Abstract
Understanding hospital service use among children with a diagnosis of craniosynostosis (CS) is important to improve services and outcomes. This study aimed to describe population-level trends, patterns, and factors influencing hospitalizations for craniosynostosis in Western Australia. Data on live births (1990–2010; n = 554,624) including craniosynostosis, episodes of death, demographic, and perinatal factors were identified from the midwives, birth defects, hospitalizations, and death datasets. Information on craniosynostosis and non-craniosynostosis-related admissions, cumulative length of hospital stay (cLoS), intensive care unit, and emergency department–related admissions were extracted from the hospitalization dataset and linked to other data sources. These associations were examined using negative binomial regression presented as annual percent change and associations of hospitalizations by age groups, demographic, and perinatal factors were expressed as incidence rate ratio (IRR). We found an increasing trend in incident hospitalizations but a marginal decline in cLoS for craniosynostosis over the observed study period. Perinatal conditions, feeding difficulties, nervous system anomalies, respiratory, and other infections contributed to majority of infant non-CS-related admissions.Respiratory infections accounted for about twice the number of admissions for individuals with CS (IRRs 1.94–2.34) across all observed age groups. Higher incidence of non-CS hospitalizations was observed among females, with associated anomalies, to families with highest socioeconomic disadvantage and living in remote areas of the state.
Conclusion: Marginal reduction in the cLoS for CS-related admissions observed over the 21-year period are potentially indicative of improved peri-operative care. However, higher incidence of respiratory infection-related admissions for syndromic synostosis is concerning and requires investigation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Children born with craniosynostosis (CS) often require early neurosurgical intervention, ideally between 4 and 13 months of age, with syndromic cases undergoing additional timed craniofacial corrections from childhood into early adulthood [1,2,3]. Extensive research has been conducted on techniques, costs, complications, and length of stay associated with surgical admissions for CS [4,5,6]. However, very little is known about the population-level trends and patterns of hospital admissions for craniosynostosis from childhood to early adulthood.
A previous Australian-based population-based study reported a stable trend in hospitalization rates and a marginal decrease in the average length of stay for people with craniosynostosis using the total population separation data from the publicly available Australia-wide National Hospital Morbidity Database [7]. However, these de-identified data were not linked to specific individuals, hence were unable to report on unit-level admissions, patterns of non-surgical admissions for craniosynostosis, provide procedure information for separations, or explain factors influencing admissions [7].
Given the knowledge gaps in the literature regarding the hospital service use for craniosynostosis, it is important to build comprehensive evidence to inform research, clinical and surgical practice, and planning and improve patient care. Hence, this study investigated trends, age-specific patterns, and factors influencing hospital admissions for people with craniosynostosis utilizing the Western Australian linked population data.
Methods
Study design and data sources
This retrospective cohort study utilized record-linked deidentified data from four data collections made available by the Western Australian Data Linkage System (WADLS). As a result of this linkage, each individual record is provided with a common unique identification number (linkage key) which was used to link the four data collections to facilitate the analysis.
Cases of craniosynostosis were principally identified from Western Australian Register of Developmental Anomalies (WARDA), with additional cases identified from the Hospital Morbidity Data Collection (HMDC). WARDA is a statutory population-based statewide register of congenital anomalies that identifies eligible cases using multiple sources of ascertainment. It includes structural and functional anomalies diagnosed in stillbirths and livebirths to six years of age [8]. Midwives Notification (MNS) collects information on all births attended by midwives in Western Australia (WA) with a gestational age ≥ 20 weeks or birth weight ≥ 400 g. Information on the Indigenous status, antenatal, and perinatal factors can also be extracted from this legislated surveillance system [9]. The Western Australian Death Registrations records all registered deaths and the associated cause of mortality [10]. The Hospital Morbidity Data Collection (HMDC) is a comprehensive collection of all hospital separations of admitted patients from all public and private hospitals in WA [11].
