Abstract
The association between breastfeeding and the occurrence of allergic rhinitis (AR) and food allergy (FA) in offspring remains inconclusive. This review aims to comprehensively explore the potential relationships between various patterns and durations of breastfeeding and allergic diseases in offspring. We systematically searched PubMed, EMBASE, Cochrane, WOS databases, and Google Scholar for observational studies published up to March 30, 2023, that investigated the link between breastfeeding and allergies in offspring. The quality of the studies was assessed using the Newcastle-Ottawa Scale (NOS) and Joanna Briggs Institute (JBI). Pooled odds ratios (OR) and 95% confidence intervals (95% CI) were calculated employing an appropriate model based on the degree of heterogeneity. A total of 68 studies, encompassing 772,142 children, were ultimately included. The findings indicated that breastfeeding for more than 6 months was associated with a reduced risk of AR (OR = 0.88, 95% CI: 0.79 to 0.98) but posed a risk for FA (OR = 1.69, 95% CI: 1.27 to 2.25). Exclusive breastfeeding exhibited a protective effect against AR (OR = 0.94, 95% CI: 0.90 to 0.97), whereas non-breastfeeding was identified as a risk factor for AR (OR = 1.48; 95% CI: 1.03 to 2.12). No significant association was observed between breastfeeding patterns and FA.
Conclusion: Breastfeeding for more than 6 months proves to be an effective preventive measure against AR. However, large prospective high-quality studies are needed to investigate the potential risk of FA in children with prolonged breastfeeding.
What is Known: • The impact of breastfeeding on allergic rhinitis and food allergy in offspring is controversial. • Previous meta-analyses fail to prove the effect of breastfeeding on food allergy in offspring of all ages. | |
What is New: • Breastfeeding for more than 6 months proves to be an effective preventive measure against AR. However, it potentially elevates the risk of FA in children. Non-breastfeeding is linked to an increased risk of AR in children, but there is no evidence of an association between breastfeeding patterns and FA in children. • The impact of breastfeeding on allergic rhinitis and food allergy in offspring may vary with the time and pattern of breastfeeding. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Allergic diseases have become increasingly prevalent among children, including conditions such as allergic rhinitis (AR), atopic dermatitis, bronchial asthma, and food allergy (FA) [1,2,3,4]. These conditions significantly impact the quality of life and pose an economic burden on affected children and their families [5], with potential life-threatening implications [6]. Kilanowski et al. [7] proposed that the surge in allergic disease prevalence in recent decades cannot be solely attributed to genetic factors. Akagawa et al. [8] also suggested a potential link to hygienic conditions, delivery methods, antibiotic usage, and Western diet improvements. How to prevent and manage allergic diseases in children has become a critical global public health concern.
In newborns, maintaining life after exposure to the extrauterine environment poses a major challenge to the immune system. The World Health Organization (WHO) recommends exclusive breastfeeding for infants under 6 months. As the primary source of natural nutrition for infants, breast milk provides not only essential nutrients such as protein and vitamins to support normal growth and development [9] but also white blood cells, antibodies, and immunoregulation factors to enhance the infant’s immune system [10]. Moreover, breastfed infants are generally healthier than formula-fed infants, with a significantly reduced risk of multiple serious diseases [11,12,13,14]. However, there is still a lack of in-depth and comprehensive research on the direct relationship between breastfeeding, childhood immunity, and allergic diseases.
In recent years, the association between breastfeeding and allergic diseases in children has become a focal point of research. Previous evidence-based medicine research has indicated that breastfeeding can reduce the risk of AR in children under 5 years old, but no significant association has been observed with their FA [15]. However, the limited number of included studies and substantial heterogeneity have diminished the reliability of this result. In their recent study, Hoang et al. found that long-term exclusive breastfeeding did not exhibit a protective effect against AR in children, with the overall evidence quality being relatively low [16]. Despite recent original studies exploring the link between breastfeeding and the risk of AR and FA, no conclusive findings have been drawn. Lyons et al. predicted factors contributing to FA in children and adults in Europe, revealing that breastfeeding for > 6 months served as a protective factor against FA [17]. In contrast, Yuenyongviwat et al., who studied risk factors for atopic dermatitis and FA in children, identified breastfeeding for more than 6 months as a major contributor to FA [18]. Saad et al. highlighted in their study on clinical phenotypes and related factors of milk allergy that exclusive breastfeeding was a protective factor against FA [19]. Matsumoto conducted a cohort study on nationwide births in Japan, concluding that exclusive breastfeeding was a risk factor for FA [20]. Tong et al., in a cross-sectional study on the prevalence and related risk factors of AR in children aged 6–12 years, found that breastfeeding for more than 6 months had a protective effect against AR [21]. However, Schmitz et al., who studied the prevalence and risk factors of atopic diseases in children and adolescents in Germany, identified breastfeeding for more than 6 months as a risk factor for AR [22]. The study by Rosas-Salazar et al. indicated that exclusive breastfeeding had a protective effect against rhinitis [23]. In contrast, Ahmed et al. demonstrated that exclusive breastfeeding promoted the occurrence of AR by evaluating eczema, asthma, AR, and allergic status in children in seventh graders from Iqaluit [24]. Given the limited and uncertain association between breastfeeding and allergic diseases in offspring, this systematic review and meta-analysis aim to synthesize existing evidence on the epidemiological characteristics of the relationship between breastfeeding and allergic diseases in offspring to quantify this association.
Materials and methods
This report adheres to the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [25] and Meta-analysis of Observational Studies in Epidemiology (MOOSE) [26]. Additionally, the meta-analysis was registered in PROSPERO (CRD42023416223).
Search strategy
PubMed, Embase, Cochrane Library, Web of Science, and Google Scholar were comprehensively searched for English-language literature, from the inception of the databases to March 30, 2023. Our search employed a combination of subject terms and free-text terms, including key terms such as child, children, Breast Feeding, Breast Milk, Food Hypersensitivity, Allergic Rhinitis, among others. Table S1 provides detailed information on the search strategies. Additionally, we manually examined the reference lists of major studies and relevant review articles to identify any additional studies meeting our inclusion criteria.
Literature screening
Inclusion criteria
(1) Participants: Offspring (with no age restriction); (2) Exposure factors: breastfeeding, measurement bases: questionnaires, follow-up, outpatient records, etc.; (3) Study types: observational study, including cross-sectional study, cohort study, case–control study; (4) Outcomes: AR, FA, with diagnostic criteria including Score for Allergic Rhinitis (SFAR), the International Study of Asthma and Allergies in Childhood (ISAAC), skin prick test (SPT), questionnaires and physician diagnosis, allergen-specific serum IgE levels, open food challenge test, and other criteria. (5) The study reported relative risk (RR), odds ratio (OR), and their 95% confidence interval (CIs) related to the outcome, or the original data were available for calculation.
