Abstract
While neonatal necrotising enterocolitis (NEC) is associated with high mortality rates in newborns, survivors can face long-term sequelae. However, the relationship between NEC and neurodevelopmental impairment (NDI) in preterm infants remains unclear. To explore the relationship between neonatal NEC and neurodevelopmental outcomes in preterm infants, we searched PubMed, EMBASE, and the Cochrane Library from their inception to February 2024 for relevant studies. Studies included were cohort or case–control studies reporting neurodevelopmental outcomes of NEC in preterm infants. Two independent investigators extracted data regarding brain damage and neurodevelopmental outcomes in these infants at a corrected age exceeding 12 months. Odds ratios (ORs) were pooled using a random effects model. We included 15 cohort studies and 18 case–control studies, encompassing 60,346 infants. Meta-analysis of unadjusted and adjusted ORs demonstrated a significant association between NEC and increased odds of NDI (OR 2.15, 95% CI 1.9–2.44; aOR 1.89, 95% CI 1.46–2.46). Regarding brain injury, pooled crude ORs indicated an association of NEC with severe intraventricular haemorrhage (IVH) (OR 1.42, 95% CI 1.06–1.92) and periventricular leucomalacia (PVL) (OR 2.55, 95% CI 1.76–3.69). When compared with conservatively treated NEC, surgical NEC potentially carries a higher risk of NDI (OR 1.78, 95% CI 1.09–2.93) and severe IVH (OR 1.57, 95% CI 1.20–2.06). However, the risk of PVL did not show a significant difference (OR 1.60, 95% CI 0.47–5.40).
Conclusions: Our meta-analysis provides evidence suggesting an association between NEC and NDI. Additionally, the severity of intestinal lesions appears to correlate with a higher risk of NDI. Further high-quality studies with comprehensive adjustments for potential confounding factors are required to definitively establish whether the association with NDI is causal.
What is Known: • NEC is a serious intestinal disease in the neonatal period with a high mortality rate, and surviving children may have digestive system sequelae. • Compared with non-NEC preterm infants, the reported incidences of brain injury and neurodevelopmental disorders in NEC preterm infants are not the same. | |
What is New: • The risk of neonatal brain injury and neurodevelopmental disorders in preterm infants with NEC is higher than that in non-NEC infants, and the risk of NDI in surgical NEC infants is higher than that in the conservative treatment group. • NEC may increase the risk of motor, cognitive, language development delays, and attention deficits in children. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Necrotising enterocolitis (NEC) is a severe gastrointestinal disease that occurs during the neonatal period and is a major cause of neonatal mortality. Neonatal intensive care units report an incidence of 2–5%. This is particularly concerning for very low birth weight (VLBW) infants, who experience a 2–7% incidence rate [1]. Mortality rates for NEC remain high, with estimates reaching 20–30% [2]. Moreover, 9–36% of surviving children face long-term digestive system sequelae such as short bowel syndrome and intestinal stenosis [3]. Studies indicate a substantial financial burden on families and society due to the increased medical costs associated with NEC, especially for those requiring surgery during their early childhood development [4].
Beyond digestive system complications, children with NEC are at risk of neurodevelopmental impairment (NDI) [5]. The incidence of NDI in these children is approximately 40%, which is twice that in children without NEC [6]. Research suggests a higher risk of intracranial haemorrhage (IVH), periventricular leukomalacia (PVL), cerebral palsy (CP), and severe visual and hearing impairment in children with NEC. Additionally, compared with medical management, surgical intervention for NEC appears to elevate the risk of NDI. However, some studies have failed to find an increased risk of NDI in children with NEC during the neonatal period [4]. Although different types of NDIs in NEC survivors have been reported, most studies have not adjusted for other factors associated with brain injury, such as gestational age, birth weight, and infection. Notably, some studies suggest a higher risk of behavioural problems, such as attention deficits in NEC survivors during childhood [6], while others have not observed such a connection [7]. Our study aims to address these inconsistencies. We conducted a comprehensive review of NEC and its neurological sequelae in children. This analysis extends to systematically evaluate the risk of various functional and behavioural brain disorders in children with NEC. This information will serve as a valuable reference for targeted early rehabilitation interventions for children with NEC.
