Abstract
Background
One of the main hurdles of oncological therapy is the development of drug resistance. The ABC transporter gene family contributes majorly to cancer chemoresistance. However, effects of somatic expression of most ABC transporters on cancer outcomes remain largely unclear.
Methods
We systematically analyzed expression signatures of all 48 human ABC transporters in samples from 8562 patients across 14 different cancer types. The association between CFTR (ABCC7) expression and outcomes was analyzed experimentally using knock-downs and pharmacological CFTR stimulation.
Results
Across 720 analyzed clinical associations with patient outcomes, 363 were nominally significant of which 29 remained significant after stringent Bonferroni correction. Among those were various previously known associations, as well as a multitude of novel factors that correlated with poor prognosis or predicted improved outcomes. The association between low CFTR levels and reduced survival in lung adenocarcinoma was confirmed in two independent cohorts of 246 patients with a history of smoking (logrank P = 0.0021, hazard ratio [HR], 0.49) and 143 never-smokers (logrank P = 0.0023, HR 0.31). Further in vitro experiments using naturally CFTR expressing lung adenocarcinoma cells showed that treatment with CFTR potentiators significantly reduced proliferation at therapeutically relevant concentrations.
Conclusions
These results suggest that CFTR acts as a pharmacologically activatable tumor suppressor and constitutes a promising target for adjuvant therapy in lung adenocarcinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
ATP-binding cassette (ABC) transporters are membrane proteins that catalyze the translocation of a wide range of endogenous substrates, such as hormones, carbohydrates, various inorganic anions and antioxidants, as well as a large number of drugs. ABC transporter-mediated efflux is particularly important in oncology where it results in increased extrusion of a multitude of structurally diverse chemotherapeutic substrates, including anthracyclines, camptothecins, vinca alkaloids, taxanes and methotrexate, and constitutes a major hallmark of multidrug resistance (Xiao et al. 2021).
Increased drug efflux can be due to variation in ABC transporter genes resulting in increased transporter activity. Examples are variants in ABCB1 that can predict toxicity and response to chemotherapy in breast cancer (Xiao et al. 2020) and ABCG2 and ABCC10 variability that associates with tyrosine kinase inhibitor and taxane toxicity in non-small cell lung cancer (Noguchi et al. 2014; Sone et al. 2019). However, the predictive accuracy of ABC transporter germline variants remains low, and they are thus currently not suitable to guide cancer therapy selection and posology. In contrast to genetic variability, the expression levels of ABC transporters are more accurate in predicting chemotherapy resistance and can serve as robust biomarkers for remission and survival across various cancers, including hematological cancers, as well as various solid tumors, such as melanoma, colorectal cancer, ovarian cancer, Ewing sarcoma and breast cancer (Pasello et al. 2019; Fletcher et al. 2010). While the mechanisms underlying ABC transporter overexpression are not fully understood, causes are likely gene induction via trans acting mechanisms or the selection of intrinsically overexpressing subclones (Theile and Wizgall 2021).
While numerous studies demonstrated associations between ABC transporter expression, chemotherapy resistance and patient prognosis, most research has focused on ABCB1 (encoding P-gp/MDR1), ABCG2 (encoding BCRP) and ABCC1 (encoding MRP1), and relatively little is known about how expression levels of other ABC transporters impact multidrug resistance, remission, and survival. Importantly, the rapidly increasing wealth of large-scale cancer transcriptomic data now enables for the first time the systematic evaluation of ABC transporter expression signatures across multiple cancer types.
In this study, we comprehensively analyzed associations between expression of all 48 members of the human ABC transporter supergene family and clinical outcomes across 14 cancer types by parsing sequencing and microarray data of a total of 8,562 patients. Across 720 analyzed clinical associations, we identified 29 links between ABC expression and overall survival that were significant after stringent Bonferroni multiple testing correction. Among these, expression levels of CFTR (ABCC7) showed a significant inverse correlation with overall survival in lung adenocarcinoma (logrank P = 3*10–5; hazard ratio [HR], 0.54; 95% confidence interval [CI], 0.41–0.73), an association that was confirmed in independent lung adenocarcinoma validation cohorts of smokers (logrank P = 0.0021; HR, 0.49; CI, 0.3 to 0.78) and never-smokers (logrank P = 0.0023; HR, 0.31; CI, 0.14 to 0.68). Importantly, in vitro experiments using CFTR expressing lung adenocarcinoma cells showed that exposure to therapeutic levels of the CFTR potentiator ivacaftor, clinically approved for the treatment of cystic fibrosis, significantly reduced proliferation and showed additive effects with anthracyclines. Combined, the presented study identified CFTR expression as a prognostic marker for survival in lung adenocarcinoma and suggests that stimulation of CFTR function using safe concentrations of ivacaftor might provide a novel strategy to reduce tumor cell proliferation.