Exclusion criteria
(1) Review, case report, research plan, or conference paper; (2) Clinical trial, animal, or in vitro study; (3) Duplicate publications and studies with no available full texts; (4) The literature did not provide information regarding the outcome indicators.
Literature screening was independently conducted by two reviewers (YL D and CB Z) based on the aforementioned criteria. Any disagreements during the screening process were addressed through discussion or, if necessary, by consulting a third reviewer (S L).
Data extraction and quality assessment
Relevant data were independently extracted from each literature by two reviewers (YL D and CB Z). The extracted information included the first author, publication year, country, research type, basic information of subjects, exposure factors, setting of exposure level, outcome indicators, and adjusted confounding factors.
The quality of cohort studies and case-control studies was assessed by two independent reviewers using the Newcastle-Ottawa Scale (NOS) [27]. The evaluated aspects for cohort studies included the following eight domains: representativeness of the exposure cohort, selection of the non-exposure cohort, confirmation of exposure, certification that the results of concern did not exist at the beginning of the study, comparability of cohorts based on design or analysis, evaluation of outcomes, assessment of whether the duration of follow-up is sufficient to obtain outcomes, and adequacy of cohort follow-up. Similarly, the following eight domains were evaluated for case-control studies: adequacy of case definition, representativeness of cases, selection of controls, definition of controls, comparability of cases and controls based on design or analysis, determination of the extent of exposure, the shared method for determining cases and controls, and comparison of non-response rates in cases and controls. Each aspect, except for comparability, had a top score of 1, with comparability having a maximum score of 2. The studies were rated on a scale of 0–9. Therefore, a total score ≥ 6 points indicated high-quality research.
The risk of bias in cross-sectional studies was assessed using the Joanna Briggs Institute (JBI) critical appraisal checklist for analytical cross-sectional studies [28]. This tool consists of eight domains: sample inclusion, description of subjects and settings, valid and reliable measure of exposure, objective and standard measure of condition, identifying confounding factors, strategies to deal with confounding factors, valid and reliable measure of outcome, and appropriate statistical analysis. Each item can be answered by four response options: yes (1 score), no (0 score), unclear (0 score), or not applicable (0 score). Based on the items in the appraisal tool, the articles were categorized as high quality (80% score and above), moderate (60–80% score), and low quality (< 60% score).
Data integration and statistical analysis
The primary outcome of interest was the relationship between breastfeeding and AR, while the secondary outcome was the association between breastfeeding and FA.
All meta-analyses utilized a random-effects model to combine effect sizes and were statistically analyzed using Stata 15.0, with a P value < 0.05 considered statistically significant. Heterogeneity across studies was assessed using Cochran’s Q X2 test, I2 statistic, and TAU (or tau-squared statistic), subgroup analysis and regression analysis were performed based on breastfeeding durations (< 4 months, 4–6 months, ≥ 6 months) and breastfeeding patterns (exclusive breastfeeding, partial breastfeeding, and non-breastfeeding) to determine heterogeneity and its sources among studies. Sensitivity analysis was used to assess the robustness of the meta-analysis by combining the results of the remaining studies after excluding each one individually [29, 30]. A funnel plot was generated to evaluate the potential publication bias in the included studies. Statistical tests (Egger’s or Begg’s test) were utilized to test the publication bias (at least eight studies were required). In case of significant publication bias, the trim-and-fill method was adopted to explore the impact of publication bias on the results.
Results
Literature screening results and flow chart
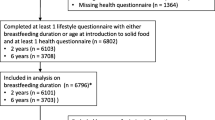
A total of 7,047 papers were initially identified through the database search, and no additional research was discovered through the examination of references. Following the removal of duplicate literature, 4850 articles underwent title and abstract review. Among these, 4357 articles were excluded as they did not meet the inclusion criteria, leaving 493 articles for a thorough full-text review. Ultimately, this meta-analysis incorporated 68 studies [17,18,19,20,21,22,23,24, 31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90]. The literature screening process is illustrated in Fig. 1.
Basic characteristics of included studies
The 68 included studies were conducted in 24 countries and regions, including China-Taiwan, China, Norway, Korea, Thailand, Turkey, Germany, Finland, Iran, Sweden, Canada, Japan, Netherlands, UK, America, Denmark, France, Egypt, Poland, Mexico, Kuwait, Spain, Australia, Qatar. In total, there were 35 articles on AR and 39 articles on FA. All studies were observational in nature, comprising cross-sectional studies (n = 30), cohort studies (n = 33), and case-control studies (n = 5). The participants across all publications were children, with a cumulative total of 772,142 children included in these studies. The sample size ranged from 65 to 46,616 in cohort studies, from 44 to 206,453 in cross-sectional studies, and from 126 to 422 in case-control studies. Most studies utilized the ISAAC questionnaires to assess allergic diseases, although other criteria such as skin prick tests, questionnaire surveys, and allergen-specific serum IgE levels were also employed to evaluate AR and FA. Additionally, potential confounding factors were adjusted in the majority of studies. The detailed characteristics of the included studies are illustrated in Table S2.
Quality evaluation
The quality assessment using the NOS scale revealed that the scores of 38 included studies were all ≥ 6, as detailed in Table S3. Concerning subject selection, 32 studies scored 4, while 6 studies scored 3, indicating potential bias in results due to specific selection of the control population. Regarding comparability, all 33 studies scored 2, signifying that important confounding factors, including age, were controlled in each study. For outcome evaluation, 23 studies scored 3, and 15 studies scored 2, due to inaccurate outcome definition, nonuse of internationally standardized methods, insufficient follow-up time, and incomplete follow-up information. Among the 30 cross-sectional studies, 16 were rated as high quality, and 14 were considered medium quality, as outlined in Table S4.
Meta-analysis results
Relationship between the duration of breastfeeding and allergic rhinitis in offspring
Twenty-two articles reported the relationship between the duration of breastfeeding and AR in offspring [21, 22, 31, 35,36,37, 42, 44, 51, 53, 56, 58,59,60, 63, 68, 70, 71, 77, 80, 83, 89]. The random effects model showed that there was no significant correlation between the duration of breastfeeding and AR in offspring (OR = 1.00, 95% CI:0.91 to 1.10, P = 0.995; τ2 = 0.0378, I2 = 91.0%, P < 0.001) (Fig. S1).
