Abstract
A surge in pediatric COVID-19 cases was observed during the fifth wave (Omicron) of the COVID-19 pandemic. Little is known about the clinical features and disease course in neonates and young infants. To describe the clinical and laboratory features, disease course and complications of COVID-19 in neonates and infants younger than 6 months. A retrospective descriptive study in which data were collected from the electronic medical records of infants younger than 6 months, with positive nasal swab tests for COVID-19. Fifty-two infants younger than 6 months who tested positive for COVID-19 were admitted to our pediatric ER/department during the omicron wave of the COVID-19 pandemic, between December 2021 and December 2022. Twenty-one percent were discharged from the ER, while the others were hospitalized predominantly for observation or supportive treatment, with an average duration of hospitalization of 1.3 ± 0.7 days. No major complications were observed.
Conclusion: COVID-19 is a mild viral illness in young healthy infants with no major complications.
What is Known: • Pediatric patients generally have a milder clinical presentation of COVID-19 but can also experience more severe symptoms and post-COVID phenomena. • Our knowledge of COVID-19 in neonates and young infants is limited, and guidelines for their diagnosis and management are lacking. | |
What is New: • In neonates and young infants, COVID-19 infection is typically a mild viral illness with no major complications observed in the majority of cases. • Hospitalization may not be necessary for well-appearing infants with COVID-19, as long as their clinical and laboratory evaluations do not raise any concerns. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Covid-19 pandemic has affected the population of the entire world, including children [1]. During the pandemic we continuously revealed new aspects regarding SARS-COV-2. In pediatric patients, we generally observed a milder clinical presentations involving upper respiratory tract infection, gastrointestinal manifestations, changes in taste and smell. However, there were also more severe presentations including lower tract respiratory infections, myocarditis, and post-CORONA phenomena such as long-COVID and Multi-System Inflammatory Syndrome in children & adolescents (MIS-C) [2].
As time passed we gained more experience in the diagnosis and treatment of SARS-COV-2 in adult patients but our knowledge regarding the clinical presentation, disease course and outcome in neonates and young infants infected with the virus, remains limited [3]. There is a knowledge gap regarding the clinical course and management of neonates and young infants with COVID-19. We extrapolate our knowledge regarding these young patients from older pediatric patients, and from a limited number of research articles [4] and case reports [5, 6] published during the pandemic. However, we continue to gain more experience with the young ages in order to create clear and uniformed guidelines especially for the treatment of young infants and neonates.
During previous waves of COVID-19 when the Alpha and Delta variants were dominant, there were a limited number of cases in neonates and young infants as reported in the United States where children younger than one year old represented less than 1% of all cases [7]. On the other hand, during the fifth wave when the omicron variant (B.1.1.529) was dominant there were more reported cases in children younger than 4 years. The rate of hospitalization was five times greater than the rate during previous waves (DELTA). Most of the hospitalized children (63%) were healthy with no underlying medical conditions, infants less than 6 months old accounted for 44% of hospitalizations. No differences in severity of the disease was noticed among various ages according to the Morbidity and Mortality Weekly Report (MMWR) published in March 2022 [8].
As previously mentioned, during the fifth wave of COVID-19, while dealing with massive infections by the fast-spreading variant of SARS-COV-2; Omicron [9], we encountered more cases of COVID-19 infections in young infants and neonates. Since guidelines are lacking, our general routine was to hospitalize most positive infants for observation. Our hospital's routine during the 5th wave was to test each febrile or hospitalized infant for SARS-COV-2. We evaluated patients who exhibited a wide range of clinical presentations including asymptomatic patients, those with mild symptoms, and others with more severe presentations including bronchiolitis, pneumonia, and myocarditis. In addition, we recognized a unique group of patients; neonates, brought to the emergency room (ER) with fever and diagnosed with SARS-COV-2 infection. These patients elicited the question whether they needed to go through a full sepsis work up because they were diagnosed with this viral infection.
In this study we aimed to examine and summarize our knowledge and experience regarding the clinical presentation, disease course, outcome and complications of neonates and infants younger than 6 months admitted to the pediatric ER with positive Polymerase Chain Reaction (PCR) nasal swabs for COVID-19, and based on these data, recommend management for these youngsters.
