Abstract
High concentrations of oxygen are often needed to optimize oxygenation in infants with persistent pulmonary hypertension (PPHN), but this can also increase the risk of hyperoxemia. We determined the occurrence of hyperoxemia in infants treated for PPHN. Medical records of infants ≥ 34 + 0 weeks gestational age (GA) who received inhaled nitric oxide (iNO) were retrospectively reviewed for oxygenation parameters during iNO therapy. Oxygen was manually titrated to target arterial oxygen tension (PaO2) 10–13 kPa and peripheral oxygen saturation (SpO2) 92–98%. The main study outcomes were the incidence and duration of hyperoxemia and hypoxemia and the fraction of inspired oxygen (FiO2). A total of 181 infants were included. The median FiO2 was 0.43 (IQR 0.34–0.56) and the maximum FiO2 was 1.0 in 156/181 (86%) infants, resulting in at least one PaO2 > 13 kPa in 149/181 (82%) infants, of which 46/149 (31%) infants had minimal one PaO2 > 30 kPa. SpO2 was > 98% in 179/181 (99%) infants for 17.7% (8.2–35.6%) of the iNO time. PaO2 < 10 kPa occurred in 160/181 (88%) infants, of which 81/160 (51%) infants had minimal one PaO2 < 6.7 kPa. SpO2 was < 92% in 169/181 (93%) infants for 1.6% (0.5–4.3%) of the iNO time.
Conclusion: While treatment of PPHN is focused on preventing and reversing hypoxemia, hyperoxemia occurs inadvertently in most patients.
What is Known: • High concentrations of oxygen are often needed to prevent hypoxemia-induced deterioration of PPHN, but this can also increase the risk of hyperoxemia. • Infants with persistent pulmonary hypertension may be particularly vulnerable to the toxic effects of oxygen, and hyperoxemia could further induce pulmonary vasoconstriction, potentially worsening the condition. | |
What is New: • Hyperoxemia occurs in the majority of infants with PPHN during treatment with iNO. • Infants with PPHN spent a considerably longer period with saturations above the target range compared to saturations below the target range. |
Similar content being viewed by others
Introduction
Persistent pulmonary hypertension of the newborn (PPHN) is a complication during neonatal transition characterized by a sustained elevation in pulmonary vascular resistance (PVR). The incidence of PPHN is approximately 2 per 1000 live births in late preterm and term neonates [1]. Despite appropriate therapy, PPHN is associated with a mortality rate of 10% and significant neurodevelopmental, cognitive, and hearing disabilities among survivors [1,2,3,4,5].
PPHN is secondary to a number of underlying causes associated with impaired relaxation of the pulmonary vasculature, such as perinatal asphyxia, infection, and meconium aspiration syndrome (MAS) [6,7,8]. Elevated PVR leads to decreased pulmonary blood flow (PBF), resulting in hypoxemia and acidosis. In turn, hypoxemia and acidosis cause the pulmonary vessels to constrict, thereby worsening the PPHN [8].
Postnatal increase in oxygen tension in the lungs is one of the most crucial factors to promote pulmonary vasodilatation [9]. Therefore, supplemental oxygen therapy is the mainstay in the treatment of PPHN to reduce PVR and increase oxygenation [6,7,8]. Inhaled nitric oxide (iNO) is a selective pulmonary vasodilator and is considered the first-line PPHN-specific therapy when oxygen therapy alone is insufficient to reduce PVR [6, 8].
High concentrations of oxygen are often needed to prevent hypoxemia-induced deterioration of PPHN, but this can also increase the risk of hyperoxemia, especially when the infant stabilizes, and PVR reduces. However, titrating oxygen therapy within the narrow therapeutic range is difficult in infants with PPHN. Infants with PPHN often experience respiratory and hemodynamic instability, which warrants caution regarding weaning off oxygen therapy.
As a result, infants with PPHN may unintentionally face an increased risk of hyperoxemia, which can cause organ injury [10]. Avoiding hyperoxemia is potentially especially relevant in the context of PPHN, as it can directly promote pulmonary vasoconstriction, further worsening the PPHN [11]. Previous translational studies have shown that there is a certain “oxygenation threshold” above which pulmonary vasodilatation is no longer enhanced and subsequent response to iNO therapy is impaired [12,13,14,15]. Moreover, reoxygenation after a period of hypoxemia may amplify or even directly cause organ injury, rendering infants with PPHN, especially those associated with perinatal asphyxia, particularly susceptible to hyperoxemia [16]. In line with this, Kilmartin et al. showed that PPHN increased the risk of death and brain injury in infants with perinatal asphyxia [17].
