Abstract
The Cow’s Milk-related Symptom Score (CoMiSS) is an awareness tool for evaluating cow’s milk-related symptoms. Previous studies have focused on providing CoMiSS values for healthy and symptomatic infants aged 0–6 months. However, there is a notable gap in the literature concerning CoMiSS values for infants older than 6 months. This cross-sectional study aimed to determine CoMiSS values in presumed healthy infants who have completed 6 months and are up to 12 months old, hereafter referred to as 6 to 12 months old. Physicians from six European countries prospectively determined CoMiSS values in infants attending well-child clinics. Exclusion criteria included preterm delivery, acute or chronic disease, and the consumption of a therapeutic formula, dietary supplements (except vitamins), or medication. The following information was collected: gestational age, gender, age, type of feed (breast milk or infant formula), and complementary feeding. Descriptive statistics were summarized with mean and standard deviation for normally distributed continuous variables, median and IQR for non-normally distributed variables, and differences in CoMiSS values were analyzed with appropriate tests. Data from 609 infants were obtained. The overall median (Q1–Q3) CoMiSS values were 3 (1–5). Significant differences were found across age groups (p < 0.001), but not across groups based on gender (p = 0.551) or feeding type (p = 0.880).
Conclusions: This study provided CoMiSS values in presumed healthy infants aged 6–12 months. Additional studies should be conducted to establish the use of CoMiSS to assess cow’s milk-related symptoms in infants 6 months and older.
What is Known: • The Cow’s Milk-related Symptom Score (CoMiSS) is an awareness tool for evaluating symptoms related to cow’s milk. • CoMiSS values for presumed healthy infants aged 0-6 months infants are already available. | |
What is New: • CoMiSS values in European infants aged 6-12 months are provided. • These CoMiSS values differed across various age groups but not across groups based on gender or feeding type. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cow’s milk allergy (CMA) is a common food allergy in infants and young children. However, the prevalence varies based on geography, feeding methods, and assessment methods [1]. For instance, a recent systematic review from European countries found that the overall pooled estimates for self-reported lifetime prevalence of cow’s milk allergy is 5.7% [2, 3]. However when verified through food challenges, the prevalence drops to less than 1% [3, 4]. These rates are even lower, ranging from 0.4 to 0.5%, in exclusively breastfed infants [5, 6]. Misdiagnosis is a common issue, and overdiagnosis in some settings is of particular concern [7, 8]. Given the potential long-term health implications [9, 10], a diagnosis of CMA should be made cautiously. The diagnosis of immunoglobulin E (IgE)-mediated allergy is relatively easy because of its immediate symptom onset and the availability of validated tests to confirm the clinical history. However, non-IgE-mediated CMA presents a diagnostic challenge, as its symptoms often overlap with common functional gastrointestinal disorders, such as infantile colic or gastroesophageal reflux [11].
The Cow’s Milk-related Symptom Score (CoMiSS) was developed in 2015 as an awareness tool for healthcare professionals, to evaluate cow’s milk-related symptoms in infants aged 0–6 months [12]. It provides a total score, as well as subscale scores, based on the assessment of crying, regurgitation, stools, skin, and respiratory symptoms evaluated by a healthcare professional in the absence of infectious disease. Crying duration is scored from 0 (less than 1 h) to 6 (more than 5 h per day). The regurgitation score depends on volume and frequency, ranging from 0 (less than 2 episodes per day) to 6 (regurgitation of the complete feed after each feeding). Stool consistency is assessed with the Brussels Infant and Toddlers Stool Scale (BITSS), with scores ranging from 0 (formed stools) to 6 (watery stools). Skin symptoms include atopic eczema severity scores for different body regions for more than 1 week on head, neck, trunk (scores of 0–3) and extremities (scores of 0–3) and acute urticaria and/or angioedema (score of 6). Respiratory symptoms scores range from 0 (no respiratory symptoms) to 3 (severe symptoms). The total CoMiSS score ranges from 0 to 33 (Table 1).
In 2022, after reviewing evidence from 25 clinical trials, the CoMiSS was revised and updated [13]. The key changes included lowering the cut-off score from ≥ 12 to ≥ 10 to indicate the likelihood of symptoms being related to cow’s milk, and also replacing the Bristol Stool Scale with the Brussels Infant Toddlers Stool Scale (BITSS), as the latter is more appropriate for non-toilet trained children [14]. The panel of experts agreed that CoMiSS also may be potentially useful for infants between 6 and 12 months [13].
However, there is a lack of data on presumed healthy infants in this age range. The aim of this study was to determine the CoMiSS values in presumed healthy infants who have completed 6 months and are up to 12 months old, hereafter referred to as 6 to 12 months old. The purpose of this determination was to facilitate a better interpretation of the CoMiSS values in patients with symptoms within the age range where the diagnosis of CMA is often established.