We present the clinical characteristics of 52 infants younger than 6 months, who presented to the pediatric ER at Carmel hospital during the 5th wave (Omicron) of SARS-COV-2, and were diagnosed with SARS-COV-2 infection. In addition, after reviewing all the neonatal cases we suggest management for such infants.
Methods
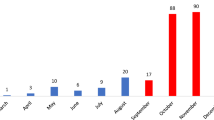
A retrospective descriptive single center study of infants younger than 6 months admitted to the pediatric ER in Carmel Medical Center, Haifa, Israel, with a positive PCR test from nasal swab for COVID-19 between December 2021 and December 2022.
All neonates and infants 6 months old and younger who presented to the pediatric ER with compatible viral symptoms and/or a history of exposure to a confirmed case of COVID-19, with positive PCR test during the 5th wave of the pandemic, were included in the study. Infants diagnosed with other viral infections from nasal swabs, or with severe congenital malformations were excluded from the study.
For those infants included in our study the following data were collected: demographic, clinical data (days of fever, symptoms and signs, pulse, O2 saturation etc.) and laboratory data. The primary outcomes were the clinical features and outcomes of neonates and young infants with COVID-19.
Continuous variables were presented as means and standard deviation (SD) or medians and interquartile ranges (IQR) values as appropriate. Categorical variables were expressed as the counts and percentages in each category.
Results
During the study period 52 infants younger than 6 months were admitted to our pediatric ER. Ten patients were younger than one month, 33 patients where 2–3 months old and 9 patients where 3–6 months old. The mean age of the infants was 8.6 weeks (range 2–20 weeks), 27/52 (51.9%) were boys and 48.1% were girls. Table 1 summarizes the epidemiological, clinical and laboratory characteristics of the patients in the study.
The most common reason for ER referral was fever 86.5% (45/52 infants). Other common symptoms are noted in (Table 1). However, only 21 patients had a measured temperature of 38 ºC or above at the ER or in the pediatric ward.
Twenty-three patients (44.2%) had normal physical examinations, 13 patients (25%) had maculopapular rashes and another 7 (13.4%) infants had mild rales on lung osculation. Laboratory test revealed that 2 (3.7%) infants experienced neutropenia (< 1000 absolute neutrophil counts). The mean C-Reactive Protein (CRP) level was 0.42 ± 0.77 mg/dl. All but one infant had normal urinalysis and urine culture, and all Cerebrospinal Fluid (CSF) cultures withdrawn for 11 infants who underwent Lumbar Puncture (LP) were also negative.
Eleven patients (21.1%) were discharged following examination in the ER. Mean duration of hospitalization for those who were admitted to the pediatric ward was 1.3 ± 0.7 days. Regarding the reason for admission; 37 (90.2%) patients were hospitalized mainly for observation due to their young age, 3 (7.3%) patients were treated with antibiotics which was stopped following the negative results of cultures, and 1 (2.4%) patient was admitted for treatment of epilepsy. Three infants were treated with antibiotics following lumbar puncture examinations. The indications for treatment were; fever in a 3-week-old neonate, bloody diarrhea and abnormal urinalysis. For these patients the antibiotic treatment was discontinued following two days of treatment owing to negative stool, blood and CSF cultures. One patient’s urine culture was positive with 10 K Colony Forming Unit (CFU) of two bacteria, which is most likely due to contamination. Four infants (7.6%) received intravenous (IV) fluids due to low intake.
The median O2 saturation was 98% (IQR: 98–99), none of the infants needed O2 supplementation during hospitalization. It should be noted that none of the infants underwent chest X-ray. Aside from mild upper respiratory tract symptoms including one infant with stridor, no other respiratory complaints were noted.
During hospitalization, two infants experienced tachycardia with pulse rates > 200/min. Both had mild increase in Creatine Phosphokinase (CPK) and troponin levels (one infant had CPK levels of 83 U/L and troponin of 37 ng/L and the other one had CPK levels of 78 U/L and troponin of 57 ng/L), which normalized after 24 h, both underwent electrocardiogram (ECG), echocardiogram and a cardiologic evaluation which were normal. During their hospital stay the pulse rates normalized.