Relationship between the pattern of breastfeeding and allergic rhinitis in offspring
Sixteen articles investigated the relationship between breastfeeding patterns and AR in offspring [23, 24, 39, 50, 53, 56, 62, 64, 69, 72, 74, 75, 79,80,81, 90]. The random-effects model indicated no significant correlation between breastfeeding patterns and AR in offspring (OR = 1.06, 95% CI: 0.96 to 1.6, P = 0.238; τ2 = 0.0233, I2 = 89.5%, P < 0.001) (Fig. S2).
Relationship between the duration of breastfeeding and food allergy in offspring
Twenty-four articles reported the relationship between the duration of breastfeeding and FA in offspring [17, 18, 20, 33, 35, 36, 38, 40, 41, 45, 48, 49, 54, 55, 57, 61, 65,66,67, 73, 76, 82, 86, 87]. The random effects model showed that there was no significant correlation between the duration of breastfeeding and FA in offspring (OR = 1.37, 95% CI: 1.11 to 1.68, P = 0.004; τ2 = 0.1614, I2 = 78.9%, P < 0.001) (Fig. S3).
Relationship between the pattern of breastfeeding and food allergy in offspring
Twenty articles reported the relationship between the pattern of breastfeeding and FA in offspring [19, 20, 23, 24, 32, 34, 43, 45,46,47, 49, 50, 52, 55, 73, 78, 79, 84, 85, 88]. There was no significant correlation between the pattern of breastfeeding and FA in offspring (OR = 1.00, 95% CI: 0.85 to 1.19, P = 0.957; τ2 = 0.1071, I2 = 79.2%, P < 0.001) (Fig. S4).
Subgroup analysis and regression analysis
We performed a subgroup analysis for AR and FA based on the durations of breastfeeding (< 4 months, 4–6 months, ≥ 6 months) and breastfeeding patterns (exclusive breastfeeding, partial breastfeeding, and non-breastfeeding) to investigate the sources of heterogeneity (Figs. 2 and 3).
Association between different durations of breastfeeding and allergy in offspring
After conducting a subgroup analysis to assess the impact of different breastfeeding durations on AR, the results indicated a significant reduction in the risk of AR in offspring with breastfeeding for more than 6 months (OR = 0.88, 95% CI: 0.79 to 0.98; P = 0.015). However, there was no significant correlation observed between breastfeeding durations of < 4 months or 4–6 months and AR in offspring (OR = 1.10, 95% CI: 0.91 to 1.32; OR = 1.15, 95% CI: 0.93 to 1.43; respectively). Regression analysis demonstrated no significant difference in the impact of different breastfeeding durations on the extent of the correlation (P = 0.790).
Following the subgroup analysis of the influence of different breastfeeding durations on FA, the results revealed a significant increase in the risk of FA in offspring with breastfeeding for more than 6 months (OR = 1.75, 95% CI: 1.30 to 2.36). Conversely, there was no significant correlation found between breastfeeding durations of < 4 months or 4–6 months and FA in offspring (OR = 1.14, 95% CI: 0.90 to 1.44; OR = 0.83, 95% CI: 0.45 to 1.53; respectively). Additionally, regression analysis indicated no significant difference in the protective effect of different breastfeeding durations against FA in offspring (P = 0.126).
Relationship between different patterns of breastfeeding and allergy in offspring
After conducting a subgroup analysis to assess the influence of different patterns of breastfeeding on AR, the results indicated that non-breastfeeding was a risk factor for AR in offspring (OR = 1.48; 95% CI: 1.03 to 2.12), while exclusive breastfeeding had a protective effect against AR in offspring (OR = 0.94, 95% CI: 0.90 to 0.97). No significant correlation was observed between partial breastfeeding and AR in offspring (OR = 1.03; 95% CI: 0.84 to 1.27). Additionally, regression analysis revealed a significant difference in the protective effect of different patterns of breastfeeding against AR in offspring (P = 0.026), suggesting that the variation in breastfeeding patterns may contribute to heterogeneity.
Following the subgroup analysis of the influence of different patterns of breastfeeding on FA, the results indicated no significant correlation between non-breastfeeding, partial breastfeeding, or exclusive breastfeeding, and FA in offspring (OR = 1.53, 95% CI: 0.81 to 2.90; OR = 0.97, 95% CI: 0.74 to 1.26; OR = 0.86, 95% CI: 0.64 to 1.15; respectively). In regression analysis, there was no significant difference in the protective effect of different patterns of breastfeeding against FA in offspring (P = 0.324).
Sensitivity analysis
Sensitivity analyses were conducted separately for the influences of the duration and pattern of breastfeeding on AR and FA. The impact of each study on the summarized results was evaluated using a one-by-one exclusion method. The analysis results demonstrated that none of the pooled results were significantly affected by any individual study. This suggested that the results of this meta-analysis were relatively reliable (Fig. S5).
Publication bias
To ensure the validity of the meta-analysis results, we employed a funnel plot and conducted Egger’s and Begg’s tests to assess the publication bias for primary outcome indicators. The results indicated that there was no significant publication bias in the four outcome indicators (P > 0.05).
Discussion
Breast milk is explicitly acknowledged by the World Health Organization (WHO) as the preferred nourishment for newborns, even during public health crises [91]. It serves as a primary source of nutrition and energy for the early growth and development of infants. Global statistics indicate that enhancing the worldwide breastfeeding rate could potentially save the lives of over 820,000 children under 5 years old annually. However, this optimal feeding practice has not received adequate attention in high-income countries [9]. This may be attributed to their rapid socio-economic development, accelerated pace of life, and escalating pressures from family and work. For children, improved economic conditions provide the foundation for a better life, but the initial provision of adequate and scientifically sound nutrition is the cornerstone of lifelong health. This underscores the significance of prioritizing breastfeeding.
Our study findings underscore that breastfeeding for more than 6 months is effective in preventing AR, whereas non-breastfeeding increases the risk of AR in children. We observed a significant association between the duration of breastfeeding and FA in offspring. Prolonged breastfeeding (≥ 6 months), however, was linked to an increased risk of FA in children. Importantly, no evidence was found to suggest an association between the pattern of breastfeeding and FA in children.
Dr. Gabryszewski, in their study, reported a positive impact of breastfeeding in reducing the incidence of AR in children [92]. Our subgroup analysis results align with this, indicating that breastfeeding for more than 6 months protects against AR in offspring. This finding is consistent with the World Health Organization’s (WHO) recommendation of breastfeeding for at least 6 months [9]. Li et al. [93] discovered that in the comparison of children with house dust mite-induced allergic rhinitis (HDM-AR) and healthy controls, among children carrying the protective TT genotype of IL18R1_rs2287037, those exclusively breastfed for the first 4 months had a significantly reduced risk of rhinitis (OR = 0.33). This may offer insights into bioinformatics research on AR. On the contrary, non-breastfeeding emerged as a risk factor for AR in offspring. Studies have indicated that early respiratory tract infections under the age of 2 are closely linked to AR in children [94]. Various bioactive molecules in breast milk are effective in preventing early infections in children [10]. While this provides a plausible explanation for our results, further evidence is required to substantiate these findings due to the limited data in this subgroup.