Methods
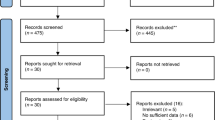
Study design and data collection
This was an international multicenter cross-sectional study conducted between September 2022 and April 2023. The study involved Investigators from Belgium, Bulgaria, Czech Republic, Italy, Poland, and Spain. Study subjects were enrolled by healthcare professionals at well-baby clinics during routine follow-up visit or vaccinations. All data were collected prospectively.
Participants
The study focused on presumed healthy infants between completed 6 and 12 months of age. Exclusion criteria included preterm delivery (less than 37 weeks), acute or chronic disease, and the consumption of a therapeutic formula (including partially hydrolyzed formula), dietary supplements (except vitamins), or medication.
Data collection
The following information was collected: gestational age, gender, age, type of feed (breast milk or infant formula), and complementary feeding. All of this data was recorded in a standardized Excel file (computer program, version 16.78, Microsoft Corporation, 2022). Subsequently, this collected data was combined and summarized at the end of the study.
CoMiSS assessment
The CoMiSS questionnaires were filled out by the health care providers, based on interviews conducted with the care providers. The interviews were carried out in the native languages of the participating countries, using questionnaires that are available in those local languages.
Ethical considerations
After obtaining informed consent from caregivers, the CoMiSS questionnaire was anonymously filled out. This study was approved by the respective ethical committees of participating institutions.
Statistical analysis
Descriptive statistics were employed, including the 5th, 25th, 75th, and 95th centiles, mean and standard deviation (SD) for normally distributed continuous variables, and median and interquartile ranges (IQR) for non-normally distributed variables. The normality was tested by Kolmogorov–Smirnov test. The global distribution of the CoMiSS for each value was calculated. Differences between groups were analyzed using a χ2-test for nominal variables, which are presented as the count and percentage (n%). The Mann–Whitney U test or Kruskal–Wallis test was used for continuous variables and results are presented as the median (Q1–Q3). Post hoc testing for skewed variables was done using a Nemenyi test. Regression analysis was performed to evaluate the impact of age, gender, country, and feeding type on CoMiSS values. A p value of < 0.05 was considered statistically significant. The analysis was performed using the R software (computer program; Version 3.5.1; http://cran.r-project.org).
Results
Population description
A total of 609 participants were recruited for the study, with the following distribution across countries: Belgium, 21 (3.5%); Bulgaria, 59 (9.7%); Czech Republic, 55 (9%); Italy, 94 (15%); Poland, 282 (46%); and Spain, 98 (16%). Overall, 333 (54%) boys and 276 (45%) girls were included. In terms of type of feeding type, 210 (34%) were breastfed, 264 (43%) were formula fed, and 135 (22%) were mixed fed. For the purposes of some of the analyses, mixed feeding was combined with formula feeding into one group (n = 399). Complementary feeding was introduced in 584 infants (96%). The overall median (Q1–Q3) age was 37 (30–44) weeks. There was no missing data. All study sites reported completed data for infants who met the inclusion criteria. Subjects’ characteristics are presented in Table S1.
Overall results of the CoMiSS
Descriptive statistics of the CoMiSS in infants aged 6–12 months are presented in Table 2. The overall median (Q1–Q3) CoMiSS values were 3 (1–5). CoMiSS values ≥ 10 were observed in 1.3% of infants (n = 8). There were no significant differences in total CoMiSS values according to gender (p = 0.55) or type of feed (p = 0.9). However, the post hoc analysis showed significantly higher total CoMiSS scores in infants aged 6 months compared to 10 months (p = 0.001) and 11 months (p = 0.007). The highest median CoMiSS value was observed in infants at 6 months [4], while the lowest median value was observed in infants at 12 months [1].
The median and interquartile range were consistent among genders and types of feed, except for mixed feeding, where Q3 was 4. The 95th percentile for total CoMiSS was 8 and was consistent with the group of girls and formula-fed infants. The 95th percentile was lower in the group of boys (7.4), breastfed infants [7], and mixed-fed infants (7.3). The distribution of the total CoMiSS values is presented in Fig. S1, Supplemental Materials. In the regression analysis, it was observed that age significantly predicted CoMiSS values, irrespective of the country and feeding method (β = −0.270, p < 0.001). Moreover, even when the impact of the feeding method was excluded from the analysis, age continued to be a significant predictor for CoMiSS (β = −0.259, p < 0.001).
Contribution of symptoms to the CoMiSS
The distribution of each symptom in the CoMiSS according to gender, type of feed, and age is presented in Figs. S2, S3, and S4 (supplementary materials), respectively.
Crying
There were no differences in the crying score across the gender (p = 0.14), age (p = 0.88), or type of feed (p = 0.12).