There is no data available regarding how often hyperoxemia occurs during PPHN treatment in infants. Therefore, we performed a retrospective cohort study to determine the occurrence of hyperoxemia in late preterm and term infants treated for PPHN.
Methods
A retrospective study was performed including late preterm and term infants (≥ 34 + 0 weeks) admitted to the Neonatal Intensive Care Unit (NICU) at Leiden University Medical Center (LUMC) who received iNO therapy between November 2011 and June 2023. As this study aims to investigate the association between PPHN therapy and hyperoxemia, echocardiographic confirmation of PPHN was not considered an inclusion criterion. Exclusion criteria were as follows: iNO therapy initiated > 48 h after birth, < 2 arterial blood gasses during iNO therapy, death < 12 h after birth, and congenital malformations that affected the ability to adequately oxygenate (e.g., cyanotic congenital heart defects and lung hypoplasia).
According to the protocol of the respective NICU, iNO therapy (PrinterNOx, CareFusion UK 232 Ltd., Kent, UK) is indicated for infants with an arterial oxygen tension (PaO2) < 13.3 kPa (100 mmHg) at a fraction of inspired oxygen (FiO2) 1.0. iNO is started at a dose of 20 parts per million (ppm). If oxygenation improves, iNO is gradually reduced at the discretion of the respective neonatologist in decrements of 50% until 5 ppm; then, further weaning is done at a rate of 1 ppm per hour. iNO is administered through conventional or high-frequency oscillation (HFO) ventilation, with peripheral oxygen saturation (SpO2) limits set at 92–98% for the cardiorespiratory monitor. PaO2 and arterial carbon dioxide tension (PaCO2) targets are 10–13 kPa (75–98 mmHg) and 5–6 kPa (38–45 mmHg), respectively. Automated oxygen control is not used in PPHN. In case of inadequate improvement, sildenafil can be considered. Extracorporeal membrane oxygenation (ECMO) is used as a rescue treatment.
All study data were retrieved from two digital medical record databases (Healthcare Information X-change (HIX), Chipsoft B.V., Amsterdam, The Netherlands, and PDMS; MetaVision iMDsoft, Leiden, The Netherlands). Baseline characteristics were determined, including maternal and patient demographics, pathology underlying PPHN (categorized according to the criteria summarized in Online Resource 1), mode of ventilation, hospital course including therapeutic interventions other than oxygen and iNO, and mortality. During iNO therapy, PaO2 in arterial blood gasses (RapidPoint500, Siemens Healthcare, UK) were collected, as well as one-per-minute data of pre- and postductal SpO2 in pulse oximetry and FiO2. The study period varies among infants due to differences in iNO therapy duration. If an infant was transferred for ECMO, the study period was ended.
The primary study outcomes were the incidence and duration of hyperoxemia during iNO therapy, defined as a PaO2 > 13 kPa (98 mmHg) or SpO2 > 98%. Secondary outcomes included the incidence and duration of hypoxemia, defined as a PaO2 < 10 kPa (75 mmHg) or SpO2 < 92%, and the concentration and duration of oxygen therapy. The definitions for hyperoxemia and hypoxemia are based on the oxygenation target ranges for PPHN used in our NICU. Severe hyperoxemia was defined as PaO2 > 30 kPa (225 mmHg) as it has been associated with an increased risk of death or adverse neurodevelopmental outcome in asphyxiated infants [18]. Severe hypoxemia was defined as a PaO2 < 6.7 kPa (50 mmHg) or SpO2 < 80% as per previous studies [19, 20]. The incidences of hyperoxemia and hypoxemia were derived from collected PaO2 measurements, while the durations of hyperoxemia and hypoxemia were derived from one-per-minute SpO2 measurements.
Due to the retrospective design of the study, a convenience sample was used. Data analysis was performed using SPSS 29 (IBM SPSS Statistics). Parameters were checked for normality through visual inspection of histograms. As this observational study intends to describe oxygenation parameters during PPHN therapy, outcomes have not been tested for statistical significance. Results are presented as n (% of N) for categorical variables and mean ± SD or median (IQR) for continuous parameters.
