Abstract
Purpose
In patients undergoing allogeneic stem cell transplantation, conditioning regimens containing alemtuzumab instead of anti-thymocyte globulin (ATG) may result in an earlier platelet engraftment and a reduced number of platelet transfusions.
Methods
We performed a retrospective, single-center, case–control study analyzing time to engraftment and transfusion needs using alemtuzumab in comparison with ATG as part of conditioning protocol.
Results
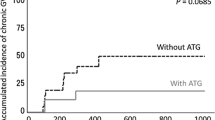
Median values for time to platelet engraftment, number of transfused platelet concentrates and number of transfused red cell concentrates were 12 versus 19.5 days (p < 0.001), 2 versus 14 (p < 0.001) and 6 versus 14.5 (p = 0.003) in the alemtuzumab and ATG group. Time to leukocyte engraftment did not differ with median 15 days in both groups. Patients in the ATG group showed a significant higher decrease in platelet count during conditioning (68 vs. 29 %, p = 0.001), leading to significant lower median platelet counts at the day of stem cell infusion (38 vs. 95.5 Gpt/l, p = 0.008), and higher values for median C-reactive protein after first antibody infusion (69.0 vs. 43.6 mg/l, p = 0.001) compared with alemtuzumab group. Test for significance was done by using Wilcoxon rank-sum test. Subgroup analysis considering the type of ATG used (Thymoglobulin vs. ATG Fresenius) revealed that differences between alemtuzumab and ATG group were more due to effects of ATG Fresenius than Thymoglobulin.
Conclusions
The use of alemtuzumab in comparison with ATG as part of the conditioning regimen may be an approach to reduce the number of transfused platelet and red cell concentrates after allogeneic stem cell transplantation.
Similar content being viewed by others
References
Avivi I, Chakrabarti S, Milligan DW et al (2004) Incidence and outcome of adenovirus disease in transplant recipients after reduced-intensity conditioning with alemtuzumab. Biol Blood Marrow Transpl 2004(10):186–194
Bertz H, Spyridonidis A, Wäsch R, Grüllich C, Egger M, Finke J (2009) A novel GVHD-prophylaxis with low-dose alemtuzumab in allogeneic sibling or unrelated donor hematopoetic cell transplantation: the feasibility of deescalation. Biol Blood Marrow Transpl 2009(15):1563–1570
Busemann C, Neumann T, Schulze M et al (2013) Low-dose alemtuzumab vs. standard policy for prevention of graft-versus-host disease in unrelated and related allogeneic stem cell transplantation-a matched pair analysis. Ann Hematol 2013(92):945–952
Chakrabarti S, Mackinnon S, Chopra R et al (2002) High incidence of cytomegalovirus infection after nonmyeloablative stem cell transplantation: potential role of Campath-1H in delaying immune reconstitution. Blood 2002(99):4357–4363
Chakraverty R, Orti G, Roughton M et al (2010) Impact of in vivo alemtuzumab dose before reduced intensity conditioning and HLA-identical sibling stem cell transplantation: pharmacokinetics, GVHD, and immune reconstitution. Blood 2010(116):3080–3088
Cumpelik A, Gerossier E, Jin J et al (2015) Mechanism of platelet activation and hypercoagulability by antithymocyte globulins (ATG). Am J Transpl 2015(15):2588–2601
Delgado J, Pillai S, Benjamin R et al (2008) The effect of in vivo T cell depletion with alemtuzumab on reduced-intensity allogeneic hematopoietic cell transplantation for chronic lymphocytic leukemia. Biol Blood Marrow Transpl 2008(14):1288–1297
Deutsch VR, Nagler A, Slavin S, Condiotti R, Levine RF, Eldor A (1993) Effect of bone marrow T lymphocytes treated with CAMPATH 1G on megakaryocyte colony formation. Exp Hematol 1993(21):1427–1435
Finke J, Bethge WA, Schmoor C et al (2009) Standard graft-versus-host disease prophylaxis with or without anti-T-cell globulin in haematopoietic cell transplantation from matched unrelated donors: a randomised, open-label, multicentre phase 3 trial. Lancet Oncol 2009(10):855–864
Hale G, Zhang MJ, Bunjes D et al (1998) Improving the outcome of bone marrow transplantation by using CD52 monoclonal antibodies to prevent graft-versus-host disease and graft rejection. Blood 1998(92):4581–4590
Juliusson G, Theorin N, Karlsson K, Frödin U, Malm C (2006) Subcutaneous alemtuzumab vs ATG in adjusted conditioning for allogeneic transplantation: influence of Campath dose on lymphoid recovery, mixed chimerism and survival. Bone Marrow Transpl 2006(37):503–510
Kottaridis PD, Milligan DW, Chopra R et al (2000) In vivo CAMPATH-1H prevents graft-versus-host disease following nonmyeloablative stem cell transplantation. Blood 2000(96):2419–2425
