Abstract
Background
The most prevalent subtype of breast cancer (BC) is luminal hormonal-positive breast cancer. The neoadjuvant chemotherapy regimens have side effects, emphasizing the need to identify new startegies.
Objective
Analyze the complete pathologic response (pCR) rate and overall response in a low-risk hormone-positive subset of patients receiving neoadjuvant hormone treatment (NAHT) with or without Palbociclib (a CDK4/CDK6 inhibitor) to boost NAHT effectiveness.
Materials and methods
Based on the upfront 21-gene Oncotype DX or low-risk Breast Recurrence Score assay (RS™), the SAFIA trial is designed as a prospective multicenter international, double-blind neoadjuvant phase-III trial that selects operable with luminal BC patients that are HER2-negative for the induction hormonal therapy with Fulvestrant 500 mg ± Goserelin (F/G) followed by randomization of responding patients to palbociclib versus placebo. The pCR rate served as the study’s main outcome, while the secondary endpoint was a clinical benefit.
Results
Of the 354 patients enrolled, 253 initially responded and were randomized to either F/G fulvestrant with palbociclib or placebo. Two hundred twenty-nine were eligible for the evaluation of the pathologic response. No statistically significant changes were observed in the pCR rates for the patients treated with the F/G therapy with placebo or palbociclib (7% versus 2%, respectively) per the Chevallier classification (Class1 + Class2) (p = 0.1464) and 3% versus 10% assessed per Sataloff Classification (TA, NA/NB) (p = 0.3108). Palbociclib did not increase the rate of complete pathological response.
Conclusion
Neoadjuvant hormonal therapy is feasible in a selected population with a low RS score of < 31
Clinical trial
NCT03447132.
Similar content being viewed by others
Introduction
Women’s breast cancer (BC) represents a significant health burden, with 2.3 million newly diagnosed cases and an estimated 685,000 deaths only during 2020 (WHO 2021). Among all cancers, BC is accountable for the highest number of total disability-adjusted life years (DALYs) (WHO 2021). BC is a complex disease that shows inter-and intra-tumoral heterogeneity (Curtis et al. 2012; Koboldt et al. 2012). This signature of BC supports a tailored approach to administering treatment modalities (Yeo and Guan 2017). Dual inhibition of the estrogen receptor (ER) and cyclin-dependent kinase 4/6 (CDK 4/6) signaling cascade holds a synergistic and anti-proliferative as well as anti-cancer potential (Finn et al. 2009). Blocking ER pathway is considered the first molecularly targeted therapeutic strategy for BC and is still used as a primary therapeutic intervention for treating ER + breast tumors (Reinert and Barrios 2015).
Fulvestrant, a selective estrogen receptor degrader (SERD), remains one of the most potent hormone therapies in metastatic BC (Suman et al. 2015; Finn et al. 2016; Turner et al. 2018a). However, fulvestrant has not been thoroughly investigated in early-stage BC or adjuvant settings (Suman et al. 2015). Palbociclib, a first-in-class CDK4/6 inhibitor, was reported to considerably improve patient outcomes when administered along with the endocrine therapy (ET) for metastatic BC (Finn et al. 2016; Turner et al. 2018a). The efficacy of treating hormone + BC with a combination of fulvestrant and palbociclib has been explored in various studies across different BC populations (Turner et al. 2018b; Cristofanilli et al. 2016a; Loibl et al. 2017).
Neoadjuvant chemotherapy (NACT) and neoadjuvant hormonal therapy (NAHT) have both been explored for the treatment of BC (Marcus et al. 2013). However, in current practice, NAHT in luminal HER2 negative BC is not commonly used. Most oncologists either favor upfront surgery or neoadjuvant chemotherapy (CT) based on a prognostic instead of a predictive approach (Ács et al. 2017; Derouane et al. 2022). Previous findings favor exploring the role of NAHT + CDK 4/6 in a neoadjuvant setting (Fisher et al. 2004a; Paik et al. 2006a).
