Abstract
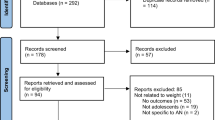
Hospital admissions for eating disorders (ED) are rapidly increasing. Limited research exists evidencing the factors that lead to hospital admissions or their outcomes. The current study aimed to identify predictors of hospital admission in adolescents with anorexia nervosa (AN) or atypical anorexia nervosa (AAN). Prospective observational study including participants (n = 205) aged 11–18 and diagnosed with AN or AAN at initial ED assessment, across eight London clinics. Physical health parameters at assessment, including heart rate, blood pressure, temperature and rate of weight loss, were compared between adolescents who were admitted to a paediatric ward following assessment and those who were not admitted. The mean rate of weight loss prior to assessment was significantly higher, and mean energy intake significantly lower, in the admitted vs not admitted groups (1.2 vs 0.6kg/week, p < 0.001 and 565 kcal/day vs 857 kcal/day, p < 0.001), independent of degree of underweight. No significant differences were identified between groups in all other parameters of physical risk. Underweight adolescents with AN were equally likely to be admitted as non-underweight adolescents with AAN.
Conclusion: This study provides evidence on predictors of hospital admission, from a sample representing the London area. The assessment of weight loss speed, duration and magnitude are recommended as priority parameters that inform the risk of deterioration and the likelihood of hospital admission in adolescent AN and AAN. Further research investigating outcomes of these hospital admission is needed.
What is Known: • Hospital admissions for eating disorders (ED) are rapidly increasing. • Limited research exists evidencing the factors that lead to hospital admissions, or their outcomes. | |
What is New: • This study provides evidence on predictors of hospital admission in young people with typical and atypical anorexia nervosa. • Weight loss speed, duration, and magnitude are recommended as priority parameters that inform the risk of deterioration and the likelihood of hospital admission in this patient group. |

Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author, CB.
Abbreviations
- AN:
-
Anorexia nervosa
- AAN:
-
Atypical anorexia nervosa
- ANOVA:
-
Analysis of variance
- ED:
-
Eating disorders
- NHS:
-
National Health Service
- MDT:
-
Multidisciplinary team
- MEED:
-
Medical of Emergencies in Eating Disorders
- NICE:
-
National Institute for Clinical and care Excellence
- %mBMI:
-
Percentage median body mass index
References
NHS Digital (2021) Hospital admissions for eating disorders. Supplementary Information. Published 2021. https://digital.nhs.uk/supplementary-information/2021/hospital-admissions-for-eating-disorders-2015-2021
Gilsbach S, Plana MT, Castro-Fornieles J et al (2022) Increase in admission rates and symptom severity of childhood and adolescent anorexia nervosa in Europe during the COVID-19 pandemic: data from specialized eating disorder units in different European countries. Child Adolesc Ment Health 16(1):1–7. https://doi.org/10.1186/s13034-022-00482-x
Hartman-Munick SM, Lin JA, Milliren CE et al (2022) Association of the COVID-19 pandemic with adolescent and young adult eating disorder care volume. JAMA Pediatr 176(12):1225–1232. https://doi.org/10.1001/jamapediatrics.2022.4346
Khalifa I, Goldman RD (2019) Anorexia nervosa requiring admission in adolescents. Can Fam Physician 65(2):107–108
Royal College of Psychiatrists (2022) Medical Emergencies in Eating Disorders (MEED) Guidance on recognition and management 185. https://www.rcpsych.ac.uk/docs/default-source/improving-care/better-mh-policy/college-reports/college-report-cr233-medical-emergencies-in-eating-disorders-(meed)-guidance.pdf?sfvrsn=2d327483_50
Brennan C, Illingworth S, Cini E, Bhakta D (2023) Medical instability in typical and atypical adolescent anorexia nervosa: a systematic review and meta-analysis. J Eat Disord 11(1):1–13. https://doi.org/10.1186/s40337-023-00779-y
Garber AK, Cheng J, Accurso EC et al (2019) Weight loss and illness severity in adolescents with atypical anorexia nervosa. Pediatrics 144(6). https://doi.org/10.1542/peds.2019-2339
Whitelaw M, Lee KJ, Gilbertson H, Sawyer SM (2018) Predictors of complications in anorexia nervosa and atypical anorexia nervosa: degree of underweight or extent and recency of weight loss? J Adolesc Heal 63(6):717–723. https://doi.org/10.1016/j.jadohealth.2018.08.019
The Royal Colleges of Psychiatrists (2022) Hospital admissions for eating disorders increased by 84% in the last five years. News and Features. Published 2022. https://www.rcpsych.ac.uk/news-and-features/latest-news/detail/2022/05/18/hospital-admissions-for-eating-disorders-increased-by-84-in-the-last-five-years
Schwartz BI, Mansbach JM, Marion JG, Katzman DK, Forman SF (2008) Variations in admission practices for adolescents with anorexia nervosa: a North American sample. J Adolesc Heal 43(5):425–431. https://doi.org/10.1016/j.jadohealth.2008.04.010