Methods
Data sources
ABC transporter expression data and the corresponding patient survival data were obtained from the cancer genome atlas program (TCGA) repository, the cancer biomedical informatics grid and the gene expression omnibus and analyzed as previously (Nagy et al. 2021; Győrffy 2021). The discovery cohort consisted of RNA sequencing data of 530 clear cell renal cell carcinoma (ccRCC), 288 papillary renal cell carcinoma (PRCC), 177 pancreatic ductal adenocarcinoma (PDAC), 371 hepatocellular carcinoma (HCC), 304 cervical squamous cell carcinoma (CSCC), 375 gastric adenocarcinoma, 501 lung squamous cell carcinoma (LSCC), 504 lung adenocarcinoma, 374 ovarian cancer, 405 bladder carcinoma, 500 head-and-neck squamous cell carcinoma (HNSCC), 259 sarcoma, 543 endometrial carcinoma, as well as microarray data of 1,496 and 1,935 breast cancer (BRCA) samples from patients who received or did not receive endocrine therapy, respectively. Survival analysis of samples with RNA sequencing information was performed as previously reported (Nagy et al. 2021). Overall survival was used as endpoint for all cancer types, except for breast cancer, for which relapse-free survival was used concordant with current recommendations (Liu et al. 2018). In addition, microarray expression data from 1,656 ovarian cancers and 719 lung adenocarcinoma samples were obtained and analyzed as previously reported for independent validations (Győrffy et al. 2012, 2013). Logrank P values were subjected to stringent Bonferroni multiple testing correction accounting for 720 tests (48 ABC transporter genes and 14 cancer types of which breast cancer samples were considered as two cohorts, one receiving endocrine therapy and one without, resulting in 48*15 = 720 tests). All analyzed data were freely available to the public for deidentified analysis and separate IRB approval was not required. P < 0.05 was considered as statistically significant.
Cell culture
Calu-3 HBT-55 cells were grown in MEM Eagle medium (Sigma) supplemented with 10% heat inactivated fetal bovine serum (FBS; Gibco), non-essential amino acids (Sigma), 2 mM l-glutamine (Sigma), 1 mM sodium pyruvate (Sigma) and penicillin–streptomycin (Cytiva). This cell line was chosen over the commonly used A549 cells as the latter do not express CFTR. Cells were propagated at 37 °C in 5%CO2 in a humidified incubator for five passages before transfection. Cells (96,000 cells/ml) were transfected in suspension with 10 nM endoribonuclease prepared siRNA consisting of a heterogeneous mixture of different CFTR targeting siRNAs target (EHU020491, Sigma) using lipofectamine RNAiMAX (Invitrogen) in antibiotics-free medium. Subsequently, the transfected cells were seeded in 24-well plates at a density of 48,000 cells per well (20% confluency). Calu-3 cells were tested negative for mycoplasma contamination.
Gene expression analysis
Total RNA was extracted using the Quick-RNA MiniPrep kit (Zymo Reseach) and 50 ng were reverse transcribed using the SuperScript III Reverse Transcriptase kit (Invitrogen). CFTR expression levels were quantified on a 7500 Fast Real-Time PCR System (Applied Biosystems) using the gene specific TaqMan probe (Hs00357011_m1, ThermoFisher) and normalized to TBP (Hs00427620_m1). Relative expression and fold-changes were calculated using the ΔΔCT method.
Western blot
Cell extracts for both knock-downs and untreated controls were prepared in RIPA buffer (Thermo) supplemented with complete protease inhibitor tablets (Roche). The total protein concentration was determined via the Lowry method (BioRad) and 10ug of total protein were separated by 10% SDS–polyacrylamide gel (Mini PROTEAN TGX, BioRad) electrophoresis. The membrane was blocked with 5% milk protein (Cell Signaling) in TBST (20 mM Tris, pH = 7,5, 150 mM NaCl, 0,1% Tween 20) and probed overnight at 4 °C with mouse monoclonal anti-CFTR antibody (sc-376683, Santa Cruz) and β-actin (A5441, Sigma-Aldrich). As secondary antibody, we used horseradish peroxidase-conjugated donkey anti-mouse IgG (A16017, Invitrogen).
Proliferation assay
48 h after transfection, cells were exposed to the CFTR potentiator ivacaftor (Sigma) and/or the anthracycline doxorubicin as indicated. The final concentration of DMSO in all treatment conditions and the control group was 0.3% v/v. Following exposure, cells were immediately placed in an incubator outfitted with an IncuCyte S3 (ESSEN Bioscience) microscope and phase-contrast images of 16 fields per well were automatically acquired every 4 h over an 80 h time course and confluence was determined automatically using the integrated software (S3 2019B Rev3). All conditions were performed in biological triplicates. Cell numbers were normalized to the first scan of the well right after the exposure. Statistical significance was determined using heteroscedastic two-tailed t tests or F tests as indicated. P < 0.05 was considered significant.
Results
Systematic analysis of ABC transporter signatures across 14 cancer types
We first parsed the expression of all 48 human ABC transporter genes across 14 different types of solid cancers using comprehensive transcriptomic data of 8,562 matched tumor and peritumoral tissue samples (Fig. 1a). Specifically for breast cancer, we stratified patients into whether or not they received endocrine therapy. When correlating tumor expression status with survival, we identified a total of 363 nominally significant associations (50.4% of all 720 tests) of which 29 remained significant after stringent Bonferroni multiple testing correction (resulting Bonferroni family-wise error threshold, 6.9*10–5; Fig. 2b). The largest numbers of significant ABC transporter associations were identified for ccRCC (n = 12), HCC (n = 5) and BRCA (n = 4 for chemotherapy and n = 3 for endocrine cohort), whereas only a single significant correlation was found for lung adenocarcinoma, PRCC, HNSCC, bladder carcinoma and ovarian cancer (Fig. 1c). No significant associations of ABC transporter expression with survival were found for endometrial cancer, sarcoma, LSCC, CSCC and gastric adenocarcinoma. Notably, the magnitude of associations between ABC expression and patient outcomes differed considerably across cancer types (Fig. 1d). Hazard ratios were overall lowest for breast cancer and HNSCC, whereas the largest effect sizes were observed for renal cancers (PRCC and ccRCC) and HCC.