Study population
Our overall study population comprised all infants born in WA between 1990 and 2010 (21 years; n = 554,624). Among them, all infants born with craniosynostosis were largely identified from WARDA using the BPA-ICD9 codes with diagnostic descriptions for craniosynostosis (75600), Crouzon syndrome (75601), Apert syndrome (75550), Pfeiffer syndrome (75601), Carpenter syndrome (75984), Saethre-Chotzen syndrome (75550), Muenke syndrome (75600), and Baller-Gerold syndrome (75600)]. Some additional cases not identified in WARDA from 1998 onwards were extracted from the separation data of HMDC, provided the individual separation data had both a principal diagnostic code and procedure codes directly corresponding to craniosynostosis (Supplementary Fig. 1). The International Classification of Diseases-10th edition-Australian Modification (ICD-10-AM) diagnostic codes used included Q75.0 (Craniosynostosis), Q75.01 (coronal synostosis), Q75.02 (sagittal synostosis), Q75.03 (metopic synostosis), Q75.04 (multiple suture synostosis), Q75.09 (unclassified synostosis), and Q75.1 (craniofacial dysostosis). The Australian Classification of Health Interventions (ACHI) procedure codes for identifying craniosynostosis included 40115–00, 40118–00 [other procedure for craniosynostosis], and 45785–03 [total cranial vault reconstruction]. Considering the International Classification of Diseases-9th revision system-clinical modification (ICD-9-CM) codes do not specifically identify craniosynostosis, case identification from HMDC was restricted to births following the introduction of the ICD-10-AM system in 1998.
For analysis purposes, only cases of craniosynostosis identified from WARDA could be categorized according to syndromic status as follows: (i) non-syndromic (isolated single/multiple suture synostosis); (ii) syndromic synostosis (presence of additional anomalies).
The comparison cohort included all live-born individuals over the same period but not diagnosed with craniosynostosis. The comparison cohort was extracted from the MNS.
Outcome
The primary outcome of this study was the number of incident hospitalizations per total person-years. Individual person time under observation was obtained by subtracting either the final date of follow-up (i.e., December 31, 2010) or date of death, whichever occurred earlier, from the date of birth. The value was then summed among the study population to ascertain the total person-years. Hospitalizations in our study were defined as craniosynostosis or non-craniosynostosis-related admissions that included both surgical and non-surgical admissions. All principal diagnoses codes were mapped to the International Classification of Diseases-9th revision system-clinical modification (ICD-9-CM) codes and procedure codes (principal and additional procedure codes) to the Australian Classification of Health Interventions (ACHI) to allow comparisons across the study period.
Craniosynostosis-related admissions (CS-related) considered for this study included surgical and non-surgical admissions that were identified using principal diagnostic codes for craniosynostosis or where relevant principal and additional procedure codes, indicating craniosynostosis repair regardless of principal diagnosis code (Supplementary Table 1). Procedures were broadly grouped into two categories: (i) neurosurgical interventions; (ii) cranio-maxillofacial interventions (Supplementary Table 1).
All admissions not categorized as craniosynostosis-related were broadly considered as non-craniosynostosis (non-CS) related. We specifically considered admissions for ocular, auricular, dental, respiratory infections, other respiratory conditions, and sleep-related disorders reasons separately as these admissions are common or previously reported among children with craniosynostosis [12]. Furthermore, as was done previously [13], we identified post-operative complications after craniosynostosis surgery by different principal diagnostic codes for infection, wound disruption, hemorrhage, dural tear, and cerebrospinal fluid (CSF) leak (Supplementary Table 2).
Secondary outcomes for this study were as follows:
-
(a)
Length of stay: calculated as the time between admission and discharge. The length of hospital stay was considered as 0.5 days when the admission and discharge occurred on the same day to reflect some period of hospitalization [14]. We reported the cumulative length of stay (cLoS) in this study, which was the total number of admitted days for an individual.
-
(b)
Frequency of intensive care unit (ICU) admissions: data were extracted from the HMDC and additionally included individual length of stay in intensive care.
-
(c)
Frequency of emergency department (ED) admissions: this information was collected from the HMDC.