Results
Between 2011 and 2023, 280 late preterm and term infants received iNO therapy in the NICU, of which 99 were excluded according to predefined criteria: 18 received iNO therapy > 48 h after birth, 9 had < 2 arterial oxygen tension measurements, 4 deceased < 12 h after birth, and 68 suffered from a congenital malformation that impaired adequate oxygenation. Thus, a total of 181 infants were included in the study (Fig. 1), with GA 40 (38–40) weeks and birth weight of 3366 ± 677 g (Table 1). The median duration of iNO therapy (study period) was 2.4 (1.5–3.6) days, with a range of 0.3 to 13.8 days. The median number of PaO2 samples per infant was 13 (8–19).
Oxygen therapy
The median duration of oxygen therapy (FiO2 > 0.21) was 49 (25–83) h, constituting 97.6% (77.6–100%) of the iNO time. FiO2 was 1.0 in 156/181 (86%) infants for a duration of 2.2 (0.3–8.0) h per infant, representing 3.7% (0.6–13.5%) of the iNO time. The median FiO2 supply per infant was 0.43 (0.34–0.56).
Hyperoxemia
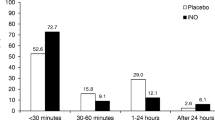
In 149/181 (82%) infants, at least one PaO2 measurement > 13 kPa was observed and severe hyperoxemia (PaO2 > 30 kPa) occurred in 46/181 (25%) infants (Fig. 2). The maximum PaO2 during iNO therapy was 21.6 (15.4–30.3) kPa, with a range of 5.6–59.7 kPa. In 179/181 (99%) infants, SpO2 > 98% was observed for 17.7% (8.2–35.6%) of the iNO time (Fig. 2).
Oxygenation parameters outside the target range. a Proportion of infants (N = 181) with at least one PaO2 outside the target range during iNO therapy. b Proportion of iNO time with a SpO2 outside the target range. Values are presented as median (IQR). PaO2, arterial oxygen tension; SpO2, oxygen saturation (pulse oximetry); iNO, inhaled nitric oxide
Hypoxemia
Of the 181 infants, 160 (88%) infants had at least one PaO2 measurement < 10 kPa, and severe hypoxemia (PaO2 < 6.7 kPa) was observed in 81/181 (45%) infants (Fig. 2). The minimum PaO2 during iNO therapy was 6.9 (5.6–8.5) kPa, with a range of 1.4 and 22.5 kPa. In 169/181 (93%) infants, SpO2 < 92% was observed for 1.6% (0.5–4.3%) of the iNO time, and severe hypoxemia (SpO2 < 80%) occurred in 93/181 (51%) infants for 0.02% (0.00–0.22%) of the iNO time (Fig. 2).
Discussion
In this study, we demonstrated for the first time that hyperoxemia occurs often in late preterm and term infants treated for PPHN.
A previous retrospective study by Solberg et al. in mechanically ventilated infants, irrespective of PPHN, showed that 36% of term infants with measurements of arterial blood gasses had at least one hyperoxemic PaO2 within 48 h, compared to 82% of the infants during treatment for PPHN in the present study [21]. Infants with PPHN constitute a subgroup of ventilated infants with an increased risk of hyperoxemia due to their high oxygen requirement, as observed in our current study in which most infants received maximum FiO2 for a considerable period of time. In line with this, the median FiO2 was higher than in the study of Solberg et al. (0.43 vs. 0.21) [21].
Remarkedly however, despite the high concentrations of oxygen therapy, the occurrence of hypoxemia was similar to that of hyperoxemia, and severe hyperoxemia (PaO2 < 6.7 kPa) was observed in almost half of the infants. In the acute phase, infants with PPHN typically present with severe hypoxemia, and may remain cyanotic even when exposed to a high oxygen concentration [7]. After stabilization, the infants remain labile, with even small changes causing acute pulmonary vasoconstriction and rapid clinical decompensation [22]. As a result, neonatologists are cautious in weaning FiO2, which increases the risk of hyperoxemia. In line with this, we found longer time periods of SpO2 > 98% compared to SpO2 < 92% within this study, indicating that the neonatologists were attentive in preventing hypoxemia but were permissive of hyperoxemia. These findings are consistent with a previous survey among 492 neonatologists in the USA that evaluated oxygen management in infants with PPHN [23]. The survey demonstrated that a significant number of neonatologists preferred to target higher SpO2 and/or PaO2 to avoid hypoxemia but did not use an upper limit of SpO2 and PaO2 to prevent hyperoxemia. Furthermore, a small but notable portion of neonatologists (6%) opted to administer 100% oxygen, irrespective of the oxygenation parameters, until they were confident that the infant had clinically stabilized [23]. The permissive attitude towards hyperoxemia is also reflected by the current significant variations in practice with respect to oxygen titration strategies and the lack of evidence-based guidelines for oxygen weaning in the management of PPHN [23, 24]. Of the 492 neonatologists from the survey, 72% did not use specific oxygen titration guidelines [23]. In line with this, in our NICU, oxygen titration is left to the discretion of the respective neonatologist. Based on the clinical perceptions of the neonatologists in this study, despite the protocol’s recommendation to avoid hyperoxemia in PPHN, it is hypothesized that titration of oxygen is initiated once PaO2 values are > 13 kPa to reduce the risk of rebound PPHN. However, the clinical tolerance towards hyperoxemia is challengeable in infants with PPHN as hyperoxemia can promote pulmonary vasoconstriction and add to organ injury due to reoxygenation after an hypoxemic episode. Considering the high incidence of hyperoxemia in infants with PPHN, evaluation of the risks of hyperoxemia in infants with PPHN is warranted.