The landscape of somatic ABC transporter expression alterations across 14 cancer types. a Mean-centered heatmap of the hazard ratios for expression of all 48 human ABC transporter genes across 14 different cancers. Cancer types and genes are sorted using unsupervised hierarchical clustering. Red and blue cell shades indicate reduced and increased survival in patients with elevated somatic expression. Asterisks indicate associations (n = 29) that were significant after Bonferroni correction. b Distribution of test significances. 50.4% of all associations were nominally significant (logrank P < 0.05) with 4% remaining significant after correction for multiple testing (logrank P < 6.9*10–5). c Bar plot showing the number of significant associations after multiple testing correction per cancer type. d Dot plot showing the hazard ratio distributions for the different cancer types. Significant associations after multiple testing correction are shown as red dots. Note that ABC expression effect sizes differ considerably between cancer types. BRCA breast cancer, ccRCC clear cell renal cell carcinoma, CSCC cervical squamous cell carcinoma, HCC hepatocellular carcinoma, HNSCC head-and-neck squamous cell carcinoma, LSCC lung squamous cell carcinoma, PDAC pancreatic ductal adenocarcinoma, PRCC papillary renal cell carcinoma
Association of CFTR with increased overall survival of lung adenocarcinoma patients across three independent cohorts. Kaplan–Meier plots of patient survival stratified by CFTR expression in the TCGA discovery cohort (a; n = 504 patients), as well as in two independent validation cohorts of smokers (b; n = 246 patients) and never-smokers (c; n = 143 patients) from the GeneChip data set
Drug efflux catalyzed by the multidrug resistance transporters MDR1 and MRP1 constitutes an essential mechanism of cancer chemoresistance. Previous research revealed associations of ABCB1 transcript levels with poor outcomes in ovarian cancer (Johnatty et al. 2013; Sun et al. 2016), gastric cancer (Oliveira et al. 2014) and HCC (Fan et al. 2016), whereas inverse trends have been reported for HNSCC (Warta et al. 2014) and ccRCC (Reustle et al. 2018). In agreement with these findings, we observed protective effects of ABCB1 expression on survival in ccRCC (logrank P = 1.4*10–6, HR 0.49, CI 0.36–0.66) and HNSCC (logrank P = 9.6*10–5, HR 0.59, CI 0.43–0.74; Table 1). Furthermore, inverse trends were observed for ovarian cancer (logrank P = 0.052, HR 1.32, CI 1.0–1.74) and HCC (logrank P = 0.002, HR 1.75, CI 1.22–2.52) that were however not significant after correction for multiple testing. Our results also corroborated (HCC: logrank P = 5.4*10–5, HR 2.01, CI 1.42–2.84; BRCA: logrank P = 2.2*10–5, HR 1.43, CI 1.21–1.68) previous observations that increased expression of the multidrug resistance transporter MRP1 associated with poor prognosis in HCC (Vander Borght et al. 2008) and BRCA patients undergoing chemotherapy (Filipits et al. 2005).
Besides these confirmations of known multidrug resistance transporters, multiple significant associations with ATP transporters were discovered that were not previously implicated in drug resistance (Table 1). Among the risk factors, high expression of ABCB8 (logrank P = 1.2*10–5, HR 1.99, CI 1.45–2.73) and ABCB9 (logrank P = 4.2*10–7, HR 2.14, CI 1.58–2.88) were strong predictors of poor prognosis in ccRCC, while ABCB6 correlated with reduced survival in HCC (logrank P = 9.5*10–7, HR 2.36, CI 1.66–3.36) and PRCC (logrank P = 2.8*10–5, HR 3.34, CI 1.84–6.06). Furthermore, expression of the orphan transporters ABCF3 and ABCF1 was increased with worse outcomes in HCC (logrank P = 4.4*10–5, HR 2.05, CI 1.44–2.92) and in BRCA patients undergoing endocrine therapy (logrank P = 9.6*10–7, HR 1.7, CI 1.37–2.11).
Inversely, expression levels of the peroxisomal fatty acid transporters ABCD2 (logrank P = 2.2*10–5, HR 0.56, CI 0.43–0.74) and ABCD3 (logrank P = 1.4*10–7, HR 0.45, CI 0.33–0.61), as well as the mitochondrial transporters ABCB7 (logrank P = 6.4*10–10, HR 0.39, CI 0.29–0.54) and ABCB10 (logrank P = 1.1*10–6, HR 0.48, CI 0.36–0.65) were associated with significantly better outcomes in ccRCC and HNSCC. Further protective associations included the expression of the ABCG subfamily member ABCG1 (logrank P = 5.4*10–6, HR 0.5, CI 0.37–0.68), ABCG2 (logrank P = 1.8*10–12, HR 0.35, CI 0.26–0.48) and ABCG5 (logrank P = 2.6*10–5, HR 0.48, CI 0.34–0.68) in ccRCC and HCC, as well as correlations of CFTR levels with improved outcomes in lung adenocarcinoma (logrank P = 3*10–5, HR 0.54 CI 0.41–0.73).