FA in children is considered the “second epidemic wave” following asthma and AR [95]. Its prevalence is gradually increasing, with the severity of allergic reactions also on the rise [96]. Our results indicate that breastfeeding for over 6 months is a risk factor for FA in offspring. This finding can be explained by dietary diversity, which is defined as the variety of foods or food combinations consumed within a specific timeframe [97]. Changes in diet significantly impact intestinal microorganisms [98]. It has been shown that a diversified diet in infancy can increase butyrate, helping reduce the risk of allergies in children [99]. Butyrate promotes the extratymatic generation of Treg cells, maintains the intestinal barrier, and supports the development and function of the immune system [100,101,102]. Additionally, early introduction of allergic foods is considered as a primary method for preventing food allergies. Current guidelines [103] recommend regular and long-term complementary feeding for high-risk allergy children after systematic evaluation by physicians based on specific IgE levels and skin prick tests. This induces immune tolerance in the body. Prescott [104] highlighted the age of 4 to 6 months as a key period for establishing immune tolerance in early life. Reasonable introduction of complementary foods at this age is beneficial for preventing allergic diseases in infants. A 2016 randomized trial assessing the preventive effect of early introduction of six allergic foods (cow’s milk, hen’s egg, peanut, sesame, codfish, and heat) on FA demonstrated a 67% decrease in the relative risk of FA in children intaking allergic foods early [105].
This provides new ideas for us to explore why breastfeeding for more than 6 months increases the risk of FA. However, we believe it may be premature to draw conclusions based on the existing evidence. In addition to prolonged breastfeeding time, FA may also be caused by late introduction of solid food during this period. Hence, late introduction of solid food may play a pivotal role in the development of FA [106]. Recommendations released in 2022 also strongly recommend the introduction of potentially allergenic foods in infants at 6 months of age, without postponing or bringing exposure forward to reduce the risk of FA [107]. Therefore, if solid foods are not introduced when breastfeeding is prolonged, infants may lose a crucial window of opportunity to develop tolerance to potential allergens. Allergic diseases in children are undeniably complex, diverse, and multifaceted. Our study faced inevitable high heterogeneity in our statistics, particularly among children who received breastfeeding for 6–12 months. Given the differences in the duration of feeding and the limited number of studies in subgroups, further subdivision is difficult. Therefore, this seemingly contradictory statistical result still requires more supportive data. Additionally, we did not explore national differences in published studies, and individual factors such as the child’s gender, age, and geographical location might contribute to high heterogeneity in statistical results.
Strengths and limitations
Our research can be considered as an update to previous evidence. First, we included more recent literature on breastfeeding and the risk of AR and FA, and most included studies are considered of high quality. Still, the reliability of data was reduced in a few studies due to inaccurate definitions of outcomes and a lack of follow-ups. Second, since these studies are observational, all participants are unlikely to be interfered with by investigators. During the breastfeeding period described, if allergic symptoms or early signs were observed in children, parents might briefly stop breastfeeding and choose corresponding drug interventions, which could cause discontinuity of exposure factors and result in biased results. Additionally, due to the high proportion of retrospective studies included and the variations in the number and types of adjustment factors, it may be inevitable to avoid the influence of recall bias and other negative factors. A more rigorous assessment is required to eliminate these influences, such as the establishment of uniform diagnostic criteria for allergic diseases, and acquisition of more detailed records and reports to balance the feeding dose of breast milk. Finally, we did not explore the relationship between breastfeeding for more than 12 months and allergy in offspring due to insufficient data. Despite these shortcomings, the likelihood of publication bias in our study is low, suggesting that our summarized evidence is reliable overall.
Conclusion
This meta-analysis reveals that non-breastfeeding increases the risk of AR in children, whereas breastfeeding for more than 6 months effectively prevents AR, aligning with the regimen recommended by WHO. Regarding FA, there is no evidence to suggest an association between the pattern of breastfeeding and FA in children. However, there is a significant correlation between the duration of breastfeeding and FA. Breastfeeding for more than 6 months increases the risk of FA in children, possibly due to the lack of a diversified diet hindering the development of early immunity. Due to the intricate nature of breastfeeding and the limitations of the types of included studies, further improvements and in-depth research are needed in the future.