The 21-gene expression-based Oncotype DX Breast Recurrence Score assay has previously shown a predictive and prognostic potential for BC therapeutics (Fisher et al. 2004a; Paik et al. 2006b). The assay executed on the biopsies could help select subgroups of patients with a high hormone sensitivity which could be identified as a candidate for NAHT (AlSaleh et al. 2021). The SAFIA trial is a multicenter neoadjuvant phase III trial performed in six different countries of the Middle East North Africa, abbreviated hereby as MENA region, that aims to compare the fulvestrant (± goserelin) (F/G) plus palbociclib to F/G plus Placebo in the operable luminal BC patients responsive to F/G in a double-blind fashion (AlSaleh et al. 2021). We have hereby reported the results of the analysis of the primary endpoint (pCR) and secondary endpoints: radiologic response rate, the safety of palbociclib, and upfront identification of hormone-sensitive patients using a 21-gene breast recurrence score assay.
Materials and methods
SAFIA trial design
The SAFIA study is the first BC neoadjuvant Phase III trial conceived and conducted in the MENA region between October 2017 and July 2021. (Clinical-Trials.gov identifier: NCT03447132). (AlSaleh et al. 2021). This international, prospective, multicenter, worldwide, double-blind, randomized, placebo-controlled trial compares F/G plus palbociclib (CDK 4/6 inhibitor) versus F/G plus placebo in patients with operable forms of the luminal BC cases that are HER2-negative and responding to F/G (AlSaleh et al. 2021).
Patients had a 21-gene assay that was performed centrally on the biopsies for the determination of the patients eligible for neoadjuvant HT (RS < 31) and who would be better served by either neoadjuvant chemotherapy (CT) or immediate surgery (surgery) (RS 31–100). Fulvestrant (500 mg intramuscularly on Days 1, 14, and 28, followed by the administration every four weeks for four months) and Gosereline (3.6 mg subcutaneously every four weeks in the pre- as well as peri-menopausal BC patients for five months, initiated one month before the start of Fulvestrant) were used for neoadjuvant induction treatment of RS > 31. To confirm the absence of hormone-refractory cases clinical and radiological response evaluations of the primary breast tumor and nodal disease using mammography, ultrasonography, and/or Magnetic Resonance Imaging (MRI), as appropriate, occurred after the induction of endocrine treatment. RECIST 1.1 criteria were used to characterize radiological responses. We split Stable Disease (SD) into Minor Reaction (MR) to analyze the true response more accurately against HT and, by extension, of hormone sensitivity. An increase of 1–25% in cross-product or the appearance of a new lesion is considered minor progression (MP).
All patients who responded to induction F/G with a complete response (CR), partial response (PR), or minimum response (MR) were randomized to receive either F/G with four months of palbociclib 125 mg or Placebo (3 weeks on / 1 week off every four weeks for four months). Patients with progression were excluded from the trial and treated at the investigators’ discretion by either neoadjuvant chemotherapy or surgery.
Breast and nodal surgery were performed after 8–9 months of neoadjuvant therapy. Radiation therapy and adjuvant systemic treatment were left at the investigators’ discretion. The study oversight has been provided in Supplementary Box 1.
Patient population
The study population consisted of post-or pre/peri-menopausal patients (with medical or surgical oophorectomy) with the operable forms of stage II and IIIA luminal BC (ER + , HER2-negative). The inclusion and exclusion criteria are displayed in Supplementary Table 1.
SAFIA trial endpoints
The primary endpoint was the complete pathologic response (pCR) rate induced by F/G with either palbociclib or placebo, defined as Class 1 and 2 according to the Chevallier classification. Secondary endpoints consisted of the pCR rate according to the Sataloff classification (T-A and N-A or N-B) and the radiologic response rate in both arms and safety in the MENA population. We further assessed the efficiency of upfront RS levels in predicting objective hormone sensitivity and the feasibility of the 21-gene test performed on core biopsies in the MENA patient population.
The oncotype DX 21-gene assay
Biopsy samples were sent to Genomic Health Inc (Redwood City, CA). Upfront 21-gene breast recurrence Score (RS) assay was performed following the established Standard Operating Procedures. Patients lacking sufficient tumor material either in the blocks or the slides or the unconfirmed diagnoses by Genomic Health pathologists were excluded from the trial.
Statistical analysis
Sample size calculation and randomization
The sample size calculation was primarily based on the assumption that F/G + Palbociclib would increase the pCR rate from 5% in placebo group to 15% in treatment group. The patient sample size of 260 was selected using one-sided significance testing. Considering that around 20% of the patients will demonstrate de novo resistance to induction F/G before to randomization, an additional 60 patients were required to identify 260 individuals who were responsive to induction therapy. This brought the total number of patients in the sample up to 320. In summary, given that around 20% of naive patients who had luminal tumors will be categorized as high risk (RS > 31), an additional eighty people were screened to locate 320 patients who had a score of 31. As a result, it was anticipated that a total of 400 patients would take part in the trial.