Validation of selected candidate associations in independent cohorts
To further increase the confidence in the reported associations, we conducted non-parametric survival analysis based on the Kaplan–Meier estimator and aimed for validation of selected associations in independent cohorts. Specifically, we focused on the associations in ovarian cancer and lung adenocarcinoma as the two cancer types for which we had access to sufficiently large validation cohorts. For ovarian cancer, we found a borderline significant association between ABCC12 expression and overall survival for grade 3 tumors (logrank P = 0.048; HR, 1.36; CI 1 to 1.85); however, this association was lost when all cancer grades were considered (logrank P = 0.16; Supplementary Fig. 1).
In contrast, the association of increased CFTR expression with improved outcomes in lung adenocarcinoma was confirmed in two independent cohorts (Fig. 2). First, we validated the finding in 246 patients with a history of smoking and found a highly significant association with an almost identical hazard ratio compared to the TCGA RNA-Seq data (logrank P = 0.0021; HR, 0.49; CI 0.3 to 0.78 vs. HR, 0.54; CI, 0.41 to 0.73 for TCGA). Furthermore, we observed a further significant correlation of almost identical magnitude in an additional cohort of 143 never-smokers (logrank P = 0.0023; HR, 0.31; CI 0.14 to 0.68).
Pharmacological stimulation of CFTR function reduces lung adenocarcinoma cell proliferation
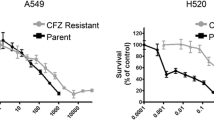
The clinical association of CFTR expression with lung cancer patient prognosis was further investigated in vitro. Notably, because the most commonly used and highly proliferative lung adenocarcinoma cell line A549 does not express CFTR (Hamai et al. 2009), we used Calu-3 cells, which exhibit natural CFTR expression and thus do not require CFTR overexpression, as in previous studies (Hamai et al. 2009; Qian et al. 2021). To monitor proliferation dynamics, we performed time-lapse imaging and found that Calu-3 cells proliferated with a growth rate (r%) of 27–42% per 24 h, resulting in a doubling time (Td) of ∼51 h (Fig. 3a–b).
CFTR activation reduces the proliferation of lung adenocarcinoma cells in vitro. a Time-lapse brightfield images of Calu-3 cells at selected time points throughout the experimental timeframe of 80 h. Images show the same representative field of view. b The relative confluency of Calu-3 cells was determined automatically every 4 h using in three independent samples using nine fields of view each. Note, that cell proliferation in the studied time frame is quasi-linear with a coefficient of determination (R2) of 0.92. Cellular growth rates (r%) are indicated for three intervals (0–24 h, 24–48 h and 48–72 h), resulting in an overall doubling time (Td) of 51 h. c Bar plot showing the reduction in lung adenocarcinoma cell confluency after 80 h upon treatment with ivacaftor compared to DMSO control. Expression levels of CFTR mRNA d and CFTR protein e upon siRNA-mediated knock-down. f Lung adenocarcinoma cell confluency after 80 h upon treatment with ivacaftor in CFTR knock-down cells. g Proliferation curves of control and CFTR knock-down cells upon treatment with vehicle (DMSO), 1 and 5 µM ivacaftor. Note the dose-dependent decrease in growth rates. h Quantification of cellular doubling times. Ivacaftor dose-dependently increases doubling times in both control and CFTR knock-down cells; however, the magnitude of this effect is significantly higher in the latter. i Therapeutic concentrations of doxorubicin (10 nM) and ivacaftor (1 µM) show additive effects in reducing cell numbers. Error bars indicate SEM. * and ** indicate P < 0.05 and P < 0.01, respectively. n.s. not significant (P > 0.05). IVA ivacaftor, DOX doxorubicin; KD CFTR knock-down
Next, we assessed whether CFTR activation impacted cell proliferation. To this end, we exposed cells to clinically relevant concentrations of the CFTR potentiator ivacaftor (1–5 µM; therapeutic cmax∼2–3 µM dose) (https://www.ema.europa.eu/en/documents/product-information/kalydeco-epar-product-information_en.pdf; https://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/203188Orig1s000ClinPharmR.pdf). Notably, we observed a significant dose-dependent inhibition of proliferation by 8 and 17% in cells exposed for three days to 1 µM and 5 µM ivacaftor, respectively (P = 0.023; Fig. 3c). To test whether effects of CFTR activation differ with CFTR expression, we used knock-downs using antisense oligos. Transfection with anti-CFTR siRNA reduced RNA and protein levels by 72 and 40%, respectively (Fig. 3d–3; Supplementary Fig. 2). Importantly, in cells in which CFTR expression was reduced, the effects of CFTR potentiation were even stronger with proliferation being reduced by up 29% after three days of exposure (Fig. 3f). These endpoint results align with dynamic proliferation measurements showing that daily growth rates in controls were decreased by 7%, corresponding to increases in cell doubling times from 51.8–54.9 h, while growth rates of CFTR knock-down cells were increased by 14%, resulting in doubling times of 59.4 h (Fig. 3g–h).