Methods
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [8], we conducted a systematic review and meta-analysis. The protocol and search strategies were registered in PROSPERO (CRD42024509168) (crd.york.ac.uk/PROSPERO/display_record.php?RecordID = 509,168).
Retrieval of studies
A systematic search of PubMed, EMBASE, and the Cochrane Library was conducted to identify related studies. The search strategy used in this study is described in Supplementary data 1. Only human studies published in English were included in this analysis. When studies shared overlapping participants, the one with the largest sample size was chosen. We also identified additional candidates by manually searching the references of included research articles, meta-analyses, and reviews.
Inclusion and exclusion criteria
Inclusion criteria for our study were as follows: (1) those with a cohort or case–control design; (2) those that reported brain injury IVH or PVL, neurodevelopmental outcomes CP, any disability, severe disability, visual impairment, hearing impairment, and language delay or behavioural difficulties (attention-deficit/hyperactivity disorder [ADHD] or autism) in preterm infants; (3) those with developmental follow-up performed at ≥ 1 year corrected age; (4) those with defined NEC diagnosis criteria (Bell’s stage II or III, or diagnosed clinically/radiologically); and (5) those that provided total participants, number of cases, odds ratios (ORs), hazard ratios (HRs), or risk ratios (RRs) with 95% confidence interval (CI).
Studies were excluded if they (1) were case reports, reviews, and animal studies; (2) focussed on term neonates; (3) had overlapping data; and (4) lacked raw data. Surgical NEC was defined as NEC requiring laparotomy, laparoscopy, or peritoneal drainage. Medical NECs were treated without surgical intervention.
Data extraction and quality assessment
Two independent reviewers extracted data on the first author, publication year, country, study design, gestational age/birth weight, number of cases and total sample population, NDI category, age at follow-up, and developmental assessment scale. Differences in opinion were resolved through discussion among all reviewers.
The methodological quality of each study was examined using the Newcastle–Ottawa Scale (NOS) with a maximum score of nine. The quality of the studies was divided into three categories: high (score 7–9), moderate (score 4–6), and low (score 0–3) [9].
Statistical analysis
Stata version 18.0 (Stata Corporation, College Station, TX, USA) was used for the meta-analysis. A random-effects model was employed as anticipated. Pooled estimates included both adjusted and unadjusted ORs with 95% CIs from the included studies. If studies lacked ORs, they were calculated from raw data. The I2 statistic (significance level, > 50%) and Q statistic (significance level, P < 0.10) were used to assess the heterogeneity between studies. We also performed a sensitivity analysis by sequentially excluding each study. The possibility of publication bias was visually assessed using Egger’s and Begg’s tests (significance level, P < 0.05). Additionally, the “trim and fill” procedure was performed to evaluate potential publication bias in our meta-analysis further.
Results
Literature search and selection
A comprehensive search identified 5287 articles (PubMed, 1122; EMBASE, 3086; Cochrane Library, 1079). Following careful screening, 33 studies were selected for inclusion (Fig. 1). There were 15 cohort studies and 18 case–control studies.
Study characteristics
The characteristics of the 33 selected studies are presented in Table 1. The selected studies spanned publication years between 1989 and 2023. Geographically, the studies originated from North America (14) [7, 10,11,12,13,14,15,16,17,18,19,20,21,22], Europe (9) [23,24,25,26,27,28,29,30], Australia (4) [31,32,33,34], China (1) [35], Japan (2) [36, 37], Taiwan (2) [38, 39], and one multicentre study [40]. Birth weight and gestational age criteria varied: 15 studies included infants < 1000 g or < 28 weeks gestation, 16 included those < 1500 g, and two studies involved all preterm infants. Per the NOS, the methodological quality was generally good, with 21 high-quality and 12 moderate-quality studies (Supplementary data 2 sTable 1).