Covariates
As was done previously [15, 16], information on demographic factors (infant sex, birth year and Indigenous status, remoteness of residence, socioeconomic disadvantage) and perinatal factors (parity, plurality, gestational age, birth weight, and fetal distress, intrauterine growth restriction and percentage of optimal head circumference) for case and comparison cohorts was collected from the MNS.
Statistical analysis
Descriptive statistics were used to summarize the frequency of admitted individuals (craniosynostosis and non-craniosynostosis-related), intensive care admissions, and emergency admissions. Linear trends in hospitalizations adjusted for age at separation, sex, Indigenous status, remoteness, and socioeconomic disadvantage were estimated using negative binomial regression, and annual percent change (APC) was reported. The APC was calculated by exponentiating the coefficient of the year of birth and then subtracting 1 [17].
Furthermore, we conducted the analysis by type of craniosynostosis (non-syndromic and syndromic) for four age groups. As was done previously [18], the four age groups included infancy (up to 1 year), toddler and preschool (from 1 up to 5 years), primary school (from 5 up to 12 years), adolescence and early adulthood (12 to 21 years). Association of incident hospitalizations per total person-years (all hospitalizations, craniosynostosis and non-craniosynostosis-related) and cumulative length of stay with the type of craniosynostosis adjusted for sex, Indigenous status, remoteness, socioeconomic disadvantage, and birth year were calculated using negative binomial regression and reported as an incidence rate ratio (IRR) and 95% confidence intervals (CI).
A similar modeling approach was used to determine the association between each relevant explanatory variable (demographic and perinatal factors) and hospitalizations (all-cause, craniosynostosis and non-craniosynostosis-related) and IRRs with 95% CIs were reported. All analyses were carried out using Stata 16.0 (Stata Corp, College Station, TX, USA).
As done in our previous work involving missing data, a complete case analysis was also used in this study (Supplementary Table 3) as we assumed the mechanism of missingness to be missing at random [15, 16].
This study was performed in line with the principles of the Declaration of Helsinki. The protocol was approved by the Human Research Ethics Committee of the WA Department of Health (HREC#2011/64), Western Australian Aboriginal Health Ethics Committee (HREC#2015/613) and The University of Western Australia (RA/4/20/5843).
Results
As presented in Table 1, nearly all (96.9%) individuals with craniosynostosis were hospitalized. Ten individuals had no admission records during the study period. Furthermore, under 5% (4.3%; 14/322) of CS individuals, all of whom had syndromic conditions, died at any given point during the study period. Mean incident hospitalizations was lowest for non-syndromic lambdoid synostosis and the highest for Apert syndrome (Table 1).
The median cumulative length of stay (cLoS) was lowest for those with non-syndromic coronal synostosis and highest for those with Apert syndrome. Furthermore, about three-fifths of the admitted individuals with CS had an emergency admission, and more than two-fifths required intensive care (Supplementary Table 4). While the median cumulative length of stay for individuals with CS in intensive care was only one day (IQR 1,16), children with Crouzon syndrome, on average, spent a total of 53 days (IQR 37, 58) in intensive care (Supplementary Table 4).
Trends of hospital admissions and cumulative length of stay
A steady increase in individual hospitalizations for both case and comparison cohort, including all-cause, CS, and non-CS-related admissions was observed over the study period. The incident hospitalizations were twice as high for craniosynostosis [IRR 2.04 (95% CI 1.94, 2.14)], more pronounced for syndromic CS, than those born without this condition (Table 1).
We observed a marginal decline in the trend for the cumulative length of stay for all-cause and CS-related hospitalizations [APC − 1.10 (95% CI − 3.23, 1.08)] prominently for non-syndromic CS but not for non-craniosynostosis-related admissions. Individuals with craniosynostosis spent three and a half times more total days in hospital for any cause [IRR 3.56 (95% CI 3.07, 4.12] than those without (Supplementary Table 4).
Patterns of hospital admissions and cumulative length of stay by age group
While the frequency of all-cause hospitalizations, CS-related and non-CS-related, ICU, and ED hospitalizations declined with increasing age, non-CS-related admissions contributed to a larger proportion of all admissions for ages after infancy (Table 2). This declining pattern was more pronounced for non-syndromic CS. Furthermore, we observed limited instances of post-operative complications, most of which occurred during the first 5 years of life (Table 2).