We furthermore tested whether the cytostatic effects of ivacaftor were synergistic with conventional cytotoxic chemotherapeutics, such as anthracyclines. Notably, when ivacaftor or doxorubicin were given alone at therapeutic concentrations (doxorubicin, 10 nM) (Bramwell et al. 2002), both drugs equally reduced cell numbers after 3 days of exposure (Fig. 3i). However, when both drugs were combined significant additive effects were observed in both control and CFTR knock-down cells, suggesting that CFTR potentiation might be a promising strategy for adjuvant therapy irrespective of tumor CFTR expression levels.
Discussion
Cancer gene expression patterns have been established as tools to classify tumor subgroups and derive patient prognoses (Qian et al. 2021). However, except for the FDA-approved Oncotype DX and MammaPrint tests that constitute integral parts of routine clinical care to guide decision-making regarding the use of adjuvant chemotherapy in early breast cancer (van ’t Veer et al. 2002; Paik et al. 2004; Cardoso, et al. 2016), other cancer expression signatures remain, as of to date, not actionable. Besides actionability, tumor signatures can also reveal mechanisms underlying disease biology, thereby potentially informing drug development and future therapeutic strategies. However, statistical association between gene expression patterns and cancer outcomes cannot be directly used to infer disease-relevant mechanisms without careful validation and/or experimental support (Venet et al. 2011).
To increase the likelihood of finding mechanistically meaningful associations, we here focused on the ABC transporter gene family due to their known roles in chemotherapy resistance. Importantly, while poor prognosis is conventionally associated with the overexpression of ABC transporters, we find that of the 29 significant associations between expression and survival, only 16 (55%), mostly with members of the ABCA, ABCB and ABCC subfamilies, indicate that increased expression is associated with worse outcomes. By contrast, increased expression of ABCD and ABCG genes was overall associated with improved survival. Notably, the cancer types for which the most significant changes in ABC expression signatures were detected (ccRCC and HCC), originate from cell types with a rich transporter expression portfolio and major roles in the disposition of endogenous and xenobiotic compounds. As such, associations between reduced transporter expression and poor prognosis might be due to increasing tumor dedifferentiation, possibly downstream of constitutive ERK-NRF2 signaling (Vecchio et al. 2014).
In previous studies, ABC expression was shown to be a strong predictor of chemotherapy resistance in acute myeloid leukemia (Marzac et al. 2011; Steinbach et al. 2006) and acute lymphoblastic leukemia patients (Efferth et al. 2006). However, links between ABC expression and survival in solid tumors are less established and only few such associations have received experimental support. The association between reduced CFTR expression and outcomes in patients with lung adenocarcinoma was among the most significant in our data. CFTR encodes a cAMP-activated chloride channel that plays essential roles in ion and water fluxes across epithelial tissues. Homozygous or compound heterozygous reduced function variants in CFTR are the known cause of cystic fibrosis and somatic CFTR mutations are enriched in non-small cell lung cancer (Govindan et al. 2012). Hypermethylation of CFTR resulting in transcriptional deactivation constitutes a common hallmark of NSCLC (Son et al. 2011) and reduced CFTR expression is significantly correlated with advanced disease stage and lymph node metastasis (Li et al. 2015). While these combined genetic and epigenetic findings strongly indicate that CFTR expression levels constitute a strong biomarker for lung cancer outcomes, they do not provide information about whether suppression of CFTR is a consequence of cellular transformation or might act as an upstream driver. Furthermore, these studies did not evaluate whether CFTR might constitute a putative therapeutic target.
We thus conducted in vitro experiments using the CFTR potentiator ivacaftor (Goor et al. 2009). Notably, while ivacaftor is only approved for the treatment of cystic fibrosis patients with specific genetic variations, multiple studies have consistently demonstrated that it also activates the unaltered reference transporter present in the utilized cell line (Eckford et al. 2012; Jih and Hwang 2013; Kim et al. 2018). Our results demonstrate that ivacaftor significantly reduced the proliferation of lung adenocarcinoma cells, corroborating that CFTR activity is mechanistically involved in cancer pathogenesis and acts as a pharmacologically targetable tumor suppressor. Effects of ivacaftor were further amplified upon CFTR knock-downs to levels found in heterozygous cystic fibrosis risk allele carriers (knock-downs resulted in 40% reduced protein levels while heterozygous carriers of the most common cystic fibrosis variant p.Phe508del have around 50% lower CFTR levels at the plasma membrane). Additionally, these findings are consistent with previous reports showing that knock-down of CFTR increased malignancy in a mouse xenograft model (Li et al. 2015). Similarly, in vitro exposure of lung cancer cells to nicotine resulted in reduced CFTR expression and increased cell migration, thus providing a potential link between smoking and disease aggressiveness (Li et al. 2018). However, the finding that low CFTR expression associated with worse clinical outcomes also in never-smokers suggests that potential nicotine-mediated downregulation of CFTR does not constitute the only mechanism underlying reduced CFTR expression.