Brain injury in NEC
IVH and PVL are the primary brain injuries that occur in the early postnatal period in preterm infants and are important risk factors for severe long-term neurodevelopmental problems. This study suggests that the risk of severe IVH and PVL in children with NEC is higher than that in those without NEC (OR 1.42, 95% CI 1.06–1.92; OR 2.547, 95% CI 1.76–3.69) (Fig. 2).
NDI in NEC
Our analysis indicated that the risk of NDI in preterm infants was significantly higher in NEC, with a pooled crude OR of 2.15 (95% CI 1.90–2.44) (Fig. 3a) and an adjusted OR of 1.89 (95% CI 1.46–2.46). No statistically significant heterogeneity was found across the studies (I2 = 32.9%; P > 0.05). Pooled unadjusted ORs from studies showed that compared with the non-NEC control group, NEC was significantly associated with CP (OR 2.02, 95% CI 1.52–2.68), visual impairment (OR 3.34, 95% CI 1.82–6.13), and hearing impairment (OR 2.77, 95% CI 1.62–4.72) (Fig. 3b). However, after adjusting for confounders including gestational age, weight, prenatal hormones, and infection, etc. (Supplementary data 2 sTable 2), the adjusted pooled OR (OR 1.26, 95% CI 0.70–2.25) did not suggest a relationship between NEC and the onset of CP (Fig. 3c).
Forest plot of neurodevelopmental impairment (NDI) in preterm infants with necrotising enterocolitis (NEC) compared with none NEC controls. a Pooling crude ORs of Overall NDI. b Pooling crude ORs of cerebral palsy, visual impairment, and hearing impairment. c Pooling adjusted ORs of NDI and cerebral palsy
Furthermore, the study found the proportion of children with NEC at a corrected age of over 1 year who scored below 70 on the physical development index (PDI) (OR 2.31, 95% CI 1.78–3.00) or mental development index (MDI) (OR 2.01, 95% CI 1.77–2.27) of a developmental assessment, or who had abnormal language assessment scores (OR 1.77, 95% CI 1.11–2.82). This indicates that the risk of motor developmental delay and cognitive and language developmental delay may increase in children with NEC. Although Pike et al. [41] found that ADHD was more common in children with NEC than in controls (15% vs. 8%), the pooled ORs in this study did not suggest a link between ADHD and NEC (OR 1.62, 95% CI 0.79–3.33). However, only three related articles were included in this analysis, exhibiting high heterogeneity (I2 = 75.2%); further studies are needed to clarify the relationship between ADHD and NEC (Fig. 4).
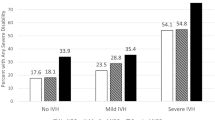
We also studied the effects of NEC severity on brain development. Compared with the surgical NEC group, the risk of severe IVH in the conservatively treated NEC group was higher (OR 1.57, 95% CI 1.20–2.06). However, the risk of PVL was not significantly different between both groups (OR 1.60, 95% CI 0.47–5.40) (Fig. 5a). It is important to note that only two studies were included in the surgical NEC vs. conservative NEC analysis; they exhibited high heterogeneity (I2 = 62.7%). The risk of NDI in children with surgical NEC was higher than that in the conservative treatment group (OR 1.78, 95% CI 1.09–2.93). Unadjusted pooled ORs indicated that the risk of developing cerebral palsy, visual impairment, and hearing impairment in children who underwent surgery was higher than that in the conservative treatment group (Fig. 5b). Regarding functional development, the risk of motor, intellectual, or language developmental delays was higher in the surgical NEC group than in the non-surgical NEC group (Fig. 5c).