Regurgitation
No differences in regurgitation score values were found according to gender (p = 0.12) or type of feed (p = 0.48). However, there were significant differences observed across age groups (p = 0.02). Out of the total participants, 17 infants (2.8%) had a regurgitation score greater than 3. The majority of these infants (10 out of 17) were 6 months old. None of the infants presented with regurgitations of the total volume after each meal (score of 6), and only one infant (0.2%) had regurgitations of more than half of the reported volume in at least half of meals (score of 5).
Stools
There were no significant differences in the stools score based on gender (p = 0.97) or type of feed (p = 0.56). However, there was a significant change in the stools score with age (p < 0.001). Significantly higher values were present in infants at 6 months compared to infants at 10 (p = 0.01) and 11 months (p = 0.02) of age. Among 230 infants with stools score of 4 or above, 70 infants (30%) were aged 6 months.
Skin symptoms
No significant differences were found in the total skin score according to age (p = 0.69), gender (p = 0.37), or feeding type (p = 0.15). Urticaria was reported in only one of the included participants.
Respiratory symptoms
There were no differences in respiratory symptoms according to gender (p = 0.18), age (p = 0.13), or feeding type (p = 0.72). No infants were reported as having severe respiratory symptoms.
Discussion
The median CoMiSS value in presumed healthy infants between 6 and 12 months in different European countries was found to be 3, which corresponds with data from infants up to the age of 6 months [15]. While previous data showed a tendency for higher CoMiSS values with increasing age in infants up to 6 months, this study showed a significant decrease in total CoMiSS values in subsequent months, starting from a median of 3 at 6 months and decreasing to a median of 1 at 12 months. A similar trend was observed for the 95th centile. Overall, the 95th centile was 8, with a tendency to be lower in subsequent months, reaching 7 at 12 months. Interestingly, the lowest 95th centile was observed at 10 months and was 6. However, there were relatively few participants in this age group (n = 78), which could have influenced the results. Our results emphasize the importance of age in understanding and interpreting CoMiSS values in infants aged 6–12 months. Further research could explore the underlying mechanisms behind this association and its implications for assessing cow’s milk-related symptoms in this age group.
This study has limitations. The study was conducted using a convenience sample of infants attending well-clinics for routine check-ups, rather than employing a random sampling method. This introduces a potential bias, as the characteristics of these infants may differ from those who were not approached or did not participate, thus, limiting the generalizability of the findings to the wider population of healthy infants. The questionnaires used in this study were translated into the native languages of participating countries; however, they were not validated. Although the researchers completed the questionnaire based on the answers in the native language and ensured that it corresponded to the original language of the questionnaire, there is a risk of translation bias. Furthermore, there is a risk of non-response bias, as the participation of parents in the study may have been influenced by factors related to their infant’s health or symptoms. This introduced the possibility of selection bias and limits the representativeness of the included participants. Additionally, there was a discrepancy in the size of cohorts from different countries included in this study. Participants from Poland accounted for close to 47% of all infants analyzed, which could have influenced the results and introduced a potential bias. It is important to consider the impact of this uneven distribution when interpreting the findings.
As stated in the Introduction, CoMiSS was developed as an awareness tool to help healthcare providers identify potential cow’s milk-related symptoms in infants. However, it is important to understand that it is not a diagnostic tool. A definitive diagnosis of CMA requires further tests, such as an oral food challenge. Therefore, CoMISS should only be used as a preliminary step to identify the likelihood of CMA and guide initial management; it should not replace formal diagnostic procedures. Furthermore, although modified CoMiSS scores have been used for predicting lactose intolerance in adults [16] and efforts are made to investigate the relationship between fecal calprotectin levels and CoMiSS scores [17], these applications have not been validated. Therefore, we do not recommend using CoMiSS for purposes other than those for which it was developed.
In conclusion, this study provides CoMiSS values for presumed healthy European infants aged 6–12 months, extending our understanding beyond the commonly studied age range (0–6 months). The influence of age on CoMiSS values highlights the importance of age-specific reference ranges when interpreting CoMiSS values in infants aged 6–12 months. Further research is needed to assess the use of CoMiSS as an awareness tool for cow’s milk-related symptoms for symptomatic infants older than 6 months.