Chidiac CW (2019) An update on the medical consequences of anorexia nervosa. Curr Opin Pediatr 31(4):448–453. https://doi.org/10.1097/MOP.0000000000000755
Golden NH, Katzman DK, Sawyer SM et al (2015) Update on the medical management of eating disorders in adolescents. J Adolesc Heal 56(4):370–375. https://doi.org/10.1016/j.jadohealth.2014.11.020
Hudson LD, Nicholls DE, Lynn RM, Viner RM (2012) Medical instability and growth of children and adolescents with early onset eating disorders. Arch Dis Child 97(9):779–784. https://doi.org/10.1136/archdischild-2011-301055
Bako A, Yeo M, Sawyer SM, Hughes E (2019) How low can you go? The significance of bradycardia for acute clinical outcomes in hospitalised adolescents with anorexia nervosa. J Adolesc Heal 64(2):S52. https://doi.org/10.1016/j.jadohealth.2018.10.114
Golden NH, Keane-Miller C, Sainani KL, Kapphahn CJ (2013) Higher caloric intake in hospitalized adolescents with anorexia nervosa is associated with reduced length of stay and no increased rate of refeeding syndrome. J Adolesc Heal 53(5):573–578. https://doi.org/10.1016/j.jadohealth.2013.05.014
Walsh BT, Hagan KE, Lockwood C (2022) A systematic review comparing atypical anorexia nervosa and anorexia nervosa. Int J Eat Disord. https://doi.org/10.1002/eat.23856
Freizinger M, Recto M, Jhe G, Lin J (2022) Atypical anorexia in youth: cautiously bridging the treatment gap. Children 9(6):1–13. https://doi.org/10.3390/children9060837
Kennedy GA, Forman SF, Woods ER et al (2017) History of overweight/obesity as predictor of care received at 1-year follow-up in adolescents with anorexia nervosa or atypical anorexia nervosa. J Adolesc Heal 60(6):674–679. https://doi.org/10.1016/j.jadohealth.2017.01.001
Lebow J, Sim LA, Kransdorf LN (2015) Prevalence of a history of overweight and obesity in adolescents with restrictive eating disorders. J Adolesc Heal 56(1):19–24. https://doi.org/10.1016/j.jadohealth.2014.06.005
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders (4th Ed., Text Revision). 4th ed
Moskowitz L, Weiselberg E (2017) Anorexia nervosa/atypical anorexia nervosa. Curr Probl Pediatr Adolesc Health Care 47(4):70–84. https://doi.org/10.1016/j.cppeds.2017.02.003
Vo M, Golden N (2022) Medical complications and management of atypical anorexia nervosa. J Eat Disord 10(1):4–9. https://doi.org/10.1186/s40337-022-00720-9
Sawyer SM, Whitelaw M, Le Grange D, Yeo M, Hughes EK (2016) Physical and psychological morbidity in adolescents with atypical anorexia nervosa. Pediatrics 137(4). https://doi.org/10.1542/peds.2015-4080
Bailey AP, Parker AG, Colautti LA, Hart LM, Liu P, Hetrick SE (2014) Mapping the evidence for the prevention and treatment of eating disorders in young people. J Eat Disord 2(1):1–12. https://doi.org/10.1186/2050-2974-2-5
Eisler I, Simic M, Blessitt E, Dodge L (2016) Maudsley Service Manual for Child and Adolescent Eating Disorders
Fink K, Rhodes P, Miskovic-Wheatley J et al (2017) Exploring the effects of a family admissions program for adolescents with anorexia nervosa. J Eat Disord 5(1):1–10. https://doi.org/10.1186/s40337-017-0181-z
Freizinger M, Jhe G, Pluhar E, Mancini L (2021) Integrating family-based treatment principles in the acute inpatient treatment of adolescents with restrictive eating disorders. Psychol Res Behav Manag 14:449–454. https://doi.org/10.2147/PRBM.S304921
Matthews A, Peterson CM, Peugh J, Mitan L (2019) An intensive family-based treatment guided intervention for medically hospitalized youth with anorexia nervosa: parental self-efficacy and weight-related outcomes. Eur Eat Disord Rev 27(1):67–75. https://doi.org/10.1002/erv.2632
National Insititute of Health and Care Excellence (2017) NICE Guideline (NG69) eating disorders: recognition and treatment treatment
Schoenwald S, Sheidow A, Letourneau E (2004) Toward effective quality assurance in evidence-based practice: links between expert consultation, therapist fidelity, and child outcomes. J Clin Child Adolesc Psychol 33(1):94–104
Acknowledgements
We acknowledge Suzy Oakley, Annie Stevenson, Ellie Bishop, Jessica Polykarpou and Eloise Saglio for their support with the study.
Author information
Authors and Affiliations
Contributions
CB was responsible for conception and design of the study, recruitment of participants, data collection and analysis and preparation of drafts and final versions of the manuscript and associated tables and documents. DB contributed to the conception, design, and supervision of the study, and editing of the draft and final manuscript and tables. MS, SI, EC, SC, DN and VC contributed to the design and supervision of the study, and the editing of the final manuscript. CS, EH, SF, JO, NC, TB and EA were responsible for the recruitment of participants, collection of study data and editing the final draft of the manuscript. Cliona Brennan wrote the first draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brennan, C., Cini, E., Illingworth, S. et al. Greater rate of weight loss predicts paediatric hospital admission in adolescent typical and atypical anorexia nervosa. Eur J Pediatr 183, 1789–1799 (2024). https://doi.org/10.1007/s00431-024-05436-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-024-05436-3