Data availability
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- AR:
-
Allergic rhinitis
- FA:
-
Food allergy
- HDM-AR:
-
House dust mite-induced allergic rhinitis
- ISAAC:
-
International Study of Asthma and Allergies in Childhood
- JBI:
-
Joanna Briggs Institute
- MOOSE:
-
Meta-analysis of Observational Studies in Epidemiology
- NOS:
-
Newcastle-Ottawa Scale
- OR:
-
Odds ratios
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RR:
-
Relative risk
- SFAR:
-
Score for Allergic Rhinitis
- SPT:
-
Skin prick test
- WHO:
-
World Health Organization
- 95% CI:
-
95% Confidence intervals
References
Zhang Y, Lan F, Zhang L (2021) Advances and highlights in allergic rhinitis. Allergy 76:3383–3389
Frazier W, Bhardwaj N (2020) Atopic dermatitis: diagnosis and treatment. Am Fam Physician 101:590–598
Toskala E, Kennedy DW (2015) Asthma risk factors. Int Forum Allergy Rhinol 5(Suppl 1):S11-16
Alduraywish SA, Lodge CJ, Campbell B, Allen KJ, Erbas B, Lowe AJ, Dharmage SC (2016) The march from early life food sensitization to allergic disease: a systematic review and meta-analyses of birth cohort studies. Allergy 71:77–89
Pawankar R (2014) Allergic diseases and asthma: a global public health concern and a call to action. World Allergy Organ J 7:12
Arnold JJ, Williams PM (2011) Anaphylaxis: recognition and management. Am Fam Physician 84:1111–1118
Kilanowski A, Thiering E, Wang G, Kumar A, Kress S, Flexeder C, Bauer CP, Berdel D, von Berg A, Bergström A, Gappa M, Heinrich J, Herberth G, Koletzko S, Kull I, Melén E, Schikowski T, Peters A, Standl M (2023) Allergic disease trajectories up to adolescence: characteristics, early-life, and genetic determinants. Allergy 78:836–850
Akagawa S, Kaneko K (2022) Gut microbiota and allergic diseases in children. Allergol Int 71:301–309
Picciano MF (2001) Nutrient composition of human milk. Pediatr Clin North Am 48:53–67
Ballard O, Morrow AL (2013) Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am 60:49–74
Ladomenou F, Moschandreas J, Kafatos A, Tselentis Y, Galanakis E (2010) Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child 95:1004–1008
Vennemann MM, Bajanowski T, Brinkmann B, Jorch G, Yücesan K, Sauerland C, Mitchell EA (2009) Does breastfeeding reduce the risk of sudden infant death syndrome? Pediatrics 123:e406-410
Horta BL, de Lima NP (2019) Breastfeeding and type 2 diabetes: systematic review and meta-analysis. Curr Diab Rep 19:1
Lin D, Chen D, Huang J, Li Y, Wen X, Ou P, Shi H (2023) Breastfeeding is associated with reduced risks of central obesity and hypertension in young school-aged children: a large, population-based study. Int Breastfeed J 18:52
Lodge CJ, Tan DJ, Lau MX, Dai X, Tham R, Lowe AJ, Bowatte G, Allen KJ, Dharmage SC (2015) Breastfeeding and asthma and allergies: a systematic review and meta-analysis. Acta Paediatr 104:38–53
Hoang MP, Samuthpongtorn J, Seresirikachorn K, Snidvongs K (2022) Prolonged breastfeeding and protective effects against the development of allergic rhinitis: a systematic review and meta-analysis. Rhinology 60:82–91
Lyons SA, Knulst AC, Burney PGJ, Fernández-Rivas M, Ballmer-Weber BK, Barreales L, Bieli C, Clausen M, Dubakiene R, Fernández-Perez C, Jedrzejczak-Czechowicz M, Kowalski ML, Kummeling I, Mustakov TB, van Os-Medendorp H, Papadopoulos NG, Popov TA, Potts J, Xepapadaki P, Welsing PMJ, Mills ENC, van Ree R, Le TM (2020) Predictors of food sensitization in children and adults across Europe. J Allergy Clin Immunol Pract 8:3074-3083.e3032
Yuenyongviwat A, Koosakulchai V, Treepaiboon Y, Jessadapakorn W, Sangsupawanich P (2021) Risk factors of food sensitization in young children with atopic dermatitis. Asian Pac J Allergy Immunol 42:30–35
Saad K, Ahmad AR, El-Tellawy MM, El-Ashry AH, Nagiub EM, Abdelsalam TA, Elhoufey A (2020) Cow milk protein allergy: clinical phenotype and risk factors. Curr Trend Immunol 21:129–135
Matsumoto N, Yorifuji T, Nakamura K, Ikeda M, Tsukahara H, Doi H (2020) Breastfeeding and risk of food allergy: a nationwide birth cohort in Japan. Allergol Int 69:91–97
Tong H, Gao L, Deng Y, Kong Y, Xiang R, Tan L, Tao Z, Xu Y (2020) Prevalence of allergic rhinitis and associated risk factors in 6 to 12 years schoolchildren from Wuhan in Central China: a cross-sectional study. Am J Rhinol Allergy 34:632–641
Schmitz R, Atzpodien K, Schlaud M (2012) Prevalence and risk factors of atopic diseases in German children and adolescents. Pediatr Allergy Immunol 23:716–723
Rosas-Salazar C, Shilts MH, Tang ZZ, Hong Q, Turi KN, Snyder BM, Wiggins DA, Lynch CE, Gebretsadik T, Peebles RS Jr, Anderson LJ, Das SR, Hartert TV (2022) Exclusive breast-feeding, the early-life microbiome and immune response, and common childhood respiratory illnesses. J Allergy Clin Immunol 150:612–621
Ahmed A, Becker A (2019) Evaluation of eczema, asthma, allergic rhinitis and allergies among the grade-7 children of Iqaluit. Allergy Asthma Clin Immunol 15:26
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, Mulrow C, Catalá-López F, Gøtzsche PC, Dickersin K, Boutron I, Altman DG, Moher D (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162:777–784
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605
Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, Currie M, Qureshi R, Mattis P, Lisy K (2017) Chapter 7: Systematic reviews of etiology and risk. Joanna briggs institute reviewer’s manual. The Joanna Briggs Institute 5:217–269
Brenner H (1987) Comprehensive treatment at outpatient heart units. Offentl Gesundheitswes 49:102–104
Maki KC, Guyton JR, Orringer CE, Hamilton-Craig I, Alexander DD, Davidson MH (2016) Triglyceride-lowering therapies reduce cardiovascular disease event risk in subjects with hypertriglyceridemia. J Clin Lipidol 10:905–914
Tong X, Tong H, Gao L, Deng Y, Xiang R, Cen R, Zhao Y, Wang P, Li G, Shen J, Xu B, He B, Kong Y, Tao Z, Xu Y (2022) A multicenter study of prevalence and risk factors for allergic rhinitis in primary school children in 5 cities of Hubei Province, China. Int Arch Allergy Immunol 183:34–44
