Abstract
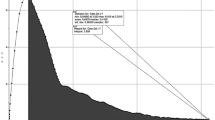
The aim of the present study was to define an initial angle called β and to assess its diagnostic value for identifying poor-quality maneuvers in spirometry testing in children. Furthermore, its predictive equation or normal value was explored. Children aged 4–14 years with respiratory symptoms who underwent spirometry were enrolled. Based on the efforts labeled during maneuvering and the quality control criteria of the guidelines, children were categorized into good-quality and poor-quality groups. According to ventilatory impairment, children in the good-quality group were divided into three subgroups: normal, restricted, and obstructed. Angle β was the angle between the line from the expiratory apex to the origin of coordinates and the x-axis of the maximal expiratory flow-volume (MEFV) curve. Demographic characteristics, angle β, and other spirometric parameters were compared among groups. The diagnostic values of angle β, forced expiratory time (FET), and their combination were assessed using receiver operating characteristic curves. Data from 258 children in the good-quality group and 702 healthy children in our previous study were used to further explore the predictive equation or normal value of angle β. The poor-quality group exhibited a significantly smaller angle β (76.44° vs. 79.36°; P < 0.001), significantly lower peak expiratory flow (PEF), FET, and effective FET (ETe), and significantly higher expiratory volume at peak flow rate (FEV-PEF) and ratio of extrapolated volume and forced vital capacity (EV/FVC) than the good-quality group. There was no significant difference in angle β among the normal, restricted, and obstructed groups. Logistic regression analysis revealed that smaller angle β and FET values indicated poor-quality MEFV curves. The combination of angle β < 74.58° and FET < 4.91 s had a significantly larger area under the curve than either one alone. The normal value of angle β of children aged 4–14 years was 78.40 ± 0.12°.
Conclusions: Angle β contributes to the quality control evaluation of spirometry in children. Both angle β < 74.58° and FET < 4.91 s are predictors of poor-quality MEFV curves, while their combination offers the highest diagnostic value.
What is Known: • A slow start is one of the leading causes of poor-quality maximal expiratory flow-volume (MEFV) curves, which is a particularly prominent issue among children due to limited cooperation, especially those younger than 6 years old. • It is relatively difficult to differentiate between ventilatory dysfunction and poor cooperation when a slow start occurs in children; therefore, there is an urgent need for an objective indicator that is unaffected by ventilatory impairment to evaluate quality control of spirometry. | |
What is New: • The initial angle β, which was introduced at the ascending limb of the MEFV curve in the present study, has a certain diagnostic value for poor-quality MEFV curves in children. • Angle β < 74.58° is a predictor of poor-quality MEFV curves, and its combination with FET < 4.91 s offers a higher diagnostic value. |



Similar content being viewed by others
Availability of data and materials
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
Abbreviations
- ATS:
-
American Thoracic Society
- ERS:
-
European Respiratory Society
- ETe:
-
Effective FET
- ETp:
-
Plateau FET
- EV:
-
Extrapolated volume
- FET:
-
Forced expiratory time
- FEV1 :
-
Forced expiratory volume in 1 s
- FEV-PEF:
-
Expiratory volume at peak flow rate
- FVC:
-
Forced vital capacity
- MEFV:
-
Maximal expiratory flow-volume
- PEF:
-
Peak expiratory flow
References
Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald JM, Gibson P, Ohta K, O’Byrne P, Pedersen SE, Pizzichini E, Sullivan SD, Wenzel SE, Zar HJ (2008) Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J 31:143–178. https://doi.org/10.1183/09031936.00138707