Kröger N, Shaw B, Iacobelli S et al (2005) Comparison between antithymocyte globulin and alemtuzumab and the possible impact of KIR-ligand mismatch after dose-reduced conditioning and unrelated stem cell transplantation in patients with multiple myeloma. Br J Haematol 2005(129):631–643
Lekas N, Rosenberg JC (1976) Release, aggregation and lysis of human platelets by antilymphocyte globulin and antiplatelet serum. Thromb Haemost 1976(36):411–423
Myers GD, Krance RA, Weiss H et al (2005) Adenovirus infection rates in pediatric recipients of alternate donor allogeneic bone marrow transplants receiving either antithymocyte globulin (ATG) or alemtuzumab (Campath). Bone Marrow Transpl 2005(36):1001–1008
Nagler A, Condiotti R, Lubina A, Deutsch VR (1997) Enhancement of megakaryocytopoiesis by Campath-1G-treated natural killer cells. Bone Marrow Transpl 1997(20):525–531
Norlin AC, Remberger M (2010) A comparison of Campath and Thymoglobulin as part of the conditioning before allogeneic hematopoietic stem cell transplantation. Eur J Haematol 2010(86):57–66
Park SH, Choi SM, Lee DG et al (2009) Infectious complications associated with alemtuzumab use for allogeneic hematopoietic stem cell transplantation: comparison with anti-thymocyte globulin. Transpl Infect Dis 2009(11):413–423
Peggs KS, Sureda A, Qian W et al (2007) Reduced-intensity conditioning for allogeneic haematopoietic stem cell transplantation in relapsed and refractory Hodgkin lymphoma: impact of alemtuzumab and donor lymphocyte infusions on long-term outcomes. Br J Haematol 2007(139):70–80
Penack O, Fischer L, Stroux A et al (2008) Serotherapy with thymoglobulin and alemtuzumab differentially influences frequency and function of natural killer cells after allogeneic stem cell transplantation. Bone Marrow Transpl 2008(41):377–383
Perez-Simon JA, Kottaridis PD, Martino R et al (2002) Nonmyeloablative transplantation with or without alemtuzumab: comparison between 2 prospective studies in patients with lymphoproliferative disorders. Blood 2002(100):3121–3127
Poiré X, van Besien K (2011) Alemtuzumab in allogeneic hematopoetic stem cell transplantation. Expert Opin Biol Ther 2011(11):1099–1111
Ramsay NK, Kersey JH, Robison LL et al (1982) A randomized study of the prevention of acute graft-versus-host disease. N Engl J Med 1982(306):392–397
Rosenberg JC, Lekas N, Lysz K, Morrell R (1975) Effect of antithymocyte globulin and other immune reactants on human platelets. Surgery 1975(77):520–529
Slichter SJ, Kaufman RM, Assmann SF et al (2010) Dose of prophylactic platelet transfusions and prevention of hemorrhage. N Engl J Med 2010(362):600–613
Soiffer RJ, LeRademacher J, Ho V et al (2011) Impact of immune modulation with anti–T-cell antibodies on the outcome of reduced-intensity allogeneic hematopoietic stem cell transplantation for hematologic malignancies. Blood 2011(117):6963–6970
Stanworth SJ, Estcourt LJ, Powter G et al (2013) A no-prophylaxis platelet-transfusion strategy for hematologic cancers. N Engl J Med 2013(368):1771–1780
Theurich S, Fischmann H, Shimabukuro-Vornhagen A et al (2012) Polyclonal anti-thymocyte globulins for the prophylaxis of graft-versus-host disease after allogeneic stem cell or bone marrow transplantation in adults. Cochrane Database Syst Rev 9:CD009159
Van Besien K, Kunavakkam R, Rondon G et al (2009) Fludarabine-melphalan conditioning for AML and MDS: alemtuzumab reduces acute and chronic GVHD without affecting long-term outcomes. Biol Blood Marrow Transpl 2009(15):610–617
Waldmann H, Hale G (2005) CAMPATH: from concept to clinic. Philos Trans R Soc Lond B Biol Sci 2005(360):1707–1711
Wandt H, Schaefer-Eckart K, Wendelin K et al (2012) Therapeutic platelet transfusion versus routine prophylactic transfusion in patients with haematological malignancies: an open-label, multicentre, randomised study. Lancet 2012(380):1309–1316
Weiden PL, Doney K, Storb R, Thomas ED (1978) Anti-human thymocyte globulin (ATG) for prophylaxis and treatment of graft-versus-host disease in recipients of allogeneic marrow grafts. Transpl Proc 1978(10):213–216
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. For this type of study, formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Neumann, T., Schneidewind, L., Thiele, T. et al. Reduced platelet transfusions and earlier platelet engraftment using alemtuzumab-based conditioning regimen in allogeneic stem cell transplantation. J Cancer Res Clin Oncol 142, 1091–1097 (2016). https://doi.org/10.1007/s00432-016-2114-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-016-2114-7