Sensitivity analyses and publication bias
The overall pooled result did not vary substantially (Supplementary data 2 sTable 3) after excluding one study in each turn. Visual inspection of the funnel plot indicated a potential publication bias for NDI and NEC, and Begg’s test confirmed statistically significance (z = 2.85; P = 0.004). We further performed a sensitivity analysis using the trim-and-fill method, which estimated the number of missing studies that may cause funnel plot asymmetry and imputed the hypothetical studies to produce a symmetrical funnel plot (Fig. 6). Although seven theoretically missing trials were incorporated, the analysis still showed a significant association between NDI and NEC.
Discussion
Our meta-analysis of 33 studies encompassing 60,346 participants indicates that NEC is associated with an increased incidence of NDI, even after adjusting for various confounding factors. In addition, infants requiring surgery for NEC seem to have poorer neurological outcomes than those treated conservatively; however, most of the included studies did not adjust for potential confounders, necessitating further research to solidify this association.
Matei et al. [5] published a systematic review on the neurodevelopmental impairment in necrotizing enterocolitis survivors in 2019. A total of 2403 NEC infants were included, and the incidence of neurodevelopmental impairment was 40%, which was higher in surgical NEC infants than in those with conservative treatment. However, the included literature included full-term and premature infants, and the heterogeneity was high (I2 = 57%). From 2020 to 2024, there were three studies [19; 21; 28] with large sample reported on the neurodevelopmental injuries in the NEC survivors. In this review, we updated the latest researches, with a larger sample size including a total of 12,409 NEC infants.
Mechanisms underlying NEC-induced brain injury and neurodevelopmental disorders remain unclear. While previously attributed solely to prematurity, studies have shown more severe brain injury in NEC infants compared with non-NEC preemies of equivalent gestational age or those with spontaneous intestinal perforation. This suggests that additional factors beyond prematurity contribute to NEC brain injury [42].
The mechanisms underlying NEC-induced brain injury may be multifactorial. Changes in cerebral haemodynamic may cause brain injury in children with NEC. Children with NEC, especially those who require surgery, often experience hypotension, shock, and acidosis. These can damage cerebrovascular regulatory function, decrease cerebral blood flow, and lead to subsequent hypoxia and ischaemia. The inflammatory response is also considered an important mechanism in the occurrence of NEC-induced brain injury. Animal experiments have shown disrupted brain barrier function in NEC model models, allowing inflammatory blood to enter the brain tissue, activate microglia, trigger neuroinflammation, and ultimately reduce the number of neurons, oligodendrocyte precursors, and neural progenitor cells in the hippocampus, basal ganglia, and cerebral cortex [43, 44]. Beyond the influx of inflammatory factors into the brain, activation of the small intestine’s toll-like receptor (TLR) signalling pathway during NEC leads to the release of high-mobility group box-1 protein, which then enters and activates microglia, resulting in neurofunctional disorders [45]. Additionally, during NEC, enteral CD4 + T enters the brain and releases interferon-γ, activating microglia within the brain and causing myelin loss [46].
Adequate nutrition is a prerequisite for the brain development of preterm infants. Malnutrition during this critical window can lead to reduced brain cells, impaired myelin production, and decreased synapse formation. However, parenteral nutrition (PN) appears to be as efficient as enteral feeding in maintaining adequate nutrition. Children with NEC often receive long-term IV nutrition in the early postnatal period. Studies have shown that parenteral nutrition exceeding 20 days is linked to cognitive impairment in children with NEC aged 2–3 years [47].