Sung WH, Yeh KW, Huang JL, Su KW, Chen KF, Wu CC, Tsai MH, Hua MC, Liao SL, Lai SH, Chiu CY (2022) Longitudinal changes in body mass index Z-scores during infancy and risk of childhood allergies. J Microbiol Immunol Infect 55:956–964
Pelak G, Wiese AM, Maskarinec JM, Phillips WL, Keim SA (2021) Infant feeding practices during the first postnatal year and risk of asthma and allergic disease during the first 6 years of life. Breastfeed Med 16:539–546
Lang A, Patel S, Rychlik K, Caruso D, Wang X, Pongracic JA, Kumar R (2021) Exploration of parent-reported food allergy symptoms via breastmilk exposures and likelihood to develop tolerance. Allergy Asthma Clin Immunol 17:102
Huang CF, Chie WC, Wang IJ (2021) Effect of environmental exposures on allergen sensitization and the development of childhood allergic diseases: a large-scale population-based study. World Allergy Organ J 14:100495
Hu Y, Chen Y, Liu S, Jiang F, Wu M, Yan C, Tan J, Yu G, Hu Y, Yin Y, Qu J, Li S, Tong S (2021) Breastfeeding duration modified the effects of neonatal and familial risk factors on childhood asthma and allergy: a population-based study. Respir Res 22:41
Ekelund L, Gloppen I, Øien T, Simpson MR (2021) Duration of breastfeeding, age at introduction of complementary foods and allergy-related diseases: a prospective cohort study. Int Breastfeed J 16:5
Amazouz H, de Lauzon-Guillain B, Bourgoin-Heck M, Just J, Beydon N, Lezmi G, Rancière F, Momas I (2021) Infant feeding clusters are associated with respiratory health and allergy at school age in the PARIS birth cohort. Allergy 76:1223–1234
Yu B, Dai L, Chen J, Sun W, Chen J, Du L, Deng N, Chen D (2019) Prenatal and neonatal factors involved in the development of childhood allergic diseases in Guangzhou primary and middle school students. BMC Pediatr 19:479
Sicherer SH, Wood RA, Perry TT, Jones SM, Leung DYM, Henning AK, Dawson P, Burks AW, Lindblad R, Sampson HA (2019) Clinical factors associated with peanut allergy in a high-risk infant cohort. Allergy 74:2199–2211
Kim YH, Kim KW, Lee SY, Koo KO, Kwon SO, Seo JH, Suh DI, Shin YH, Ahn K, Oh SY, Lee S, Sohn MH, Hong SJ (2019) Maternal perinatal dietary patterns affect food allergy development in susceptible infants. J Allergy Clin Immunol Pract 7:2337-2347.e2337
Han DH, Shin JM, An S, Kim JS, Kim DY, Moon S, Kim JS, Cho JS, Kim SW, Kim YH, Roh HJ, Shim WS, Rha KS, Kim SW, Lee SS, Kim DW, Cho KS, Yim HJ, Park SK, Rhee CS (2019) Long-term breastfeeding in the prevention of allergic rhinitis: Allergic Rhinitis Cohort Study for Kids (ARCO-Kids Study). Clin Exp Otorhinolaryngol 12:301–307
Davisse-Paturet C, Raherison C, Adel-Patient K, Divaret-Chauveau A, Bois C, Dufourg MN, Lioret S, Charles MA, de Lauzon-Guillain B (2019) Use of partially hydrolysed formula in infancy and incidence of eczema, respiratory symptoms or food allergies in toddlers from the ELFE cohort. Pediatr Allergy Immunol 30:614–623
Chinratanapisit S, Suratannon N, Pacharn P, Sritipsukho P, Vichyanond P (2019) Prevalence and risk factors of allergic rhinitis in children in Bangkok area. Asian Pac J Allergy Immunol 37:232–239
Wang XY, Zhuang Y, Ma TT, Zhang B, Wang XY (2018) Prevalence of self-reported food allergy in six regions of inner Mongolia, northern China: a population-based survey. Med Sci Monit 24:1902–1911
van Ginkel CD, van der Meulen GN, Bak E, Flokstra-de Blok BMJ, Kollen BJ, Koppelman GH, Dubois AEJ (2018) Retrospective observational cohort study regarding the effect of breastfeeding on challenge-proven food allergy. Eur J Clin Nutr 72:557–563
Sardecka I, Łoś-Rycharska E, Ludwig H, Gawryjołek J, Krogulska A (2018) Early risk factors for cow’s milk allergy in children in the first year of life. Allergy Asthma Proc 39:e44–e54
Bedolla-Barajas M, Morales-Romero J, Gaxiola-Arredondo BY, Alcalá-Padilla G, Romero-Velarde E (2018) Prolonged breastfeeding and delayed introduction of whole cow’s milk into the diet are factors associated with egg sensitization: a matched case-control study. Allergol Immunopathol (Madr) 46:539–545
Alkazemi D, Albeajan M, Kubow S (2018) Early infant feeding practices as possible risk factors for immunoglobulin E-mediated food allergies in Kuwait. Int J Pediatr 2018:1701903
Ahmed A, Hakim A, Becker A (2018) Evaluation of eczema, asthma, allergic rhinitis and allergies among the Grade-1 children of Iqaluit. Allergy Asthma Clin Immunol 14:9
Lee MT, Wu CC, Ou CY, Chang JC, Liu CA, Wang CL, Chuang H, Kuo HC, Hsu TY, Chen CP, Yang KD (2017) A prospective birth cohort study of different risk factors for development of allergic diseases in offspring of non-atopic parents. Oncotarget 8:10858–10870
Jonsson K, Barman M, Brekke HK, Hesselmar B, Johansen S, Sandberg AS, Wold AE (2017) Late introduction of fish and eggs is associated with increased risk of allergy development - results from the FARMFLORA birth cohort. Food Nutr Res 61:1393306
Huang C, Liu W, Cai J, Weschler LB, Wang X, Hu Y, Zou Z, Shen L, Sundell J (2017) Breastfeeding and timing of first dietary introduction in relation to childhood asthma, allergies, and airway diseases: a cross-sectional study. J Asthma 54:488–497
Gil F, Amezqueta A, Martinez D, Aznal E, Etayo V, Durá T, Sánchez-Valverde F (2017) Association between caesarean delivery and isolated doses of formula feeding in cow milk allergy. Int Arch Allergy Immunol 173:147–152
Elbert NJ, van Meel ER, den Dekker HT, de Jong NW, Nijsten TEC, Jaddoe VWV, de Jongste JC, Pasmans S, Duijts L (2017) Duration and exclusiveness of breastfeeding and risk of childhood atopic diseases. Allergy 72:1936–1943
Wang X, Liu W, Hu Y, Zou Z, Shen L, Huang C (2016) Home environment, lifestyles behaviors, and rhinitis in childhood. Int J Hyg Environ Health 219:220–231
Goldsmith AJ, Koplin JJ, Lowe AJ, Tang ML, Matheson MC, Robinson M, Peters R, Dharmage SC, Allen KJ (2016) Formula and breast feeding in infant food allergy: a population-based study. J Paediatr Child Health 52:377–384