Watz H, Tetzlaff K, Magnussen H et al (2018) Spirometric changes during exacerbations of COPD: a post hoc analysis of the WISDOM trial. Respir Res 19:251. https://doi.org/10.1186/s12931-018-0944-3
Halpin DMG, Criner GJ, Papi A et al (2021) Global initiative for the diagnosis, management, and prevention of chronic obstructive lung disease. The 2020 GOLD science committee report on COVID-19 and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 203:24–36. https://doi.org/10.1164/rccm.202009-3533SO
Eguiluz-Gracia I, van den Berge M, Boccabella C et al (2021) Real-life impact of COVID-19 pandemic lockdown on the management of pediatric and adult asthma: a survey by the EAACI Asthma Section. Allergy 76:2776–2784. https://doi.org/10.1111/all.14831
Loeb JS, Blower WC, Feldstein JF et al (2008) Acceptability and repeatability of spirometry in children using updated ATS/ERS criteria. Pediatr Pulmonol 43:1020–1024. https://doi.org/10.1002/ppul.20908
Beydon N, Davis SD, Lombardi E et al (2007) An official American Thoracic Society/European Respiratory Society statement: pulmonary function testing in preschool children. Am J Respir Crit Care Med 175:1304–1345. https://doi.org/10.1164/rccm.200605-642ST
Graham BL, Steenbruggen I, Miller MR et al (2019) Standardization of spirometry 2019 update. An official American thoracic society and European respiratory society technical statement. Am J Respir Crit Care Med 200:e70–e88. https://doi.org/10.1164/rccm.201908-1590ST
McKibben JM, McKay RT, Freeman AG et al (2011) Redefining spirometry hesitating start criteria based on the ratio of extrapolated volume to timed FEVs. Chest 140:164–169. https://doi.org/10.1378/chest.09-2198
Enright P, Vollmer WM, Lamprecht B et al (2011) Quality of spirometry tests performed by 9893 adults in 14 countries: the BOLD Study. Respir Med 105:1507–1515. https://doi.org/10.1016/j.rmed.2011.04.008
Ashba J, Garshick E, Tun CG et al (1993) Spirometry—acceptability and reproducibility in spinal cord injured subjects. J Am Paraplegia Soc 16:197–203. https://doi.org/10.1080/01952307.1993.11735901
Cui X, Li Z, Teng Y et al (2020) Association between bedroom particulate matter filtration and changes in airway pathophysiology in children with asthma. JAMA Pediatr 174:533–542. https://doi.org/10.1001/jamapediatrics.2020.0140
Halpin DMG, Meltzer EO, Pisternick-Ruf W et al (2019) Peak expiratory flow as an endpoint for clinical trials in asthma: a comparison with FEV1. Respir Res 20:159. https://doi.org/10.1186/s12931-019-1119-6
Melia U, Burgos F, Vallverdú M et al (2014) Algorithm for automatic forced spirometry quality assessment: technological developments. PLoS ONE 9:e116238. https://doi.org/10.1371/journal.pone.0116238
Berrier A, Tiotiu A, Bonabel C et al (2021) Assessment of bronchial obstruction and its reversibility by shape indexes of the flow-volume loop in asthmatic children. Pediatr Pulmonol 56:226–233. https://doi.org/10.1002/ppul.25162
Dominelli PB, Foster GE, Guenette JA et al (2015) Quantifying the shape of the maximal expiratory flow-volume curve in mild COPD. Respir Physiol Neurobiol 219:30–35. https://doi.org/10.1016/j.resp.2015.08.002
Kapp MC, Schachter EN, Beck GJ et al (1988) The shape of the maximum expiratory flow volume curve. Chest 94:799–806. https://doi.org/10.1378/chest.94.4.799
Lian N, Li L, Ren W et al (2017) Angle β of greater than 80° at the start of spirometry may identify high-quality flow volume curves: Angle β at the start of spirometry. Respirology 22:527–532. https://doi.org/10.1111/resp.12950
Quanjer PH, Stanojevic S, Cole TJ et al (2012) Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J 40:1324–1343. https://doi.org/10.1183/09031936.00080312