This study had several advantages. The large sample size of our study allowed for a much greater possibility of reaching reliable conclusions about the association between NDI and NEC. The positive association between NDI and NEC persisted even after adjusting for confounding factors, demonstrating the high reliability of our findings. Our study also examined the different types of NDI separately. NEC may increase the risk of cerebral palsy in newborns; however, after adjusting for gestational age and birth weight, the combined OR did not suggest a relationship between NEC and cerebral palsy. Therefore, further high-quality studies are needed to clarify this relationship. Our study also suggests that the occurrence of blindness; hearing impairment; and delayed motor, cognitive, and language development during childhood is higher in children with NEC than in those without. However, factors such as gestational age and foetal age may be related to the development of the newborn brain. The possible confounding factors were not adjusted for in the included studies and the related relationships need to be explored further.
The limitations of this study should also be considered. First, most included studies did not adjust for confounding factors affecting child neurodevelopment (e.g., gestational age, birth weight, infection). Second, inconsistency exists in the definition of NDI, and the assessment criteria used are not the same (e.g., while some studies utilised the Bailey scale assessment criterion, others employed the Wechsler scale). Third, most studies were retrospective, with inherent limitations in data control, potentially introducing bias due to incomplete data. Additional well-designed prospective studies reporting adjusted OR are required to confirm our findings.
In conclusion, our study suggests that children with NEC have a higher incidence of brain injury and neurodevelopmental disorders than preterm infants without NEC, and the severity of NDI appears to be related to the degree of intestinal injury. However, the relationship between cerebral palsy and NEC requires further investigation. The risks of blindness, hearing impairment, motor developmental delay, cognitive impairment, and attention deficits seem to be higher in children with NEC than in those without NEC. These findings inform clinical follow-up practices, enabling earlier targeted rehabilitation interventions and potentially improving prognoses. However, most of the included studies did not adjust for confounding factors, and high-quality studies adjusting for factors such as gestational age, birth weight, prenatal hormone use, and infection are needed to definitively assess the NEC-NDI association. Additionally, the mechanisms underlying NDI in children with NEC remain unclear, and effective preventive and treatment methods are lacking. Further research is warranted to address these knowledge gaps.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- ADHD:
-
Attention-deficit/hyperactivity disorder
- CP:
-
Cerebral palsy
- CI:
-
Confidence interval
- HRs:
-
Hazard ratios
- IVH:
-
Intraventricular haemorrhage
- MDI:
-
Mental development index
- NDI:
-
Neurodevelopment impairment
- NEC:
-
Necrotizing enterocolitis
- NOS:
-
Newcastle-Ottawa Scale
- ORs:
-
Odds ratios
- PDI:
-
Physical development index
- PN:
-
Parenteral nutrition
- PVL:
-
Periventricular leukomalacia
- RRs:
-
Risk ratios
- VLBW:
-
Very low birth weight
- TLR:
-
Toll-like receptor
References
He Y, Zhang M, Tang J, Liu W, Hu Y, Shi J, Wang H, Xiong T, Zhang L, Ying J, Mu D (2024) A retrospective cohort study on mortality, morbidity, and care practices for 1750 very low birth weight infants, 2016–2021. Chin Med J (Engl)