With respect to surgical admissions, half [50.0%] of children with CS aged up to 5 years undergoing neurosurgical interventions required intensive care. The requirement of intensive care after cranio-maxillofacial interventions was proportionally about 30% higher than neurosurgical admissions for the same age group (Supplementary Table 5).
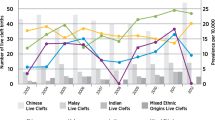
As presented in Table 3, perinatal conditions, other congenital anomalies, and feeding difficulties contributed to a large share of infant admissions, among other non-CS-related reasons. Respiratory infections contributed to about twice the number of hospital admissions for children with CS, especially syndromic CS, for all observed age groups compared to those without (Table 3). Furthermore, males with non-syndromic CS had higher rates of hospitalizations for respiratory infections than females which was contrary to syndromic CS were females had higher hospitalization rates than males (Supplementary Fig. 2). Hospital admissions for oral health–related reasons were also nearly three times higher among children with CS aged between 5 and 12 years relative to those without CS. We also observed that nearly three-fifths of all non-synostosis admissions were recorded as emergency admissions which were even higher for syndromic CS (Table 3). Furthermore, among non-craniosynostosis admissions, perinatal, other respiratory conditions (including asthma), and respiratory infections contributed to a large share of emergency admissions across age groups (Fig. 1).
Factors influencing hospital admission patterns
All-cause hospitalizations for females with craniosynostosis were 1.46 times (95% CI 1.31, 1.61) higher than for males (Table 4). Furthermore, the most socioeconomically disadvantaged quintile had a 32% greater increase in all-cause hospitalizations [IRR 1.32 95% CI 1.13, 1.55], especially non-CS admissions, than those in the highest quintile (Table 4). Being born preterm increased the risk of both synostosis and non-synostosis-related admissions relative to those born at term. Similarly, low birth weight, greater intrauterine growth restriction, and presence of fetal distress increased the incidence of hospitalizations, especially non-synostosis-related, for individuals with CS, more so for those with syndromic conditions (Table 4).
Discussion
This study provides comprehensive population-based information on the hospitalization burden of craniosynostosis in Western Australia. Our findings indicate an increasing trend in incident hospitalizations for craniosynostosis but a marginal decline in the cumulative length of hospital stay for the observed 21 years. Furthermore, respiratory infections accounted for about twice the number of admissions for individuals with CS across all observed age groups. We also observed a higher incidence of non-CS-related hospitalizations among females, children born preterm, severe intrauterine growth restriction, with syndromic CS, and to families with greatest socioeconomic disadvantage.
There are limited population studies describing patterns of hospitalization for craniosynostosis and other rare craniofacial anomalies. The use of population data to describe the changing trends and age-specific patterns of individual-level hospitalizations is a strength of this study. Furthermore, the ability to link to the midwives registry provided the opportunity to explore the association of demographic and perinatal factors with the incidence of admissions. Considering the inclusivity of this linked data, we were able to avoid any chance of selection bias.
Despite the strengths, there were some limitations to this study. The administrative coding for craniosynostosis in the hospital system is not nuanced, and hence we cannot identify or report individual differences in case severity or treatment protocols followed. However, admissions related to different types of CS and procedure information were better coded with the ICD-10-AM diagnosis and ACHI procedure codes than in the earlier systems of coding using ICD-9-CM and the International Classification of Procedures in Medicine.
The marginal reduction in the cumulative length of stay for CS-related admissions which we observed in our cohort was similar to the findings from the national hospital separation data for craniosynostosis [7]. The observed marginal reduction in the cumulative length of stay in our data could also indicate efficiency and improved quality of hospital care [19]. However, we observed an increasing trend in all-cause, CS and non-CS-related hospitalizations in our cohort despite stable trends observed both for reported birth prevalence in WA and national hospital separation data on craniosynostosis [7, 15]. The increasing trends in hospitalization for craniosynostosis-related reasons may relate to the establishment of a specialized craniofacial unit during the observed time period (1993) [Dr Timothy Hewitt, Perth Children’s Hospital, personal communication, 10.01.2022] and changing treatment practices given the growth of a specialized surgical workforce.
