Petrucelli N, Daly MB, Pal T (1993) BRCA1- and BRCA2-associated hereditary breast and ovarian cancer. In: Adam MP, Everman DB, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH et al (eds) GeneReviews((R)) Seattle (WA). https://www.ncbi.nlm.nih.gov/pubmed/20301425. Accessed 24 Nov 2022
Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD et al (2007) American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 57(2):75–89. https://doi.org/10.3322/canjclin.57.2.75
Stolier AJ, Corsetti RL (2005) Newly diagnosed breast cancer patients choose bilateral mastectomy over breast-conserving surgery when testing positive for a BRCA1/2 mutation. Am Surg 71(12):1031–1033
Wei G, Kumar A, Lee MC, Wang X (2021) Influential factors on risk-reduction mastectomy in a high-risk breast cancer population with genetic predispositions. Clin Breast Cancer 21(4):e427–e433. https://doi.org/10.1016/j.clbc.2021.01.008
Acknowledgments
This work was performed by a research team involved in ERN GENTURIS from CHUSJ which is a full member of ERN GENTURIS (project ID 739547); ERN GENTURIS is partly cofounded by the EU within the framework of the Third Health Programme ERN-2016—Framework Partnership Agreement 2017–2021.
Funding
Open access funding provided by FCT|FCCN (b-on). The authors declare that no funds, grants, or other supports were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by ST, BP, and AM. The first draft of the manuscript was written by ST, BP, and AM, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Centro Hospitalar e Universitário São João (124/2022).
Consent to participate
The retrospective nature of the analysis supported the informed consent waiver, for the sake of feasibility. This research ensured the privacy of patient data, since any sort of personal information that allows identification was not used or shown in the database built.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Torres, S., Peleteiro, B., Magalhães, A. et al. Differences among a Portuguese cohort of BRCA pathogenic/likely pathogenic variants carriers choosing risk-reducing mastectomy or intensive breast surveillance. J Cancer Res Clin Oncol 149, 7529–7538 (2023). https://doi.org/10.1007/s00432-023-04663-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-04663-9