In vitro studies in recombinant expression systems indicate that expression of functional CFTR suppresses NFκB activity (Vij et al. 2009), which in turn constitutes a key mediator controlling epithelial-to-mesenchymal transition (Ma et al. 2021). While the molecular links between CFTR activity and NFκB signaling remain elusive, the inhibition of NFκB activation is likely caused by defective CFTR Cl− channel activity rather than protein misfolding, as the expression of different defective CFTR channels results in increased NFκB signaling, irrespective of whether the defect is associated with trafficking or channel function (Weber et al. 2001; Dudez et al. 2008).
Our finding that CFTR is directly involved in lung adenocarcinoma progression receives further support from a recent large Danish register study in which morbidity and mortality of 108,035 individuals genotyped for the CFTR reduced function variant p.Phe508del was analyzed during up to 15 years of follow-up (Çolak et al. 2020). Strikingly, the authors found that while heterozygous variant carriers did not have reduced lifespan, they had a 52% higher lung cancer risk, thus strongly suggesting that reduced CFTR expression constitutes not only a biomarker for lung cancer prognosis but is also directly involved in disease etiology. Furthermore, a meta-analysis of 1159 NSCLC patients analyzing the association between NFκB expression and overall survival found that NFκB levels constitute a prognostic marker for poor outcomes (Gu et al. 2018), providing further in vivo evidence for the important role of the CFTR- NFκB axis.
In conclusion, our data provide the first comprehensive pan-cancer overview of somatic ABC transporter dysregulation and reveal gene- and cancer type-specific signatures that correlate with patient outcomes. Among those, we validate the association between CFTR expression and lung adenocarcinoma in two independent cohorts and demonstrate experimentally that pharmacological stimulation of CFTR function at therapeutically relevant concentrations results in a dose-dependent inhibition of lung cancer cell proliferation. In the context of previous results, these data indicate that CFTR is directly involved in lung cancer onset and progression and that CFTR thus constitutes a promising target for adjuvant therapy by repurposing already approved CFTR agonists.
Availability of data and materials
All analyzed data are available at The Cancer Genome Atlas Program (TCGA) repository, the Cancer Biomedical Informatics Grid and the Gene Expression Omnibus.
References
Bramwell VH, Morris D, Scott Ernst D, Hings I, Blackstein M, Venner PM, Ette EI, Harding MW, Waxman A, Demetri GD (2002) Safety and efficacy of the multidrug-resistance inhibitor biricodar (VX-710) with concurrent doxorubicin in patients with anthracycline-resistant advanced soft tissue sarcoma. Clin Cancer Res 8:383–393
Cardoso F, van’t Veer LJ, Bogaerts J, Slaets L, Viale G, Delaloge S, et al 2016 70-Gene Signature as an Aid to Treatment Decisions in Early-Stage Breast Cancer. N Engl J Med 375 717–729.
Çolak Y, Nordestgaard BG, Afzal S (2020) Morbidity and mortality in carriers of the cystic fibrosis mutation CFTR Phe508del in the general population. Eur Respir J 56:2000558
de Oliveira J, Felipe AV, Neto RA, Oshima CT, de Souza SM, Forones NM (2014) Association between ABCB1 immunohistochemical expression and overall survival in gastric cancer patients. Asian Pac J Cancer Prev 15:6935–6938
Del Vecchio CA, Feng Y, Sokol ES, Tillman EJ, Sanduja S, Reinhardt F, Gupta PB (2014) De-differentiation confers multidrug resistance via noncanonical perk-nrf2 signaling. PloS Biol 12:e1001945
Dudez T, Borot F, Huang S, Kwak BR, Bacchetta M, Ollero M, Stanton BA, Chanson M (2008) CFTR in a lipid raft-TNFR1 complex modulates gap junctional intercellular communication and IL-8 secretion. Biochim Biophys Acta 1783(5):779–788
Eckford PD, Li C, Ramjeesingh M, Bear CE (2012) Cystic fibrosis transmembrane conductance regulator (CFTR) potentiator VX-770 (ivacaftor) opens the defective channel gate of mutant CFTR in a phosphorylation-dependent but ATP-independent manner. J Biol Chem 287:36639–36649
Efferth T, Gillet JP, Sauerbrey A, Zintl F, Bertholet V, de Longueville F et al (2006) Expression profiling of ATP-binding cassette transporters in childhood T-cell acute lymphoblastic leukemia. Mol Cancer Ther 5:1986–1994
Fan L, Zhang Y, Zhou Y, Wang Z, Zhang Y, Chen H (2016) Clinical significance of ABC transporter expression in patients with hepatocellular carcinoma. J Hard Tissue Biol 25:81–88
Filipits M, Pohl G, Rudas M, Dietze O, Lax S, Grill R et al (2005) Clinical role of multidrug resistance protein 1 expression in chemotherapy resistance in early-stage breast cancer: the Austrian Breast and Colorectal Cancer Study Group. J Clin Oncol 23:1161–1168