In total, 11 infants underwent lumbar puncture; Of these, three infants due to full fontanelle on physical examination (two were normal and the latter revealed mild pleocytosis with negative PCR test for Enterovirus and COVID-19). Three infants had LP due to their young age (3 weeks) per neonatal fever protocol (normal CSF). One infant, less than 3 months old, had LP due to dysentery (the CSF was bloody and could not be interpreted, though the CSF culture was negative). Another infant less than 3 months old had a LP due to abnormal urinalysis (urine culture was positive for 2 bacteria- most likely contamination). One patient underwent LP due to restlessness and another due to restlessness and neutropenia (mild pleocytosis in the CSF and normal cultures). One infant had a LP due to seizures (mild pleocytosis in the CSF with negative CSF culture and negative PCR for Herpes Simplex Virus (HSV) & Enterovirus).
Of note, none of the participants returned to the hospital within a month after discharge. We are unaware of any long COVID phenomena, Pediatric Inflammatory Multisystem Syndrome (PIMS) or Kawasaki in the participants of the current study.
Discussion
Little is known about the clinical course of COVID-19 infection in neonates and young infants. Recent studies estimated that children accounted for 1–5% of all COVID-19 cases. Children are less susceptible to COVID-19 and seem to be affected less frequently than adults. Suggested reasons include more active innate immune responses among children, healthier respiratory tracts and fewer underlying disorders [8]. Though there are several reports of children with COVID-19 infections, very few reported the disease in neonates and young infants.
During the fifth wave of the pandemic, with the Omicron variant which was more transmissible, a higher percentage of children contracted the illness. We noticed more cases in neonates and young infants, which presented us with the question of how to evaluate these infants especially neonates under 28 days old; whether they should undergo a full sepsis workup and be treated with antibiotics or perhaps to hospitalize them for observation only. Since no clear answers are provided in the literature, we completed this small series about neonates and infants younger than 6 months diagnosed with COVID-19 during the Omicron wave. According to our results, the disease is mild with no major respiratory complaints or complications in this group of patients. Most were hospitalized for observation only due to their young age. None needed oxygen supplementation or more invasive mechanical ventilation. No secondary bacterial infections were noted and all of the infants had laboratory test results within normal ranges. There were with no cases of bacteremia or urinary tract infections (UTI) identified that required antibiotic treatments. Similar results were noted in one study which was conducted during the first year of the pandemic [9] which also concluded that COVID-19 in young infants is a mild viral illness. Therefore, given the high frequency of hospitalization among infants with COVID-19, it may be reasonable to discharge well appearing young infants with COVID-19, rather than keeping them under observation, as long as their clinical and laboratory evaluations do not raise any concerns.
COVID-19 can cause mild myocarditis in young infants; therefore, it is crucial to measure the heart rate in all neonates with COVID-19, and if tachycardia or arrhythmia is observed, a full workout for myocarditis should be conducted including electrocardiography and echocardiography.
Regarding whether neonates with fever and a positive COVID-19 test require a full sepsis workup like any other neonate with fever, our study suggests that a well-appearing neonate with a positive COVID-19 test may not need a full sepsis workup. However, our study is limited in its ability to make a definitive conclusion on this matter, as we had only a small cohort of 7 infants under 3 months old who underwent LP, consisting of 3 neonates less than 1 month old with fever and 4 patients younger than 3 months with a high risk for meningitis based on the Rochester criteria. Nevertheless, no cases of serious bacterial infections were identified in our cohort. Similar results were found in a previous study[9], which raises concerns about the potential negative impact of the virus on antibiotic stewardship. To make more definitive conclusions, further studies of patients younger than 3 months with COVID-19 are required.
Study limitations: A retrospective and descriptive single center study on a small number of infants under 6 months old, a very small number of neonates (< 28 days old) with neonatal fever and positive COVID-19 test for whom a full sepsis workup was done.
No long-term follow-up for these infants was conducted beyond the observation that there were no re-admissions during the 30 days post COVID-19 diagnosis so we cannot conclude regarding long COVID complications.
In conclusion, our study sheds light on the clinical course of COVID-19 infection in neonates and young infants, particularly during the fifth wave of the pandemic with the Omicron variant. Our findings suggest that COVID-19 in this age group is a mild viral illness with no major respiratory or other complications identified, and hospitalization may not be necessary for well-appearing infants with COVID-19, as long as their clinical and laboratory evaluations do not raise concerns. However, further studies are needed to make more definitive conclusions especially regarding the need for full sepsis workups and antibiotic treatments in neonates less than 28 days old.