A large proportion of CS-related admissions took place during infancy which is in line with the ideal age for neurosurgical intervention [1]. However, admissions for children aged one to five years in our cohort might relate to multiple issues. These include potential delayed diagnosis, increased waiting times, delayed scheduling of surgery especially for syndromic CS, postsurgical complications, and requirement of continued management for specific rare syndromic conditions [20,21,22]. We observed a substantial decline in admissions, especially for CS-related reasons for children (especially non-syndromic CS) over the age of five, similar to the pattern observed with national hospital separation data for craniosynostosis [7]. This admission pattern is expected for craniosynostosis, considering most single-suture synostosis have fewer CS-related service contacts with increasing age as a result of better surgical outcomes [23]. However, individuals born with syndromic craniosynostosis have prolonged service contacts for managing additional associated anomalies [22].
We observed higher proportions of ICU admissions and cLoS for cranio-maxillofacial interventions than neurosurgical interventions. For syndromic craniosynostosis, a large majority of patients require airway/midface procedures warranting intensive care admission because of potential airway issues [22]. However, cases undergoing neurosurgical interventions are often extubated the day of surgery, observed overnight in intensive care, and discharged [24]. Furthermore, the length of stay for cranio-maxillofacial intervention is longer, especially for cases with any specific airway issues [25]. Nevertheless, this finding can be confounded by admissions to high dependency units or the presence of a specialist nurse in wards which can potentially reduce the requirement of ICU admissions [26,27,28].
Respiratory infections contributed to twice as many admissions among individuals with CS and occurred more often in those with syndromic CS across all observed age groups than in those without. While acute lower respiratory infections have been reported to be higher among children with any birth defects, children born with syndromic CS specifically present with midfacial deficiencies and micrognathia, which could increase their susceptibility to respiratory infections [29, 30].
We also observed a higher incidence of hospitalizations, especially for non-CS-related reasons, in females than males, despite the birth prevalence of CS among males being greater than females [15]. Further research is required to explore this sex-related disease severity. It is widely acknowledged that preterm and low birth weight children have higher hospital service contacts, especially during infancy [31]. Considering children with craniosynostosis have a higher chance to be born preterm, with low birth weight, intrauterine growth restrictions, and fetal distress than children born without [15], the higher incidence of hospitalizations among this cohort is largely predictable. While the association between socioeconomic disadvantage and the birth prevalence of craniosynostosis in WA is unclear [15], we found those belonging to families with the highest socioeconomic disadvantage were more frequently admitted, especially for non-craniosynostosis reasons. Previous WA population studies have shown increased hospital service use, especially for respiratory infections among socially disadvantaged children not born with any birth defects [32, 33]. We believe a similar pattern exists for our cohort and requires further investigation.
In the future, from a research standpoint, it will be critical that health system coding is nuanced to accommodate more intricate details related to different craniosynostosis types, associated underlying and comorbid rare diseases, and different surgical techniques.
Conclusion
Our study provides a longitudinal, population-level description of all individual-level hospitalizations for craniosynostosis in Western Australia and emphasizes the increased hospital service needs for those born with this condition relative to those born without. This hospital service use for individuals with craniosynostosis was higher for females, with greater socioeconomic disadvantage, born preterm, with syndromic conditions, low birth weight, intrauterine growth restriction, and fetal distress. The higher incidence of respiratory infections across age groups for syndromic synostosis is concerning and requires further investigation.
Data Availability
Due to the nature of the research [ethical/legal/commercial reasons] supporting data is not available.