The randomization list with blinded treatment groups (A and B) was generated using the SAS procedure (PROC PLAN) and then uploaded in eCRF. Patient with no progression after four months of NAHT was randomized via eCRF. The randomization code was defined by the third-party Eurofins/LC2 (Fulvestrant, Goserelin). The unblinded code (definition of A and B) was provided to the statistician once the clinical database was locked.
Statistical methodology
The statistical analysis plan (SAP) for the trial called for three different analysis populations: (i) intent-to-treat (ITT) population: study subjects who were randomized, and treated and had surgery with histopathological results, (ii) per-protocol (PP) population: ITT population without any protocol violations that impact the study outcome. (iii) safety population: all study subjects.
To describe the demographic and baseline characteristics, descriptive statistics were used for the variables that were continuous, while frequency and percentage were used for the variables that were categorical. The ITT population group and the PP population group were both used in the investigation of efficacy.
Chi-square X2 or Fisher's exact tests were used to analyze the data and determine whether or not there was a link between the RS result and the replies to NAHT. All statistical analyses were carried out with the use of the Validated Statistical Analysis System (SAS) software, version 9.4 (SAS Institute, Cary, North Carolina, United States).
Results
Patient selection
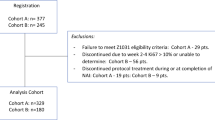
A total of 354 BC patients enrolled in six countries, with 24 centers,of the MENA region were included in the study. However, as outlined in Fig. 1, only 221 patients were evaluable (114 F/G + Palbociclib/115 for F/G + placebo) whose response to treatment could be measured because enough information was collected.
Baseline characteristics
The median age of the whole population was 49 years (ranging between 25 and 84 years), with 55% of the enrolled patients being pre/peri-menopausal (n = 195; median age 43 years) and 45% (n = 159; median age 61 years) post-menopausal.
The clinicopathological characteristics of patients eligible for induction F/G (N = 277) were as follows: Clinical stage: IIA 44%, IIB 39%, IIIA 17%. Histological Type: Ductal: 79%, Lobular: 12%, other: 9%. Histological Grade: I: 14%, II: 79%, III: 5%, missing: 2%. Ki67: ≤ 14% = 44% and > 14% = 55%, missing: 1%.
Patient distribution based on oncotype DX 21-gene assay (n = 268)
A total of 282 samples were sent for 21-gene assay with successful RS determination for 273 patients (96.7%) and failure for nine patients. The results showed RS ≥ 31 (N = 57, 20.9%) and RS < 31 (N = 216, 79.1%) with the following distribution: 0–10: 36 patients (13.2%), 11–25: 154 patients (56.4%) divided in 11–18: 92 patients (33.7%)/10–25: 19–25: 62 patients (22.7%) and 26–30: 26 patients (9.5%).
The clinicopathological characteristics of patients eligible for induction F/G according to the RS levels are shown in Supplementary Table 2. Patients with high RS levels (26–30) presented with higher histologic grades (Grade III: 31% vs. 3%), higher Ki67 (> 14%: 87% vs. 42–53%), more Luminal B (91% vs. 33–44%) compared to the lower RS levels. No differences between the RS levels regarding histologic type and clinical stage at diagnosis were seen.
Efficacy results
Response to induction F/G
A total of 266 patients were evaluable for response to induction F/G out of the 277 initially included in the clinicopathological report (Supplement Fig. 1). The non-progression rate (PR + CR + MR) was 89.8%, with PR: 63.2, CR: 2.6% for a major response rate (PR + CR) of 65.8%, and a Minor Response (MR) rate of 24%. Alternatively, 13 patients (4.9%) had a progression (PD), and 14 additional patients (5.3%) had a Minor Progression (between 1 and 25%) for a total overall progression rate (PD + MP) of 10.2%.
No statistically significant differences were observed in response when stratifying radiological responses according to hormone responsiveness and RS levels (n = 206). In contrast, Partial Response (PR) was numerically higher in the high RS (26–30) subgroup: 72% vs. 57% in the low RS (0–25) subgroup.