Jiang S, Yan W, Li S, Zhang L, Zhang Y, Shah PS, Shah V, Lee SK, Yang Y, Cao Y (2020) Mortality and morbidity in infants <34 weeks’ gestation in 25 NICUs in China: a prospective cohort study. Front Pediatr 8:33
Duro D, Kalish LA, Johnston P, Jaksic T, McCarthy M, Martin C, Dunn JC, Brandt M, Nobuhara KK, Sylvester KG, Moss RL, Duggan C (2010) Risk factors for intestinal failure in infants with necrotizing enterocolitis: a Glaser Pediatric Research Network study. J Pediatr 157:203-208.e201
Ganapathy V, Hay JW, Kim JH, Lee ML, Rechtman DJ (2013) Long term healthcare costs of infants who survived neonatal necrotizing enterocolitis: a retrospective longitudinal study among infants enrolled in Texas Medicaid. BMC Pediatr 13:127
Matei A, Montalva L, Goodbaum A, Lauriti G, Zani A (2020) Neurodevelopmental impairment in necrotising enterocolitis survivors: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 105:432–439
Hansen ML, Jensen IV, Gregersen R, Juhl SM, Greisen G (2019) Behavioural and neurodevelopmental impairment at school age following necrotising enterocolitis in the newborn period. PLoS ONE 14
Vaidya R, Yi JX, O'Shea TM, Jensen ET, Joseph RM, Shenberger J, Gogcu S, Wagner K, Msall ME, Thompson AL, Frazier JA, Fry R, Singh R (2022) Long-term outcome of necrotizing enterocolitis and spontaneous intestinal perforation. Pediatrics 150
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L et al (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372:n160
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605
Walsh MC, Kliegman RM, Hack M (1989) Severity of necrotizing enterocolitis: influence on outcome at 2 years of age. Pediatrics 84:808–814
Simon NP, Brady NR, Stafford RL, Powell RW (1993) no age match-the effect of abdominal incisions on early motor development of infants with necrotizing enterocolitis. Dev Med Child Neurol 35:49–53
Hintz SR, Kendrick DE, Stoll BJ, Vohr BR, Fanaroff AA, Donovan EF, Poole WK, Blakely ML, Wright L, Higgins R (2005) Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics 115:696–703
Salhab WA, Perlman JM, Silver L, Broyles RS (2004) Necrotizing enterocolitis and neurodevelopmental outcome in extremely low birth weight infants < 1000 g. J Perinatol 24:534–540
Jen HC, Graber JJ, Hill JL, Alaish SM, Voigt RW, Strauch ED (2006) Surgical necrotizing enterocolitis and intraventricular hemorrhage in premature infants below 1000 g. J Pediatr Surg 41:1425–1430
Martin CR, Dammann O, Allred EN, Patel S, O’Shea TM, Kuban KCK, Leviton A (2010) Neurodevelopment of extremely preterm infants who had necrotizing enterocolitis with or without late bacteremia. J Pediatr 157:751-756.e751
Maitre NL, Marshall DD, Goldstein RF, Slaughter JC, Price WA (2011) Necrotizing enterocolitis in infants with periventricular hemorrhagic infarction: associations and outcomes. Neonatology 99:97–103
Shah TA, Meinzen-Derr J, Gratton T, Steichen J, Donovan EF, Yolton K, Alexander B, Narendran V, Schibler KR (2012) Hospital and neurodevelopmental outcomes of extremely low-birth-weight infants with necrotizing enterocolitis and spontaneous intestinal perforation. J Perinatol 32:552–558
Wadhawan R, Oh W, Hintz SR, Blakely ML, Das A, Bell EF, Saha S, Laptook AR, Shankaran S, Stoll BJ, Walsh MC, Higgins RD (2014) Neurodevelopmental outcomes of extremely low birth weight infants with spontaneous intestinal perforation or surgical necrotizing enterocolitis. J Perinatol 34:64–70