References
Bruce WJ, Chang V, Joyce CJ, Cobb AN, Maduekwe UI, Patel PA (2018) Age at time of craniosynostosis repair predicts increased complication rate. Cleft Palate Craniofac J 55:649–654. https://doi.org/10.1177/1055665617725215
Mehta VA, Bettegowda C, Jallo GI, Ahn ES (2010) The evolution of surgical management for craniosynostosis. Neurosurg Focus 29(6):E5. https://doi.org/10.3171/2010.9.FOCUS10204
Proctor MR, Meara JG (2019) A review of the management of single-suture craniosynostosis, past, present, and future: JNSPG 75th Anniversary Invited Review Article. J Neurosurg Pediatr 24:622–631. https://doi.org/10.3171/2019.7.PEDS18585
Garber ST, Karsy M, Kestle JRW, Siddiqi F, Spanos SP, Riva-Cambrin J (2017) Comparing outcomes and cost of 3 surgical treatments for sagittal synostosis: a retrospective study including procedure-related cost analysis. Neurosurgery 81:680–687. https://doi.org/10.1093/neuros/nyx209
Wu SS, Cai Y, Sunshine K, Boas SR, Kumar AR (2021) Evaluating the effects of enhanced recovery pathways in craniosynostosis: national trends in hospitalization charges and length of stay in craniosynostosis surgery. Ann Plast Surg 87. https://doi.org/10.1097/SAP.0000000000002808
Yan H, Abel TJ, Alotaibi NM, Anderson M, Niazi TN, Weil AG, Fallah A, Phillips JH, Forrest CR, Kulkarni AV et al (2018) A systematic review and meta-analysis of endoscopic versus open treatment of craniosynostosis. Part 1: the sagittal suture. J Neurosurg Pediatr 22:352–360. https://doi.org/10.3171/2018.4.PEDS17729
Junaid M, Slack-Smith L, Wong K, Baynam G, Calache H, Hewitt T, Leonard H (2022) Epidemiology of hospital admissions for craniosynostosis in Australia: a population-based study. Cleft Palate Craniofac J. https://doi.org/10.1177/105566562210742
Women and Newborn Health Service (2015) Department of Health, Government of Western Australia. Western Australian Register of Developmental Anomalies 1980 – 2014
Department of Health (2019) Government of Western Australia. Midwives Notification System. Available from https://ww2.health.wa.gov.au/Articles/J_M/Midwives-Notification-System
Holman CD, Bass AJ, Rouse IL, Hobbs MS (2019) Population-based linkage of health records in Western Australia: development of a health services research linked database. Aust N Z J Public Health 23:453–459. https://doi.org/10.1111/j.1467-842X.1999.tb01297.x
Department of Health, Government of Western Australia. Hospital Morbidity Data System (2019) Reference manual. Part A: Contacts, hospital responsibilities, data element definitions. In: Department of Health, editor. Perth, Western Australia.: Government of Western Australia. https://ww2.health.wa.gov.au/~/media/Files/Corporate/general-documents/Clinical-Information-Assurance/Part-A-HMDS-Ref-Manual-2018-19.pdf
Sun B, Cloonan YK, Collett BR, Speltz ML (2017) Sleep outcomes in children with single-suture craniosynostosis compared with unaffected controls. Cleft Palate Craniofac J 54:734–738. https://doi.org/10.1597/16-090
Lin Y, Pan IW, Mayer RR, Lam S (2015) Complications after craniosynostosis surgery: comparison of the 2012 Kids’ Inpatient Database and Pediatric NSQIP Database. Neurosurg Focus 39:E11. https://doi.org/10.3171/2015.9.FOCUS15383
Colvin L, Bower C (2009) A retrospective population-based study of childhood hospital admissions with record linkage to a birth defects registry. BMC Pediatr 9:32. https://doi.org/10.1186/1471-2431-9-32
Junaid M, Slack-Smith L, Wong K, Bourke J, Baynam G, Calache H, Leonard H (2022) Epidemiology of rare craniofacial anomalies: retrospective western Australian population data linkage study. J Pediatr 241:162-172.e9. https://doi.org/10.1016/j.jpeds.2021.09.060