Fletcher JI, Haber M, Henderson MJ, Norris MD (2010) ABC transporters in cancer: more than just drug efflux pumps. Nat Rev Cancer 10:147–156
Govindan R, Ding L, Griffith M, Subramanian J, Dees ND, Kanchi KL et al (2012) Genomic landscape of non-small cell lung cancer in smokers and never-smokers. Cell 150:1121–1134
Gu L, Wang Z, Zuo J, Li H, Zha L (2018) Prognostic significance of NF-κB expression in non-small cell lung cancer: a meta-analysis. PLoS ONE 13(5):e0198223
Győrffy B (2021) Survival analysis across the entire transcriptome identifies biomarkers with the highest prognostic power in breast cancer. Comput Struct Biotechnol J 19:4101–4109
Győrffy B, Lánczky A, Szállási Z (2012) Implementing an online tool for genome-wide validation of survival-associated biomarkers in ovarian-cancer using microarray data from 1287 patients. Endocr-Relat Cancer 19:197–208
Győrffy B, Surowiak P, Budczies J, Lánczky A (2013) Online survival analysis software to assess the prognostic value of biomarkers using transcriptomic data in non-small-cell lung cancer. PLoS ONE 8:e82241
Hamai H, Keyserman F, Quittell LM, Worgall TS (2009) Defective CFTR increases synthesis and mass of sphingolipids that modulate membrane composition and lipid signaling. J Lipid Res 50:1101–1108
Jih K, Hwang T (2013) Vx-770 potentiates CFTR function by promoting decoupling between the gating cycle and ATP hydrolysis cycle. Proc Natl Acad Sci USA 110:4404–4409
Johnatty SE, Beesley J, Gao B, Chen X, Lu Y, Law MH et al (2013) ABCB1 (MDR1) polymorphisms and ovarian cancer progression and survival: a comprehensive analysis from the ovarian cancer association consortium and the cancer genome atlas. Gynecol Oncol 131:8–14
Kim J, Farahmand M, Dunn C, Milla CE, Horii RI, Thomas EA et al (2018) Sweat rate analysis of ivacaftor potentiation of CFTR in non-CF adults. Sci Rep 1:16233
Li J, Zhang JT, Jiang X, Shi X, Shen J, Feng F et al (2015) The cystic fibrosis transmembrane conductance regulator as a biomarker in non-small cell lung cancer. Int J Oncol 46:2107–2115
Li H, Ma N, Wang J, Wang Y, Yuan C, Wu J et al (2018) Nicotine induces progressive properties of lung adenocarcinoma A549 cells by inhibiting cystic fibrosis transmembrane conductance regulator (CFTR) expression and plasma membrane localization. Technol Cancer Res Treat 17:1533033818809984
Liu J, Lichtenberg T, Poisson LM, Lazar AJ, Cherniack AD, Benz CC et al (2018) An integrated TCGA pan-cancer clinical data resource to drive high-quality survival outcome analytics. Cell 173:400–416
Ma M, Shi F, Zhai R, Wang H, Li K, Xu C, Yao W, Zhou F (2021) TGF-β promote epithelial-mesenchymal transition via NF-κB/NOX4/ROS signal pathway in lung cancer cells. Mol Biol Rep 48(3):2365–2375
Marzac C, Garrido E, Tang R, Fava F, Hirsch P, Benedictis CD et al (2011) ATP binding cassette transporters associated with chemoresistance: transcriptional profiling in extreme cohorts and their prognostic impact in a cohort of 281 acute myeloid leukemia patients. Haematologica 96:1293–1301
Nagy A, Munkácsy G, Győrffy B (2021) Pancancer survival analysis of cancer hallmark genes. Sci Rep 11:6047
Noguchi K, Katayama K, Sugimoto Y (2014) Human ABC transporter ABCG2/BCRP expression in chemoresistance: basic and clinical perspectives for molecular cancer therapeutics. Pharmacogenomics Pers Med 7:53–64
Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M et al (2004) A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 351:2817–2826
Pasello M, Giudice AM, Scotlandi K (2019) The ABC subfamily a transporters: multifaceted players with incipient potentialities in cancer. Semin Cancer Biol 60:57–71
Qian Y, Daza J, Itzel T, Betge J, Zhan T, Marmé F, Teufel A (2021) Prognostic cancer gene expression signatures: current status and challenges. Cells 10:648
Reustle A, Fisel P, Renner O, Büttner F, Winter S, Rausch S et al (2018) Characterization of the breast cancer resistance protein (BCRP/ ABCG2) in clear cell renal cell carcinoma. Int J Cancer 143:3181–3193
Son JW, Kim YJ, Cho HM, Lee SY, Lee SM, Kang J et al (2011) Promoter hypermethylation of the CFTR gene and clinical/pathological features associated with non-small cell lung cancer. Respirology 16:1203–1209
Sone K, Oguri T, Uemura T, Takeuchi A, Fukuda S, Takakuwa O et al (2019) Genetic variation in the ATP binding cassette transporter ABCC10 is associated with neutropenia for docetaxel in Japanese lung cancer patients cohort. BMC Cancer 19:246
Steinbach D, Gillet JP, Sauerbrey A, Gruhn B, Dawczynski K, Bertholet V et al (2006) ABCA3 as a possible cause of drug resistance in childhood acute myeloid leukemia. Clin Cancer Res 12:4357–4363
Sun S, Cai J, Yang Q, Zhu Y, Zhao S, Wang Z (2016) Prognostic value and implication for chemotherapy treatment of ABCB1 in epithelial ovarian cancer: a meta-analysis. PLoS ONE 11:e0166058
Theile D, Wizgall P (2021) Acquired ABC-transporter overexpression in cancer cells: transcriptional induction or Darwinian selection? Naunyn-Schmiedeberg’s Arch Pharmacol 394:1621–1632