Culbreath K, Keefe G, Nes E, Edwards EM, Knell J, Morrow KA, Soll RF, Jaksic T, Horbar JD, Modi BP (2024) Association between neurodevelopmental outcomes and concomitant presence of NEC and IVH in extremely low birth weight infants. J Perinatol 44:108–115
Fullerton BS, Hong CR, Velazco CS, Mercier CE, Morrow KA, Edwards EM, Ferrelli KR, Soll RF, Modi BP, Horbar JD, Jaksic T (2018) Severe neurodevelopmental disability and healthcare needs among survivors of medical and surgical necrotizing enterocolitis: a prospective cohort study. J Pediatr Surg 53:101–107
Zozaya C, Shah J, Pierro A, Zani A, Synnes A, Lee S, Shah PS (2021) age not matched Neurodevelopmental and growth outcomes of extremely preterm infants with necrotizing enterocolitis or spontaneous intestinal perforation. J Pediatr Surg 56:309–316
Soraisham AS, Amin HJ, Al-Hindi MY, Singhal N, Sauve RS (2006) Does necrotising enterocolitis impact the neurodevelopmental and growth outcomes in preterm infants with birthweight < or =1250 g? J Paediatr Child Health 42:499–504
Sonntag J, Grimmer I, Scholz T, Metze B, Wit J, Obladen M (2000) Growth and neurodevelopmental outcome of very low birthweight infants with necrotizing enterocolitis. Acta Paediatr Int J Paediatr 89:528–532
Saldir M, Sarici SU, Bakar EE, Özcan O (2010) Neurodevelopmental status of preterm newborns at infancy, born at a Tertiary Care Center in Turkey. Am J Perinatol 27:121–128
Roze E, Ta BD, van der Ree MH, Tanis JC, van Braeckel KN, Hulscher JB, Bos AF (2011) Functional impairments at school age of children with necrotizing enterocolitis or spontaneous intestinal perforation. Pediatr Res 70:619–625
Dilli D, Eras Z, Ulu HO, Dilmen U, Şakrucu ED (2012) Does necrotizing enterocolitis affect growth and neurodevelopmental outcome in very low birth weight infants? Pediatr Surg Int 28:471–476
Allendorf A, Dewitz R, Weber J, Bakthiar S, Schloesser R, Rolle U (2018) Necrotizing enterocolitis as a prognostic factor for the neurodevelopmental outcome of preterm infants - match control study after 2 years. J Pediatr Surg 53:1573–1577
Humberg A, Spiegler J, Fortmann MI, Zemlin M, Marissen J, Swoboda I, Rausch TK, Herting E, Göpel W, Härtel C (2020) Surgical necrotizing enterocolitis but not spontaneous intestinal perforation is associated with adverse neurological outcome at school age. Sci Rep 10:2373
Imren C, Vlug LE, De Koning BAE, Diertens T, Snel HE, Suurland J, Swarte RMC, Vermeulen MJ, Keyzer-Dekker CMG (2022) Necrotizing enterocolitis in a Dutch cohort of very preterm infants: prevalence, mortality, and long-term outcomes. Eur J Pediatr Surg 32:111–119
Vallant N, Haffenden V, Peatman O, Khan H, Lee G, Thakkar H, Yardley I (2022) Outcomes for necrotising enterocolitis (NEC) in babies born at the threshold of viability: a case-control study. BMJ paediatrics open 6
Mayr J, Fasching G, Höllwarth ME (1994) Psychosocial and psychomotoric development of very low birthweight infants with necrotizing enterocolitis. Acta paediatrica (Oslo, Norway : 1992) Supplement 396:96–100
Tobiansky R, Lui K, Roberts S, Veddovi M (1995) Neurodevelopmental outcome in very low birthweight infants with necrotizing enterocolitis requiring surgery. J Paediatr Child Health 31:233–236
Waugh J, O’Callaghan MJ, Tudehope DI, Mohay HA, Burns YR, Gray PH, Rogers YM (1996) Prevalence and aetiology of neurological impairment in extremely low birthweight infants. J Paediatr Child Health 32:120–124
Chacko J, Ford WD, Haslam R (1999) Growth and neurodevelopmental outcome in extremely-low-birth-weight infants after laparotomy. Pediatr Surg Int 15:496–499
Chen S, Xiao X, Lin S, Zhu J, Liang L, Zhu M, Yang Z, Chen S, Lin Z, Liu Y (2021) Early aEEG can predict neurodevelopmental outcomes at 12 to 18 month of age in VLBWI with necrotizing enterocolitis: a cohort study. BMC Pediatr 21:582