Radiological response assessment (investigator) after eight months of treatment (n = 226)
The radiological response assessed by investigators before surgery is displayed in Table 1. No statistically significant differences between the two arms (F/G + palbociclib or Placebo) were recorded for major response (62% vs. 66%, respectively) (p = 0.4963). However, the rate of clinical benefit (CB), defined as a major response (MR) + stable disease (SD) > 6 months, was extremely high in both arms (98% vs. 96%, respectively) with a rate of progressive disease (PD) of 2% and 4%, respectively.
Pathologic response of F/G + Palbociclib versus F/G + Placebo
Out of 253 randomized patients (ITT population), pathologic responses following surgery were available in 229 patients (Table 2). No difference was observed in the type of surgery between the two arms: conservative surgery: F/G + palbociclib (47%) versus P/G + Placebo: (48%). When considering the pCR rate according to the Chevallier classification (primary endpoint), no statistically significant difference was found between the two treatment groups: F/G + palbociclib: three patients (2%) versus P/G + Placebo: eight patients (7%) (p = 0.1464) (Supplementary Table 2). Also, per the Sataloff classification, no statistically significant difference was seen between the two arms in terms of pCR: F/G + palbociclib: four patients (3%) versus P/G + Placebo: 11 patients (10%) (p = 0.3108). The PP analysis did not show any statistically significant difference in terms of pCR when compared to the ITT population.
Safety
Adverse Events (AEs) and Serious Adverse Events (SAEs) were recorded from therapy initiation to 28 days following the administration of the last dose of the study medications (months 9 or 10). Expectedly, the main side effect in the F/G + palbociclib was neutropenia, with Grade 3–4 neutropenia reported in 25% of patients vs. 1.7% in the F/G + placebo arm. Febrile neutropenia was seen in two patients treated with F/G + palbociclib (1.7%) with no evidence of systemic infection. Other hematologic toxicities were mild (Grades 1–2) and mainly of anemia (20% for the F/G + palbociclib arm vs. 5% for the F/G + placebo arm). Non-hematologic side-effects were infrequent and low grade, reported in both arms (fatigue, arthralgia, hot flushes). Additionally, there was no significant gastrointestinal toxicity (diarrhea/nausea). No deaths were reported during this study. Palbociclib dose reductions were implemented in 19 patients (15%), with discontinuation of F/G + Palbociclib in 3 patients (2.4%). Neutropenia was 3% on Fulvestant + Palbociclib arm and 1% on Fulvestant + Placebo arm (Supplementary Table 3).
Discussion
The SAFIA trial is the first 3rd generation neoadjuvant hormonal phase III trial designed and conducted in the MENA region to test the benefits of hormonal therapy in patients with a low-risk RS (< 31) using Oncotype Dx. Oncotype Dx is highly correlated with the Ki-67 score (Sahebjam et al. 2011) and can help to eliminate the need to repeat the biopsy at day 14 to select patients who are benefiting from hormonal therapy Polley et al. 2013). In our MENA population, 21-gene assays on core biopsy specimens were possible in 97% of cases, with only 3% having insufficient carcinoma material. These results align with those found in the published literature, where failure rates are reported to lie between 4.8 and 10.2 percent; this further substantiates the usefulness of the 21-gene assay on biopsy materials for neoadjuvant therapies (Allevi et al. 2013). Over the last decade, there has been a substantial shift in the therapeutic landscape for HR + and HER2- advanced-stage breast cancer. ET as monotherapy, which was once considered the mainstay of treatment in the regimes proposed initially as well as the following lines of treatments, has been supplanted in the treatment hierarchy because of the introduction of specialized, small-molecule CDK4/6 inhibitors. In patients with advanced HR + /HER2-negative breast cancer, progression-free survival (PFS) is practically doubled when these three medications are administered in conjunction with ET. This is in comparison to patients who received ET plus a placebo in phase III trials conducted in the upfront setting with large number of subjects (MONALEESA-2 for ribociclib + letrozole (Hortobagyi et al. 2016); PALOMA-2 (Finn et al. 2016) for palbociclib + letrozole; and MONARCH-3 (Goetz et al. 2017) for abemaciclib + letrozole or Anastrozole), as well as in the populations tah have been treated previously with ET for advanced disease (MONARCH-2 for abemaciclib + fulvestrant (Sledge et al. 2017); PALOMA-3 for palbociclib + fulvestrant (Cristofanilli et al. 2016b) and MONALEESA-3 for ribociclib + fulvestrant) (Slamon et al. 2018). However, acquired or de novo resistance to CDK4/6 inhibitors is practically universal. Because of this, there has been a significant interest in establishing the potential origins of resistance, as well as strategies for overcoming resistance and diagnostic tests. In the TransNeos study, Iwata et al. reported the Recurrence Score distribution for 275 patients, comparable to the 282 patients from Asia (Iwata et al. 2019). The NP rate (PR + CR + Minor Response) for persons with an RS of 31 who were induced with NAHT using F/G was 89.8%. Using the RS < 31 21-gene assay, certain ″De Novo″ hormone-resistant tumors with a low risk of advancement (5.3% minor progression + 4.9% conventional PD = 10.2%) were found and removed.