In addition, re-assessment of current strategies for oxygen therapy is needed to improve the time of having oxygenation parameters within the target range in infants with PPHN. The use of standardized protocols or innovations such as automated oxygen control [25] has the potential to improve oxygen titration, but more data is required to investigate its application in infants with PPHN.
An important consideration in optimizing oxygen titration in infants with PPHN is that SpO2 may not accurately reflect the arterial oxygen saturation due to underlying pathologies and therapies that compromise the peripheral circulation (e.g., asphyxia, inotropic agents) and shift the oxygen-hemoglobin dissociation curve (e.g., hypothermia) [26, 27]. An alternative titration parameter could be transcutaneous oxygen tension (TcPO2) [28], but its accuracy in infants with PPHN requires more research. Furthermore, the optimal SpO2 and PaO2 ranges in the management of PPHN are unknown. Based on translational studies, it is recommended to maintain SpO2 in the low to mid-90s and PaO2 between 55 and 80 mmHg (7.3–10.7 kPa) [8, 11]. However, clinical studies comparing different oxygenation targets are lacking.
This study has several limitations due to its retrospective design. In infants with PPHN, preductal PaO2 and SpO2 are typically higher compared to postductal values through right-to-left shunting over the ductus arteriosus [8]. Therefore, the probability of a hyperoxic PaO2 and SpO2 is higher in preductal than postductal measurements. This study was not able to differentiate between pre- and postductal PaO2 and SpO2, which may have led to an underestimation of the occurrence of hyperoxemia. However, this would only emphasize the need to improve oxygen weaning in PPHN.
Moreover, it was not possible to compare the occurrence and duration of hyperoxemia and hypoxemia based on PaO2 due to sampling bias: the decision to sample an arterial blood gas depends on the clinical condition of the infant. During a period of hypoxemia or hyperoxemia, the number of PaO2 samples will be increased to closely monitor the infant, resulting in an increase in the occurrence of hypoxemia or hyperoxemia. Similarly, a higher number of PaO2 samples result in a more adequate estimation of the duration of hyperoxemia and hypoxemia. However, we were able to estimate the duration of hyperoxemia and hypoxemia in terms of SpO2, which is the most commonly used parameter to titrate oxygen in PPHN [23].
Furthermore, considering the wide variety in the management of PPHN [23], in particular the variation in oxygenation target ranges, the external validity of the study may be limited by its single-center design. However, the majority of neonatologists are tolerant towards hyperoxemia [23], suggesting that the trend of high occurrence of hyperoxemia demonstrated in this study may be generalizable to a broader population. Lastly, although the data collection over 11 years significantly increased the number of infants included in the study, variations in clinical practice may have occurred, resulting in a historical bias.
In conclusion, while there is an increasing awareness of oxygen toxicity, the management of PPHN remains focused on reversing hypoxemia by means of high concentrations of oxygen. As a result, hyperoxemia occurs often during manual oxygen therapy in late preterm and term infants treated for PPHN. These findings warrant clinical awareness regarding the high risk for hyperoxemia in infants with PPHN. Further research is required to improve current strategies of oxygen therapy in these infants.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to patient privacy, but are available from the corresponding author upon reasonable request.