Hayakawa M, Taguchi T, Urushihara N, Yokoi A, Take H, Shiraishi J, Fujinaga H, Ohashi K, Oshiro M, Kato Y, Ohfuji S, Okuyama H (2015) Outcome in VLBW infants with surgical intestinal disorder at 18 months of corrected age. Pediatrics international : official journal of the Japan Pediatric Society 57:633–638
Lodha A, Asztalos E, Moore AM (2010) Cytokine levels in neonatal necrotizing enterocolitis and long-term growth and neurodevelopment. Acta paediatrica (Oslo, Norway : 1992) 99:338–343
Tseng WL, Chen CH, Chang JH, Peng CC, Jim WT, Lin CY, Hsu CH, Liu TY, Chang HY, On Behalf Of The Taiwan Premature Infant Follow-Up N (2023) Risk factors of language delay at two years of corrected age among very-low-birth-weight preterm infants: a population-based study. Children (Basel) 10
Yeh TC, Chang JH, Kao HA, Hsu CH, Hung HY, Peng CC (2004) Necrotizing enterocolitis in infants: clinical outcome and influence on growth and neurodevelopment. J Formos Med Assoc 103:761–766
Bassler D, Stoll BJ, Schmidt B, Asztalos EV, Roberts RS, Robertson CMT, Sauve RS (2009) Using a count of neonatal morbidities to predict poor outcome in extremely low birth weight infants: Added role of neonatal infection. Pediatrics 123:313–318
Pike K, Brocklehurst P, Jones D, Kenyon S, Salt A, Taylor D, Marlow N (2012) Outcomes at 7 years for babies who developed neonatal necrotising enterocolitis: the ORACLE Children Study. Arch Dis Child Fetal Neonatal Ed 97:F318-322
Shin SH, Kim EK, Kim SH, Kim HY, Kim HS (2021) Head growth and neurodevelopment of preterm infants with surgical necrotizing enterocolitis and spontaneous intestinal perforation. Children (Basel) 8
Brunse A, Abbaspour A, Sangild PT (2018) Brain barrier disruption and region-specific neuronal degeneration during necrotizing enterocolitis in preterm pigs. Dev Neurosci 40:198–208
Biouss G, Antounians L, Li B, O’Connell JS, Seo S, Catania VD, Guadagno J, Rahman A, Zani-Ruttenstock E, Svergun N, Pierro A, Zani A (2019) Experimental necrotizing enterocolitis induces neuroinflammation in the neonatal brain. J Neuroinflammation 16:97
Niño DF, Zhou Q, Yamaguchi Y, Martin LY, Wang S, Fulton WB, Jia H, Lu P, Prindle T, Jr., Zhang F, Crawford J, Hou Z, Mori S, Chen LL, Guajardo A, Fatemi A, Pletnikov M, Kannan RM, Kannan S, Sodhi CP, Hackam DJ (2018) Cognitive impairments induced by necrotizing enterocolitis can be prevented by inhibiting microglial activation in mouse brain. Sci Transl Med 10
Zhou Q, Niño DF, Yamaguchi Y, Wang S, Fulton WB, Jia H, Lu P, Prindle T, Jr., Pamies D, Morris M, Chen LL, Sodhi CP, Hackam DJ (2021) Necrotizing enterocolitis induces T lymphocyte-mediated injury in the developing mammalian brain. Sci Transl Med 13
Kuik SJ, den Heijer AE, Mebius MJ, Hulscher JBF, Bos AF, Kooi EMW (2020) Time to full enteral feeding after necrotizing enterocolitis in preterm-born children is related to neurodevelopment at 2–3 years of age. Early Hum Dev 147:105091
Acknowledgements
We would like to thank Zhao Ningyuan for figure editing.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection was performed by HL and HT. Data analysis was performed by LSL and WY. The first draft of the manuscript was written by WY and LMZ, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Y., Liu, S., Lu, M. et al. Neurodevelopmental outcomes of preterm with necrotizing enterocolitis: a systematic review and meta-analysis. Eur J Pediatr 183, 3147–3158 (2024). https://doi.org/10.1007/s00431-024-05569-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-024-05569-5