To assess the radiological responses post-randomization and pre-surgery, we elected to use the concept of clinical benefit (CB), adding to minor response (MR) (CR + PR), stabilization > 24 weeks (Allevi et al. 2013). Our results show a very high rate of CB: 98% for F/G + Palbociclib and 96% for F/G + Placebo. In the phase II trial published by Johnston et al. the PD rate was comparable to 5.4% for Letrozole (L) and 3.2% for L + Palbociclib, with SD 45.1% and 42.5%, respectively (Johnston et al. 2019).
We did not observe a statistically significant difference was observed in pCR between F/G + Palbociclib vs. F/G + Placebo using the Chevallier classification (2% vs. 7%, respectively) nor with the Satalof classification (3% vs. 10%, respectively) either on the ITT or PP analyses. These negative results might be related to the duration of exposure to the CDK 4/6 inhibitor, which could have been too short (4 cycles). Additionally, due to the COVID-19 pandemic, surgery was significantly delayed without further exposure to Palbociclib beyond four cycles in several patients (AlSaleh 2021). The overall result suggests that clinical benefit rather than pCR will be of more use in future trials of neoadjuvant hormonal therapy.
Alternatively, the high rate of clinical benefit seen with F/G (96%) in this luminal HER2-negative BC population with low RS (<31%) plead in favor of neoadjuvant endocrine therapy, in particular when patients are reluctant for surgery or when surgical access is limited.
In terms of safety, these results provide the first prospective data related to using F/G + palbociclib in the MENA population in a neoadjuvant setting. The main toxicity was neutropenia, with grades 3–4 in 25% of the trial population. Even though only four cycles of F/G + palbociclib were delivered in this trial, these results compare favorably with the grade 3–4 neutropenia rates reported in the advanced BC Paloma 3 and 2 trials (Im et al. 2017; Iwata et al. 2017). These safety data suggest that palbociclib bears an acceptable safety profile in the MENA population. It has been noted that the mean age of our cohort is younger than the average reported in their western counterparts (Zhang et al. 2019).
Conclusion
The addition of palbociclib to neoadjuvant F/G did not increase pathologic response rates or pathologic complete response rates in HER2-negative Luminal BC that responds to induction F/G. After 8–9 months of F/G neoadjuvant therapy, a clinical benefit of 96% was attained with RS<31 tumor diagnosis and subsequent patient selection for endocrine-sensitive treatment. However, it did not appear possible to conduct a 21-gene assay on biopsy samples immediately. These results suggest that NAHT with F/G should be considered a therapeutic option, particularly in patients reluctant to surgery or when surgical access is limited.
Data availability
Data shall be shared upon request to the corresponding author.