Abbreviations
- ECMO:
-
Extracorporeal membrane oxygenation
- FiO2 :
-
Fraction of inspired oxygen
- GA:
-
Gestational age
- HFO:
-
High-frequency oscillation
- iNO:
-
Inhaled nitric oxide
- LUMC:
-
Leiden University Medical Center
- MAS:
-
Meconium aspiration syndrome
- NICU:
-
Neonatal intensive care unit
- PaCO2 :
-
Arterial carbon dioxide tension
- PaO2 :
-
Arterial oxygen tension
- PBF:
-
Pulmonary blood flow
- PPHN:
-
Persistent pulmonary hypertension of the newborn
- PPM:
-
Parts per million
- PVR:
-
Pulmonary vascular resistance
- SpO2 :
-
Peripheral oxygen saturation
- TcPO2 :
-
Transcutaneous oxygen tension
References
Walsh-Sukys MC, Tyson JE, Wright LL et al (2000) Persistent pulmonary hypertension of the newborn in the era before nitric oxide: practice variation and outcomes. Pediatrics 105:14–20. https://doi.org/10.1542/PEDS.105.1.14
Konduri GG, Vohr B, Robertson C et al (2007) Early inhaled nitric oxide therapy for term and near-term newborn infants with hypoxic respiratory failure: neurodevelopmental follow-up. J Pediatr 150:235–240. https://doi.org/10.1016/J.JPEDS.2006.11.065
Finer N (2000) Inhaled nitric oxide in term and near-term infants: neurodevelopmental follow-up of The Neonatal Inhaled Nitric Oxide Study Group (NINOS). J Pediatr 136:611–617. https://doi.org/10.1067/mpd.2000.104826
Clark RH, Huckaby JL, Kueser TJ et al (2003) Low-dose nitric oxide therapy for persistent pulmonary hypertension: 1-year follow-up. J Perinatol 23:300–303. https://doi.org/10.1038/SJ.JP.7210908
Lipkin PH, Davidson D, Spivak L et al (2002) Neurodevelopmental and medical outcomes of persistent pulmonary hypertension in term newborns treated with nitric oxide. J Pediatr 140:306–310. https://doi.org/10.1067/mpd.2002.122730
Ball MK, Seabrook RB, Bonachea EM et al (2022) Evidence-based guidelines for acute stabilization and management of neonates with persistent pulmonary hypertension of the newborn. Am J Perinatol 40:1495–1508. https://doi.org/10.1055/A-1711-0778
Bendapudi P, Rao GG, Greenough A (2015) Diagnosis and management of persistent pulmonary hypertension of the newborn. Paediatr Respir Rev 16:157–161. https://doi.org/10.1016/J.PRRV.2015.02.001
Singh Y, Lakshminrusimha S (2021) Pathophysiology and management of persistent pulmonary hypertension of the newborn. Clin Perinatol 48:595–618. https://doi.org/10.1016/J.CLP.2021.05.009
Teitel DF, Iwamoto HS, Rudolph AM (1990) Changes in the pulmonary circulation during birth-related events. Pediatr Res 27:372–378. https://doi.org/10.1203/00006450-199004000-00010
Saugstad OD (2012) Hyperoxia in the term newborn: more evidence is still needed for optimal oxygen therapy. Acta Paediatr 101:34–38. https://doi.org/10.1111/J.1651-2227.2011.02546.X
Rawat M, Lakshminrusimha S, Vento M (2022) Pulmonary hypertension and oxidative stress: where is the link? Semin Fetal Neonatal Med 27:101347. https://doi.org/10.1016/J.SINY.2022.101347
Lakshminrusimha S, Swartz DD, Gugino SF et al (2009) Oxygen concentration and pulmonary hemodynamics in newborn lambs with pulmonary hypertension. Pediatr Res 66:539–544. https://doi.org/10.1203/PDR.0B013E3181BAB0C7
Rudolph AM, Yuan S (1966) Response of the pulmonary vasculature to hypoxia and H+ ion concentration changes. J Clin Invest 45:399–411. https://doi.org/10.1172/JCI105355
Lakshminrusimha S, Russell JA, Steinhorn RH et al (2007) Pulmonary hemodynamics in neonatal lambs resuscitated with 21%, 50%, and 100% oxygen. Pediatr Res 62:313–318. https://doi.org/10.1203/PDR.0B013E3180DB29FE
Lakshminrusimha S, Steinhorn RH, Wedgwood S et al (1985) (2011) Pulmonary hemodynamics and vascular reactivity in asphyxiated term lambs resuscitated with 21 and 100% oxygen. J Appl Physiol 111:1441–1447. https://doi.org/10.1152/JAPPLPHYSIOL.00711.2011
Fellman V, Raivio KO (1997) Reperfusion injury as the mechanism of brain damage after perinatal asphyxia. Pediatr Res 41:599–606. https://doi.org/10.1203/00006450-199705000-00001