Chiu CY, Liao SL, Su KW, Tsai MH, Hua MC, Lai SH, Chen LC, Yao TC, Yeh KW, Huang JL (2016) Exclusive or partial breastfeeding for 6 months is associated with reduced milk sensitization and risk of eczema in early childhood: the PATCH birth cohort study. Medicine (Baltimore) 95:e3391
Wang L, Qu F, Zhang Y, Weschler LB, Sundell J (2015) Home environment in relation to allergic rhinitis among preschool children in Beijing, China: a cross-sectional study. Build Environ 93:54–63
Li Y, Jiang Y, Li S, Shen X, Liu J, Jiang F (2015) Pre- and postnatal risk factors in relation to allergic rhinitis in school-aged children in China. PLoS ONE 10:e0114022
Kim NY, Kim GR, Kim JH, Baek JH, Yoon JW, Jee HM, Baek HS, Jung YH, Choi SH, Kim KE, Shin YH, Yum HY, Han MY, Kim KE (2015) Food allergen sensitization in young children with typical signs and symptoms of immediate-type food allergies: a comparison between monosensitized and polysensitized children. Korean J Pediatr 58:330–335
Jelding-Dannemand E, Malby Schoos AM, Bisgaard H (2015) Breast-feeding does not protect against allergic sensitization in early childhood and allergy-associated disease at age 7 years. J Allergy Clin Immunol 136:1302–1308. e1301–1313
Tamay Z, Akçay A, Ergin A, Güler N (2014) Prevalence of allergic rhinitis and risk factors in 6- to 7-yearold children in İstanbul, Turkey. Turk J Pediatr 56:31–40
Song N, Shamssain M, Zhang J, Wu J, Fu C, Hao S, Guan J, Yan X (2014) Prevalence, severity and risk factors of asthma, rhinitis and eczema in a large group of Chinese schoolchildren. J Asthma 51:232–242
Luccioli S, Zhang Y, Verrill L, Ramos-Valle M, Kwegyir-Afful E (2014) Infant feeding practices and reported food allergies at 6 years of age. Pediatrics 134(Suppl 1):S21-28
Liao SL, Lai SH, Yeh KW, Huang YL, Yao TC, Tsai MH, Hua MC, Huang JL (2014) Exclusive breastfeeding is associated with reduced cow’s milk sensitization in early childhood. Pediatr Allergy Immunol 25:456–461
Nwaru BI, Takkinen HM, Niemelä O, Kaila M, Erkkola M, Ahonen S, Tuomi H, Haapala AM, Kenward MG, Pekkanen J, Lahesmaa R, Kere J, Simell O, Veijola R, Ilonen J, Hyöty H, Knip M, Virtanen SM (2013) Introduction of complementary foods in infancy and atopic sensitization at the age of 5 years: timing and food diversity in a Finnish birth cohort. Allergy 68:507–516
Kellberger J, Dressel H, Vogelberg C, Leupold W, Windstetter D, Weinmayr G, Genuneit J, Heumann C, Nowak D, von Mutius E, Radon K (2012) Prediction of the incidence and persistence of allergic rhinitis in adolescence: a prospective cohort study. J Allergy Clin Immunol 129(397–402):402.e391–393
Chen BY, Chan CC, Han YY, Wu HP, Guo YL (2012) The risk factors and quality of life in children with allergic rhinitis in relation to seasonal attack patterns. Paediatr Perinat Epidemiol 26:146–155
Siriaksorn S, Suchaitanawanit S, Trakultivakorn M (2011) Allergic rhinitis and immunoglobulin deficiency in preschool children with frequent upper respiratory illness. Asian Pac J Allergy Immunol 29:73–77
Sandini U, Kukkonen AK, Poussa T, Sandini L, Savilahti E, Kuitunen M (2011) Protective and risk factors for allergic diseases in high-risk children at the ages of two and five years. Int Arch Allergy Immunol 156:339–348
Sahebi L, Shabestary MS (2011) The prevalence of asthma, allergic rhinitis, and eczema among middle school students in Tabriz (northwestern Iran). Turk J Med Sci 41:927–938
Hong X, Wang G, Liu X, Kumar R, Tsai HJ, Arguelles L, Hao K, Pearson C, Ortiz K, Bonzagni A, Apollon S, Fu L, Caruso D, Pongracic JA, Schleimer R, Holt PG, Bauchner H, Wang X (2011) Gene polymorphisms, breast-feeding, and development of food sensitization in early childhood. J Allergy Clin Immunol 128:374-381.e372
Björkstén B, Aït-Khaled N, Innes Asher M, Clayton TO, Robertson C (2011) Global analysis of breast feeding and risk of symptoms of asthma, rhinoconjunctivitis and eczema in 6–7 year old children: ISAAC Phase Three. Allergol Immunopathol (Madr) 39:318–325
Kusunoki T, Morimoto T, Nishikomori R, Yasumi T, Heike T, Mukaida K, Fujii T, Nakahata T (2010) Breastfeeding and the prevalence of allergic diseases in schoolchildren: does reverse causation matter? Pediatr Allergy Immunol 21:60–66
Sánchez-Valverde F, Gil F, Martinez D, Fernandez B, Aznal E, Oscoz M, Olivera JE (2009) The impact of caesarean delivery and type of feeding on cow’s milk allergy in infants and subsequent development of allergic march in childhood. Allergy 64:884–889
Kramer MS, Matush L, Bogdanovich N, Dahhou M, Platt RW, Mazer B (2009) The low prevalence of allergic disease in Eastern Europe: are risk factors consistent with the hygiene hypothesis? Clin Exp Allergy 39:708–716
Kljakovic M, Gatenby P, Hawkins C, Attewell RG, Ciszek K, Kratochvil G, Moreira A, Ponsonby AL (2009) The parent-reported prevalence and management of peanut and nut allergy in school children in the Australian Capital Territory. J Paediatr Child Health 45:98–103
Ehlayel MS, Bener A (2008) Duration of breast-feeding and the risk of childhood allergic diseases in a developing country. Allergy Asthma Proc 29:386–391
Miyake Y, Arakawa M, Tanaka K, Sasaki S, Ohya Y (2007) Cross-sectional study of allergic disorders associated with breastfeeding in Japan: the Ryukyus Child Health Study. Pediatr Allergy Immunol 18:433–440
Kurt E, Metintas S, Basyigit I, Bulut I, Coskun E, Dabak S, Deveci F, Fidan F, Kaynar H, Uzaslan EK, Onbasi K, Ozkurt S, Pasaoglu G, Sahan S, Sahin U, Oguzulgen K, Yildiz F, Mungan D, Yorgancioglu A, Gemicioglu B, Fuat Kalyoncu A (2007) Prevalence and risk factors of allergies in Turkey: Results of a multicentric cross-sectional study in children. Pediatr Allergy Immunol 18:566–574
Pesonen M, Kallio MJ, Ranki A, Siimes MA (2006) Prolonged exclusive breastfeeding is associated with increased atopic dermatitis: a prospective follow-up study of unselected healthy newborns from birth to age 20 years. Clin Exp Allergy 36:1011–1018
Obihara CC, Marais BJ, Gie RP, Potter P, Bateman ED, Lombard CJ, Beyers N, Kimpen JL (2005) The association of prolonged breastfeeding and allergic disease in poor urban children. Eur Respir J 25:970–977