Data availability
The data that supports the findings of this study are available from the corresponding auther, S.S, upon reasonable request.
Abbreviations
- CFU:
-
Colony Forming Unit
- CPK:
-
Creatine Phosphokinase
- CRP:
-
C-Reactive Protein
- CSF:
-
Cerebrospinal Fluid
- ECG:
-
Electrocardiogram
- ER:
-
Emergency room
- HSV:
-
Herpes simplex virus
- IQR:
-
Interquartile range
- IV:
-
Intravenous
- LP:
-
Lumbar Puncture
- MIS-C:
-
Multi-System Inflammatory Syndrome in children and adolescents
- MMWR:
-
Morbidity and Mortality Weekly Report
- PCR:
-
Polymerase Chain Reaction
- PIMS:
-
Pediatric Inflammatory Multisystem Syndrome
- SD:
-
Standard deviation
- UTI:
-
Urinary Tract Infection
References
Zhu N, Zhang D, Wang W et al (2020) A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med 382:727–733. https://doi.org/10.1056/NEJMOA2001017
Alsohime F, Temsah MH, Al-Nemri AM et al (2020) COVID-19 infection prevalence in pediatric population: Etiology, clinical presentation, and outcome. J Infect Public Health 13:1791–1796. https://doi.org/10.1016/J.JIPH.2020.10.008
Covid-19 in pregnant women and babies: What pediatricians need to know | Elsevier Enhanced Reader. https://reader.elsevier.com/reader/sd/pii/S1526054220300919?token=1E9BF168414BBB1D2D5BA613E5569F4DF2C92C047BDF9497EB22448B304758C9F930B1059629A74B2DDBA79C453484B2&originRegion=eu-west-1&originCreation=20220204174931. Accessed 4 Feb 2022
Hassan M, Khalil A, Magboul S et al (2021) Neonates and Young Infants With COVID-19 Presented With Sepsis-Like Syndrome: A Retrospective Case Controlled Study. Front Pediatr 9. https://doi.org/10.3389/FPED.2021.634844
Coronado Munoz A, Nawaratne U, McMann D et al (2020) Late-Onset Neonatal Sepsis in a Patient with Covid-19. N Engl J Med 382:e49. https://doi.org/10.1056/NEJMC2010614
Ryan L, Plötz FB, van den Hoogen A et al (2021) Neonates and COVID-19: state of the art : Neonatal Sepsis series. Pediatr Res. https://doi.org/10.1038/S41390-021-01875-Y
Spoulou V, Noni M, Koukou D et al (2021) Clinical characteristics of COVID-19 in neonates and young infants. Eur J Pediatr 180:3041–3045. https://doi.org/10.1007/S00431-021-04042-X/TABLES/2
Marks KJ, Whitaker M, Agathis NT et al (2022) Hospitalization of Infants and Children Aged 0–4 Years with Laboratory-Confirmed COVID-19 — COVID-NET, 14 States, March 2020–February 2022. MMWR Morb Mortal Wkly Rep 71:429–436. https://doi.org/10.15585/MMWR.MM7111E2
Chen J, Wang R, Gilby NB, Wei GW (2022) Omicron variant (B.1.1.529): Infectivity, vaccine breakthrough, and antibody resistance. J Chem Inf Model 62:412–422. https://doi.org/10.1021/acs.jcim.1c01451
Author information
Authors and Affiliations
Contributions
L.K wrote the main manuscript text and prepared the table. G.P Revised the work and interpreted the data. S.S wrote the main manuscript text and prepared the table. All authors reviewed the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical Approval
The Internal Review Board named “Helsinki Committee” at Carmel Medical Center have approved the study. Approval Number: CMC-0032-22.
Consent to participate
Not applicable (retrospective study, all identifiable information of participants was removed from data).
Consent to publish
Not applicable (retrospective study, all identifiable information of participants was removed from data).
Guidelines
All the cases were encoded with numbers; All identifiable information of participants has been removed. All the research data are kept in a file in closed archive available only to the primary researcher.
Competing interests
The authors declare that they have no competing interests.
Additional information
Communicated by Tobias Tenenbaum.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khoury, L., Pillar, G. & Shehadeh, S. COVID-19 in neonates and infants younger than 6 months - a mild viral illness. Eur J Pediatr 182, 3287–3291 (2023). https://doi.org/10.1007/s00431-023-05016-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05016-x