Kilmartin KC, Al Balushi A, Altit G et al (2023) Impact of persistent pulmonary hypertension and oxygenation on brain injury in neonates with neonatal encephalopathy treated with therapeutic hypothermia. J Perinatol. https://doi.org/10.1038/s41372-023-01805-2
Klinger G, Beyene J, Shah P, Perlman M (2005) Do hyperoxaemia and hypocapnia add to the risk of brain injury after intrapartum asphyxia? Arch Dis Child Fetal Neonatal Ed 90:49–52. https://doi.org/10.1136/adc.2003.048785
Mitra S, Singh B, El-Naggar W, McMillan DD (2018) Automated versus manual control of inspired oxygen to target oxygen saturation in preterm infants: a systematic review and meta-analysis. J Perinatol 38:351–360. https://doi.org/10.1038/s41372-017-0037-z
Kelly R, Quine D, Stenson BJ (2023) Exploring the risk of hyperoxia in oxygen-dependent very low birthweight infants in the first week of life to plan future trials of oxygen targeting. Arch Dis Child Fetal Neonatal Ed 108:434–435. https://doi.org/10.1136/ARCHDISCHILD-2022-324717
Solberg MT, Bjørk IT, Hansen TWR (2013) Adherence to oxygenation and ventilation targets in mechanically ventilated premature and sick newborns: a retrospective study. BMC Pediatr 13:126. https://doi.org/10.1186/1471-2431-13-126
Mandell E, Kinsella JP, Abman SH (2021) Persistent pulmonary hypertension of the newborn. Pediatr Pulmonol 56:661–669. https://doi.org/10.1002/ppul.25073
Alapati D, Jassar R, Shaffer TH (2017) Management of supplemental oxygen for infants with persistent pulmonary hypertension of newborn: a survey. Am J Perinatol 34:276–282. https://doi.org/10.1055/S-0036-1586754
Nakwan N, Chaiwiriyawong P (2016) An international survey on persistent pulmonary hypertension of the newborn: a need for an evidence-based management. J Neonatal Perinatal Med 9:243–250. https://doi.org/10.3233/NPM-16915133
Kaltsogianni O, Dassios T, Lee R et al (2023) Closed-loop automated oxygen control in ventilated infants born at or near term: a crossover trial. Acta Paediatr 112:246–251. https://doi.org/10.1111/APA.16598
Chan ED, Chan MM, Chan MM (2013) Pulse oximetry: understanding its basic principles facilitates appreciation of its limitations. Respir Med 107:789–799. https://doi.org/10.1016/J.RMED.2013.02.004
Chandrasekharan P, Rawat M, Lakshminrusimha S (2020) How do we monitor oxygenation during the management of PPHN? Alveolar, arterial, mixed venous oxygen tension or peripheral saturation? Children (Basel) 7:180. https://doi.org/10.3390/CHILDREN7100180
Quine D, Stenson BJ (2008) Does the monitoring method influence stability of oxygenation in preterm infants? A randomised crossover study of saturation versus transcutaneous monitoring. Arch Dis Child Fetal Neonatal Ed 93:347–350. https://doi.org/10.1136/ADC.2007.132282
Author information
Authors and Affiliations
Contributions
Justine de Jager, Fleur Brouwer, Jeroen Reijman, Roel L. F. van der Palen, Arjan B. te Pas, and Janneke Dekker contributed to the study conception and design. Data collection, analysis, and interpretation were performed by Justine de Jager, Fleur Brouwer, Jeroen Reijman, and Janneke Dekker. The first draft of the manuscript was written by Justine de Jager and all authors revised it critically for important intellectual content. All authors approved the final version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Because of the observational nature, this study did not require adherence to the Dutch law on Medical Research in Humans. Therefore, patient consent was not necessary. The Research Ethics Committee Leiden-Den Haag-Delft provided a statement of no objection for performing this study.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Jager, J., Brouwer, F., Reijman, J. et al. Occurrence of hyperoxia during iNO treatment for persistent pulmonary hypertension of the newborn: a cohort study. Eur J Pediatr 183, 2455–2461 (2024). https://doi.org/10.1007/s00431-024-05506-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-024-05506-6