van ’t Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AA, Mao M, et al. 2002 van ’t Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AA, Mao M, et al. 2002 Gene expression profiling predicts clinical outcome of breast cancer. Nature 415 530–536
Van Goor F, Hadida S, Grootenhuis PD, Burton B, Cao D, Neuberger T et al (2009) Rescue of CF airway epithelial cell function in vitro by a CFTR potentiator, VX-770. Proc Natl Acad Sci USA 106:18825–18830
Vander Borght S, Komuta M, Libbrecht L, Katoonizadeh A, Aerts R, Dymarkowski S et al (2008) Expression of multidrug resistance-associated protein 1 in hepatocellular carcinoma is associated with a more aggressive tumour phenotype and may reflect a progenitor cell origin. Liver Int 28:1370–1380
Venet D, Dumont JE, Detours V (2011) Most random gene expression signatures are significantly associated with breast cancer outcome. PloS Comput Biol 7:e1002240
Vij N, Mazur S, Zeitlin PL (2009) CFTR is a negative regulator of NFkappaB mediated innate immune response. PLoS ONE 4(2):e4664
Warta R, Theile D, Mogler C, Herpel E, Grabe N, Lahrmann B et al (2014) Association of drug transporter expression with mortality and progression-free survival in stage iv head and neck squamous cell carcinoma. PLoS ONE 9:e108908
Weber AJ, Soong G, Bryan R, Saba S, Prince A (2001) Activation of NF-kappaB in airway epithelial cells is dependent on CFTR trafficking and Cl- channel function. Am J Physiol Lung Cell Mol Physiol 281(1):L71–L78
Xiao Q, Zhou Y, Lauschke VM (2020) Impact of variants in ATP-binding cassette transporters on breast cancer treatment. Pharmacogenomics 21:1299–1310
Xiao H, Zheng Y, Ma L, Tian L, Sun Q (2021) Clinically-Relevant ABC Transporter for Anti-Cancer Drug Resistance. Front Pharmacol 12:648407
Acknowledgements
We are grateful to Hanna Axelsson (Department of Medical Biochemistry and Biophysics at Karolinska Institutet) for kindly providing the Calu-3 cells.
Funding
Open access funding provided by Karolinska Institute. The authors received support from the European Union’s Horizon 2020 research and innovation program U-PGx (grant agreement number 668353), from the Swedish Research Council (grant agreement numbers: 2016–01153, 2016–01154 and 2019–01837), from the EU/EFPIA/OICR/McGill/KTH/Diamond Innovative Medicines Initiative 2 Joint Undertaking (EUbOPEN grant number 875510), as well as from the Swedish Strategic Research Programmes in Diabetes (SFO Diabetes) and Stem Cells and Regenerative Medicine (SFO StratRegen). The lab furthermore acknowledges support from the Robert Bosch Foundation for Medical Research (RBMF), Merck KGaA and Eli Lilly and Company. S.K. is a recipient of an Onassis Foundation scholarship.
Author information
Authors and Affiliations
Contributions
QX performed the computational analyses of ABC expression signature data and compiled the first draft of the manuscript. SK performed in vitro experiments and revised the draft. DCS supported the in vitro work. VML. designed and supervised the research and revised the draft. All authors approve the submitted version.
Corresponding author
Ethics declarations
Conflict of interest
V.M.L. declares no conflict of interest according to the ICMJE Uniform Requirements but discloses the following financial relationships: CEO and shareholder of HepaPredict AB; co-founder and chairman of the board PersoMedix AB; consultancy work for Enginzyme AB. The other authors declare no competing interests.
Ethical approval
The analyzed data is available for aggregate, deidentified analysis and, thus, IRB approval specific to this study was not required.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
432_2022_4106_MOESM1_ESM.pdf
Supplementary file1 Supplementary Figure 1: Association of ABCC12 with overall survival of ovarian cancer patients. Kaplan-Meier plots of patient survival stratified by ABCC12 expression in the TCGA discovery cohort (a; n=373 patients), as well as in the GeneChip validation cohort (b, c). Note that a borderline significant association was found with stage 3 ovarian cancer (b; n=392 patients), whereas this correlation was lost when all patients were considered (c; n=655 patients). (PDF 554 kb)
432_2022_4106_MOESM2_ESM.pdf
Supplementary file2 Supplementary Figure 2: Western blot of CFTR knock-down experiments. Western blot membranes are shown that were probed for CFTR and β-actin. The quantification of these bands are shown in Figure 3e. (PDF 3441 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xiao, Q., Koutsilieri, S., Sismanoglou, DC. et al. CFTR reduces the proliferation of lung adenocarcinoma and is a strong predictor of survival in both smokers and non-smokers. J Cancer Res Clin Oncol 148, 3293–3302 (2022). https://doi.org/10.1007/s00432-022-04106-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04106-x