References
Ács B, Zámbó V, Vízkeleti L, Szász AM, Madaras L, Szentmártoni G et al (2017) Ki-67 as a controversial predictive and prognostic marker in breast cancer patients treated with neoadjuvant chemotherapy. Diagn Pathol 12(1):1–12
Allevi G, Strina C, Andreis D, Zanoni V, Bazzola L, Bonardi S et al (2013) Increased pathological complete response rate after a long-term neoadjuvant letrozole treatment in postmenopausal oestrogen and/or progesterone receptor-positive breast cancer. Br J Cancer 108(8):1587–1592
AlSaleh KA (2021) Clinical trials before, during, and after COVID-19 Pandemic. Am J Clin Oncol 44(2):90–91
AlSaleh K, Al Zahwahry H, Bounedjar A, Oukkal M, Saadeddine A, Mahfouf H et al (2021) Response to induction neoadjuvant hormonal therapy using upfront 21-gene breast recurrence score assay—results from the SAFIA phase III trial. JCO Global Oncol 7:811–819
Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im SA, Masuda N et al (2016a) Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol 17(4):425–439
Curtis C, Shah SP, Chin S-F, Turashvili G, Rueda OM, Dunning MJ et al (2012) The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature 486(7403):346–352
Derouane F, van Marcke C, Berlière M, Gerday A, Fellah L, Leconte I et al (2022) Predictive biomarkers of response to neoadjuvant chemotherapy in breast cancer: current and future perspectives for precision medicine. Cancers 14(16):3876
Finn RS, Dering J, Conklin D, Kalous O, Cohen DJ, Desai AJ et al (2009) PD 0332991, a selective cyclin D kinase 4/6 inhibitor, preferentially inhibits proliferation of luminal estrogen receptor-positive human breast cancer cell lines in vitro. Breast Cancer Res 11(5):R77
Finn RS, Martin M, Rugo HS, Jones S, Im S-A, Gelmon K et al (2016) Palbociclib and letrozole in advanced breast cancer. N Engl J Med 375(20):1925–1936
Fisher B, Jeong J-H, Bryant J, Anderson S, Dignam J, Fisher ER et al (2004a) Treatment of lymph-node-negative, oestrogen-receptor-positive breast cancer: long-term findings from national surgical adjuvant breast and bowel project randomised clinical trials. The Lancet 364(9437):858–868
Fisher B, Jeong J-H, Bryant J, Anderson S, Dignam J, Fisher ER et al (2004b) Treatment of lymph-node-negative, oestrogen-receptor-positive breast cancer: long-term findings from national surgical adjuvant breast and bowel project randomised clinical trials. Lancet 364(9437):858–868
Goetz MP, Toi M, Campone M, Sohn J, Paluch-Shimon S, Huober J et al (2017) MONARCH 3: abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol 35(32):3638–3646
Haddad TC, Goetz MP (2015) Landscape of neoadjuvant therapy for breast cancer. Ann Surg Oncol 22(5):1408–1415
Hortobagyi GN, Stemmer SM, Burris HA, Yap Y-S, Sonke GS, Paluch-Shimon S et al (2016) Ribociclib as first-line therapy for HR-positive, advanced breast cancer. N Engl J Med 375(18):1738–1748
Im S, Masuda N, Im Y, Inoue K, Kim S, Redfern A et al (2017) Efficacy and safety of palbociclib plus endocrine therapy in women with hormone receptor-positive (HR+)/human epidermal growth factor receptor 2-negative (HER2-) advanced breast cancer (ABC) in the Asia-Pacific region: Data from PALOMA-2 and-3. Ann Oncol 28:x27
Iwata H, Im S-A, Masuda N, Im Y-H, Inoue K, Rai Y et al (2017) PALOMA-3: phase III trial of fulvestrant with or without palbociclib in premenopausal and postmenopausal women with hormone receptor–positive, human epidermal growth factor receptor 2–negative metastatic breast cancer that progressed on prior endocrine therapy—safety and efficacy in Asian patients. J Global Oncol 3(4):289–303
Iwata H, Masuda N, Yamamoto Y, Fujisawa T, Toyama T, Kashiwaba M et al (2019) Validation of the 21-gene test as a predictor of clinical response to neoadjuvant hormonal therapy for ER+, HER2-negative breast cancer: the TransNEOS study. Breast Cancer Res Treat 173(1):123–133
Johnston S, Puhalla S, Wheatley D, Ring A, Barry P, Holcombe C et al (2019) Randomized Phase II study evaluating palbociclib in addition to letrozole as neoadjuvant therapy in estrogen receptor-positive early breast cancer: PALLET Trial. J Clin Oncol 37:178. 30523750
Koboldt D, Fulton R, McLellan M, Schmidt H, Kalicki-Veizer J, McMichael J et al (2012) Comprehensive molecular portraits of human breast tumours. Nature 490(7418):61–70