References
Woods RK, Stoney RM, Raven J, Walters EH, Abramson M, Thien FC (2002) Reported adverse food reactions overestimate true food allergy in the community. Eur J Clin Nutr 56(1):31–36
Spolidoro GCI, Amera YT, Ali MM, Nyassi S, Lisik D, Ioannidou A et al (2023) Frequency of food allergy in Europe: an updated systematic review and meta-analysis. Allergy 78(2):351–368
Vandenplas Y, Broekaert I, Domellof M, Indrio F, Lapillonne A, Pienar C et al (2023) An ESPGHAN position paper on the diagnosis, management and prevention of cow’s milk allergy. J Pediatr Gastroenterol Nutr
Schoemaker AA, Sprikkelman AB, Grimshaw KE, Roberts G, Grabenhenrich L, Rosenfeld L et al (2015) Incidence and natural history of challenge-proven cow’s milk allergy in European children–EuroPrevall birth cohort. Allergy 70(8):963–972
Host A, Husby S, Osterballe O (1988) A prospective study of cow’s milk allergy in exclusively breast-fed infants. Incidence, pathogenetic role of early inadvertent exposure to cow’s milk formula, and characterization of bovine milk protein in human milk. Acta Paediatr Scand 77(5):663–70
Saarinen KM, Juntunen-Backman K, Järvenpää AL, Klemetti P, Kuitunen P, Lope L et al (2000) Breast-feeding and the development of cows’ milk protein allergy. Adv Exp Med Biol 478:121–130
Mehta S, Allen HI, Campbell DE, Arntsen KF, Simpson MR, Boyle RJ (2022) Trends in use of specialized formula for managing cow’s milk allergy in young children. Clin Exp Allergy 52(7):839–847
Allen H, Gupta A, Mundell A, Gupta N, Thakur A, Nagarajan S et al (2023) Formula milk companies and allergy healthcare professionals in India. Clin Exp Allergy 53(7):697–710
Meyer R, Godwin H, Dziubak R, Panepinto JA, Foong RM, Bryon M et al (2017) The impact on quality of life on families of children on an elimination diet for Non-immunoglobulin E mediated gastrointestinal food allergies. World Allergy Organ J 10(1):8
Meyer R, De Koker C, Dziubak R, Godwin H, Dominguez-Ortega G, Chebar Lozinsky A et al (2016) The impact of the elimination diet on growth and nutrient intake in children with food protein induced gastrointestinal allergies. Clin Transl Allergy 6:25
Munblit D, Perkin MR, Palmer DJ, Allen KJ, Boyle RJ (2020) Assessment of Evidence About Common Infant Symptoms and Cow’s Milk Allergy. JAMA Pediatr 174(6):599–608
Vandenplas Y, Dupont C, Eigenmann P, Host A, Kuitunen M, Ribes-Koninckx C et al (2015) A workshop report on the development of the Cow’s Milk-related Symptom Score awareness tool for young children. Acta Paediatr 104(4):334–339
Vandenplas Y, Bajerova K, Dupont C, Eigenmann P, Kuitunen M, Meyer R et al (2022) The cow’s milk related symptom score: the 2022 update. Nutrients 14(13)
Bajerova K, Salvatore S, Dupont C, Kuitunen M, Meyer R, Ribes-Koninckx C et al (2023) Cow’s Milk-related Symptom Score (CoMiSS): from Bristol to Brussels Stool Scale. J Pediatr Gastroenterol Nutr
Vandenplas Y, Salvatore S, Ribes-Koninckx C, Carvajal E, Szajewska H, Huysentruyt K (2018) The cow milk symptom score (CoMiSSTM) in presumed healthy infants. PLoS One 13(7):e0200603
Mohammed HI, Baioumy E, Allam MF, Al-Ashram MNB (2022) Validation of a modified Cow’s Milk-related Symptom Score (CoMISS) for screening of lactose intolerance in adults. Curr Med Res Opin 38(6):947–953
Zain-Alabedeen S, Kamel N, Amin M, Vernon-Roberts A, Day AS, Khashana A (2023) Fecal calprotectin and cow’s milk-related-symptoms score in children with cow’s milk protein allergy. Pediatr Gastroenterol Hepatol Nutr 26(1):43–49
Author information
Authors and Affiliations
Contributions
MJ conducted all analyses and assumed the main responsibility for the writing of the first draft of the manuscript. MJ, FA, KB, MECR, CRK, RP, SS, and AS collected the data. All authors critically revised it for important intellectual content and provided final approval of the version to be submitted for publication. HS is the guarantor.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol of the study was reviewed and approved by the Ethics Committee of the Medical University of Warsaw (AKBE/196/2022). The research was conducted in accordance with the Declaration of Helsinki. Parents/caregivers of the participants were fully informed about the study, and informed consent was obtained.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Gregorio Milani
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Katerina Bajerova, Christophe Dupont, Mikael Kuitunen, Rosan Meyer, Carmen Ribes Koninckx, Silvia Salvatore, Raanan Shamir, Annamaria Staiano, Yvan Vandenplas, and Hania Szajewska are members of the CoMiSS Study Group.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jankiewicz, M., Ahmed, F., Bajerova, K. et al. Cow’s Milk-related Symptom Score (CoMiSS) values in presumed healthy European infants aged 6–12 months: a cross-sectional study. Eur J Pediatr 183, 707–713 (2024). https://doi.org/10.1007/s00431-023-05334-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05334-0