Milner JD, Stein DM, McCarter R, Moon RY (2004) Early infant multivitamin supplementation is associated with increased risk for food allergy and asthma. Pediatrics 114:27–32
Kull I, Wickman M, Lilja G, Nordvall SL, Pershagen G (2002) Breast feeding and allergic diseases in infants-a prospective birth cohort study. Arch Dis Child 87:478–481
Wetzig H, Schulz R, Diez U, Herbarth O, Viehweg B, Borte M (2000) Associations between duration of breast-feeding, sensitization to hens’ eggs and eczema infantum in one and two year old children at high risk of atopy. Int J Hyg Environ Health 203:17–21
Saarinen KM, Savilahti E (2000) Infant feeding patterns affect the subsequent immunological features in cow’s milk allergy. Clin Exp Allergy 30:400–406
Saarinen KM, Juntunen-Backman K, Järvenpää AL, Klemetti P, Kuitunen P, Lope L, Renlund M, Siivola M, Vaarala O, Savilahti E (2000) Breast-feeding and the development of cows’ milk protein allergy. Adv Exp Med Biol 478:121–130
Butland BK, Strachan DP, Lewis S, Bynner J, Butler N, Britton J (1997) Investigation into the increase in hay fever and eczema at age 16 observed between the 1958 and 1970 British birth cohorts. BMJ 315:717–721
Strachan DP, Taylor EM, Carpenter RG (1996) Family structure, neonatal infection, and hay fever in adolescence. Arch Dis Child 74:422–426
Vilar-Compte M, Pérez-Escamilla R, Ruano AL (2022) Interventions and policy approaches to promote equity in breastfeeding. Int J Equity Health 21:63
Gabryszewski SJ, Dudley J, Grundmeier RW, Hill DA (2021) Early-life environmental exposures associate with individual and cumulative allergic morbidity. Pediatr Allergy Immunol 32:1089–1093
Li Y, Lin Y, Jiang Y, Rui X, Ma B, Li J (2022) GWAS-identified variants to allergic disease and early environmental exposure in Chinese schoolchildren with allergic rhinitis induced by house dust mite. Asian Pac J Allergy Immunol 40:55–64
Chen J, Liu X, Liu Z, Zhou Y, Xie L, Zhang J, Tan J, Yang Y, Tian M, Dong Y, Li J (2023) Early exposure to infections increases the risk of allergic rhinitis-a systematic review and meta-analysis. BMC Pediatr 23:96
Prescott S, Allen KJ (2011) Food allergy: riding the second wave of the allergy epidemic. Pediatr Allergy Immunol 22:155–160
Rueter K, Moseley N, Ta B, Bear N, Borland ML, Prescott SL (2023) Increasing emergency department visits for anaphylaxis in very early childhood: a canary in the coal mine. Acta Paediatr 112:2182–2188
Ruel MT (2003) Is dietary diversity an indicator of food security or dietary quality? A review of measurement issues and research needs. Food Nutr Bull 24:231–232
Leeming ER, Johnson AJ, Spector TD, Le Roy CI (2019) Effect of diet on the gut microbiota: rethinking intervention duration. Nutrients 11:2862
Roduit C, Frei R, Ferstl R, Loeliger S, Westermann P, Rhyner C, Schiavi E, Barcik W, Rodriguez-Perez N, Wawrzyniak M, Chassard C, Lacroix C, Schmausser-Hechfellner E, Depner M, von Mutius E, Braun-Fahrländer C, Karvonen AM, Kirjavainen PV, Pekkanen J, Dalphin JC, Riedler J, Akdis C, Lauener R, O’Mahony L (2019) High levels of butyrate and propionate in early life are associated with protection against atopy. Allergy 74:799–809
Arpaia N, Campbell C, Fan X, Dikiy S, van der Veeken J, deRoos P, Liu H, Cross JR, Pfeffer K, Coffer PJ, Rudensky AY (2013) Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature 504:451–455
Ríos-Covián D, Ruas-Madiedo P, Margolles A, Gueimonde M, de Los Reyes-Gavilán CG, Salazar N (2016) Intestinal short chain fatty acids and their link with diet and human health. Front Microbiol 7:185
Berni Canani R, De Filippis F, Nocerino R, Laiola M, Paparo L, Calignano A, De Caro C, Coretti L, Chiariotti L, Gilbert JA, Ercolini D (2017) Specific signatures of the gut microbiota and increased levels of butyrate in children treated with fermented cow’s milk containing heat-killed Lactobacillus paracasei CBA L74. Appl Environ Microbiol 83:e01206–17
Sampath V, Abrams EM, Adlou B, Akdis C, Akdis M, Brough HA, Chan S et al (2021) Food allergy across the globe. J Allergy Clin Immunol 148:1347–1364
Prescott SL, Smith P, Tang M, Palmer DJ, Sinn J, Huntley SJ, Cormack B, Heine RG, Gibson RA, Makrides M (2008) The importance of early complementary feeding in the development of oral tolerance: concerns and controversies. Pediatr Allergy Immunol 19:375–380
Perkin MR, Logan K, Tseng A, Raji B, Ayis S, Peacock J, Brough H, Marrs T, Radulovic S, Craven J, Flohr C, Lack G (2016) Randomized trial of introduction of allergenic foods in breast-fed infants. N Engl J Med 374:1733–1743
Hicke-Roberts A, Wennergren G, Hesselmar B (2020) Late introduction of solids into infants’ diets may increase the risk of food allergy development. BMC Pediatr 20:273
Caroli M, Vania A, Verga MC, Di Mauro G, Bergamini M, Cuomo B, D’Anna R et al (2022) Recommendations on complementary feeding as a tool for prevention of non-communicable diseases (NCDs)-paper co-drafted by the SIPPS, FIMP, SIDOHaD, and SINUPE Joint Working Group. Nutrients 14:257
Funding
This work was supported by the National Natural Science Foundation of China (82174436); Scientific Research Program of Wuxi Municipal Health Commission (M202231).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Writing—original draft preparation: Yali Ding, Chengbi Zhu; writing—review and editing: Bin Yuan, Changjiang Zhao, Yali Ding, Chengbi Zhu; conceptualization: Yali Ding, Chengbi Zhu; methodology: Yali Ding, Chengbi Zhu; formal analysis and investigation: Shuo Li, Naixu Liu, Qian Liu, Weifeng Li; funding acquisition: Bin Yuan, Changjiang Zhao; resources: Shuo Li, Naixu Liu, Qian Liu, Weifeng Li, Changjiang Zhao; supervision: Bin Yuan, Changjiang Zhao; and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Tobias Tenenbaum
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ding, Y., Zhu, C., Li, S. et al. Breastfeeding and risk of food allergy and allergic rhinitis in offspring: a systematic review and meta-analysis of cohort studies. Eur J Pediatr (2024). https://doi.org/10.1007/s00431-024-05580-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00431-024-05580-w