Loibl S, Turner NC, Ro J, Cristofanilli M, Iwata H, Im SA et al (2017) Palbociclib combined with fulvestrant in premenopausal women with advanced breast cancer and prior progression on endocrine therapy: PALOMA-3 results. Oncologist 22(9):1028–1038
Marcus DM, Switchenko JM, Prabhu R, O’Regan R, Zelnak A, Fasola C et al (2013) Neoadjuvant hormonal therapy is associated with comparable outcomes to neoadjuvant chemotherapy in post-menopausal women with estrogen receptor-positive breast cancer. Front Oncol 3:317
Paik S, Tang G, Shak S, Kim C, Baker J, Kim W et al (2006a) Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol 24(23):3726–3734
Paik S, Tang G, Shak S, Kim C, Baker J, Kim W et al (2006b) Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor–positive breast cancer. J Clin Oncol 24(23):3726–3734
Polley M-YC, Leung SC, McShane LM, Gao D, Hugh JC, Mastropasqua MG et al (2013) An international Ki67 reproducibility study. J Natl Cancer Inst 105(24):1897–906
Reinert T, Barrios CH (2015) Optimal management of hormone receptor positive metastatic breast cancer in 2016. Ther Adv Med Oncol 7(6):304–320
Sahebjam S, Aloyz R, Pilavdzic D, Brisson M, Ferrario C, Bouganim N et al (2011) Ki 67 is a major, but not the sole determinant of oncotype Dx recurrence score. Br J Cancer 105(9):1342–1345
Slamon DJ, Neven P, Chia S, Fasching PA, De Laurentiis M, Im S-A et al (2018) Phase III randomized study of ribociclib and fulvestrant in hormone receptor–positive, human epidermal growth factor receptor 2–negative advanced breast cancer: MONALEESA-3. J Clin Oncol 36(24):2465–2472
Sledge GW Jr, Toi M, Neven P, Sohn J, Inoue K, Pivot X et al (2017) MONARCH 2: abemaciclib in combination with fulvestrant in women with HR+/HER2− advanced breast cancer who had progressed while receiving endocrine therapy. J Clin Oncol 35(25):2875–2884
Suman VJ, Ellis MJ, Ma CX (2015) The ALTERNATE trial: assessing a biomarker driven strategy for the treatment of post-menopausal women with ER+/Her2- invasive breast cancer. Chin Clin Oncol 4(3):34
WHO. Breast Cancer 2021 [updated 26th March, 2021]. Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer. Accessed 2 Sep 2021
Turner NC, Slamon DJ, Ro J, Bondarenko I, Im S-A, Masuda N et al (2018a) Overall survival with palbociclib and fulvestrant in advanced breast cancer. N Engl J Med 379(20):1926–1936
Yeo SK, Guan J-L (2017) Breast cancer: multiple subtypes within a tumor? Trends Cancer 3(11):753–760
Zhang T, Feng F, Yao Y, Qi L, Tian J, Zhou C et al (2019) Efficacy and acceptability of neoadjuvant endocrine therapy in patients with hormone receptor-positive breast cancer: a network meta-analysis. J Cell Physiol 234(8):12393–12403
Funding
Pfizer, AstraZeneca, and Genomic Health funded this research on the basis of investigator-initiated trials. Supplemental fund received from Deanship of Scientific Research, King Saud University, Researcher Supporting Project Number RSP-2019/88 for Dr. Khalid AlSaleh.
Author information
Authors and Affiliations
Consortia
Contributions
Authors’ Contribution: All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas, took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
K. Alsaleh: Honoraria: Amgen, AstraZeneca, Novartis, Pfizer, Roche. Research grants: Pfizer and AstraZeneca. M. Oukkal: Advisory/Consultancy, Speaker Bureau/Expert testimony: Amgen; Roche, Novartis, Pfizer, Bayer. O. Abulkhair: Advisory Board: Pfizer, Roche, Lilly, Newbridge. Hikmat Abdel-Razeq: Honoraria: Hikma Pharmaceuticals, Sanofi, Roche. J.M. Nabholtz: Research grants: Pfizer, AstraZeneca, Genomic Health, MSD. Honoraria: Amgen, AstraZeneca, MSD, Novartis, Pfizer, Roche. H. Al Zahwahry, A. Bounedjar, A. Saadeddine, H. Mahfouf, K. Bouzid, A. Bensalem, T. Fillali, B. Larbaoui, A. Kandil, H. Boussen, M. Al Foheidi, Jihen Ayari, M. Al Ghamdi, H. Errihani, M. Ghosn, N. Abdel-Aziz, M. Arafah, F. Dabouz, M. Bahadoor, S. Kullab: None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alsaleh, K., Al Zahwahry, H., Bounedjar, A. et al. Neoadjuvant endocrine therapy with or without palbociclib in low-risk patients: a phase III randomized double-blind SAFIA trial. J Cancer Res Clin Oncol 149, 6171–6179 (2023). https://doi.org/10.1007/s00432-023-04588-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-04588-3