Stanojevic S, Kaminsky DA, Miller MR et al (2022) ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J 60:2101499. https://doi.org/10.1183/13993003.01499-2021
Feng Y, Yu X-H, Song Y-X et al (2021) Establishment of a predictive equation for pulmonary ventilation function in school-aged children in northeast China: a prospective study. Zhongguo Dang Dai Er Ke Za Zhi 23:1119–1126. https://doi.org/10.7499/j.issn.1008-8830.2108139
Feng Y, Yang Q, Shang Y (2021) “Poor Effort” does not account for reduced forced vital capacity in asthmatic children. Front Pediatr 9:596384. https://doi.org/10.3389/fped.2021.596384
Culver BH, Graham BL, Coates AL et al (2017) Recommendations for a standardized pulmonary function report. An official American Thoracic Society technical statement. Am J Respir Crit Care Med 196:1463–1472. https://doi.org/10.1164/rccm.201710-1981ST
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Zanconato S, Meneghelli G, Braga R et al (2005) Office spirometry in primary care pediatrics: a pilot study. Pediatrics 116:e792-797. https://doi.org/10.1542/peds.2005-0487
Arets HGM, Brackel HJL, van der Ent CK (2001) Forced expiratory manoeuvres in children: do they meet ATS and ERS criteria for spirometry? Eur Respir J 18:655–660. https://doi.org/10.1183/09031936.01.00204301
Pesant C, Santschi M, Praud J-P et al (2007) Spirometric pulmonary function in 3- to 5-year-old children. Pediatr Pulmonol 42:263–271. https://doi.org/10.1002/ppul.20564
Zhang Y, Shi H, Su A et al (2022) Angle β combined with FeNO and FEV1/FVC% for the detection of asthma in school-aged children. J Asthma 59:746–754. https://doi.org/10.1080/02770903.2021.1874979
Gochicoa-Rangel L, Rodríguez-Peralta KY, Gutiérrez-Bautista AK et al (2022) Maximal inspiratory and expiratory flow at moderate altitude: a study of a Latin American population. BMC Pulm Med 22:147. https://doi.org/10.1186/s12890-022-01943-x
Sadiq S, Rizvi NA, Soleja FK, Abbasi M (2019) Factors affecting spirometry reference range in growing children. Pak J Med Sci 35:1587–1591. https://doi.org/10.12669/pjms.35.6.1212
Jones MH, Vidal PCV, Lanza FC et al (2020) Reference values for spirometry in Brazilian children. J Bras Pneumol 46:e20190138. https://doi.org/10.36416/1806-3756/e20190138
Miller MR, Hankinson J, Brusasco V et al (2005) Standardisation of spirometry. Eur Respir J 26:319–338. https://doi.org/10.1183/09031936.05.00034805
Müller-Brandes C, Krämer U, Gappa M et al (2014) LUNOKID: can numerical American Thoracic Society/European Respiratory Society quality criteria replace visual inspection of spirometry? Eur Respir J 43:1347–1356. https://doi.org/10.1183/09031936.00058813
Enright PL, Linn WS, Avol EL et al (2000) Quality of spirometry test performance in children and adolescents : experience in a large field study. Chest 118:665–671. https://doi.org/10.1378/chest.118.3.665
Funding
None.
Author information
Authors and Affiliations
Contributions
YLJ, SYX, and FY conceived and designed the study. MLD, LX, LXW, and LF were responsible for the collection and analysis of the experimental data. YLJ and FY interpreted the data and drafted the manuscript which was revised by all authors. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was obtained from the Ethics Committee of Shengjing Hospital of China Medical University (approval number: 2022PS073K). This study was conducted in accordance with the principles of the Declaration of Helsinki.
Consent to participate
Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yao, L., Meng, L., Liu, X. et al. The initial angle of the maximum expiratory flow-volume curve: a novel start-of-test criteria of spirometry in children. Eur J Pediatr 183, 435–444 (2024). https://doi.org/10.1007/s00431-023-05323-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05323-3