Junaid M, Slack-Smith L, Wong K, Bourke J, Baynam G, Calache H, Leonard H (2022) Association between craniofacial anomalies, intellectual disability and autism spectrum disorder: Western Australian population-based study. Pediatr Res 92:1795–1804. https://doi.org/10.1038/s41390-022-02024-9
Glasson EJ, Wong K, Leonard H, Forbes D, Ravikumara M, Mews C, Jacoby P, Bourke J, Trollor J, Srasuebkul P et al (2018) Evolving trends of gastrostomy insertion within a pediatric population. J Pediatr Gastroenterol Nutr 67:e89-e94. https://doi.org/10.1097/MPG.0000000000002042
Bell J, Nassar N, Turner R, Bower C, Gillett D, McBain W, Raynes-Greenow C (2016) Hospitalisations up to adulthood for children born with orofacial clefts. J Paediatr Child Health 52(4):441–448. https://doi.org/10.1111/jpc.13024
Australian Institute of Health and Welfare (2020) Australia’s hospitals at a glance 2018–19. Canberra: AIHW
Abraham P, Brandel MG, Dalle Ore CL, Reid CM, Kpaduwa CS, Lance S, Meltzer HS, Gosman AA (2018) Predictors of postoperative complications of craniosynostosis repair in the national inpatient sample. Ann Plast Surg 80:S261–S266. https://doi.org/10.1097/SAP.0000000000001383
Australian Institute of Health and Welfare (2018) Elective surgery waiting times 2017–18: Australian hospital statistics. Health services series no. 88. Cat. no. HSE 215. Canberra: AIHW
Mathijssen IM (2015) Guideline for care of patients with the diagnoses of craniosynostosis: working group on craniosynostosis. J Craniofac Surg 26:1735–1807. https://doi.org/10.1097/SCS.0000000000002016
Fearon JA, McLaughlin EB, Kolar JC (2006) Sagittal craniosynostosis: surgical outcomes and long-term growth. Plast Reconstr Surg 117:532–541. https://doi.org/10.1097/01.prs.0000200774.31311.09
Bonfield CM, Basem J, Cochrane DD, Singhal A, Steinbok P (2018) Examining the need for routine intensive care admission after surgical repair of nonsyndromic craniosynostosis: a preliminary analysis. J Neurosurg Pediatr 22:616–619. https://doi.org/10.3171/2018.6.PEDS18136
Nguyen C, Hernandez-Boussard T, Khosla RK, Curtin CM (2013) A national study on craniosynostosis surgical repair. Cleft Palate Craniofac J 50:555–560. https://doi.org/10.1597/11-324
Boots R, Lipman J (2002) High dependency units: issues to consider in their planning. Anaesth Intensive Care 30:348–354. https://doi.org/10.1177/0310057X0203000314
Fukuda T, Sakurai H, Kashiwagi M (2020) Impact of having a certified nurse specialist in critical care nursing as head nurse on ICU patient outcomes. PLoS One 15:e0228458. https://doi.org/10.1371/journal.pone.0228458
Gould A, Ho KM, Dobb G (2010) Risk factors and outcomes of high-dependency patients requiring intensive care unit admission: a nested case-control study. Anaesth Intensive Care 38:855–861. https://doi.org/10.1177/0310057X1003800508
Jama-Alol KA, Moore HC, Jacoby P, Bower C, Lehmann D (2014) Morbidity due to acute lower respiratory infection in children with birth defects: a total population-based linked data study. BMC Pediatr 14:80. https://doi.org/10.1186/1471-2431-14-80
Koppel D, Grant J (2021) Modern Management of Craniosynostosis (2021). In: Bonanthaya K, Panneerselvam E, Manuel S, Kumar VV, Rai A (eds) Oral and maxillofacial surgery for the clinician. Springer Singapore, Singapore, pp 1813–1841
Miller JE, Hammond GC, Strunk T, Moore HC, Leonard H, Carter KW, Bhutta Z, Stanley F, de Klerk N, Burgner DP (2016) Association of gestational age and growth measures at birth with infection-related admissions to hospital throughout childhood: a population-based, data-linkage study from Western Australia. Lancet Infect Dis 16:952–961. https://doi.org/10.1016/S1473-3099(16)00150-X
Barnes R, Blyth CC, de Klerk N, Lee WH, Borland ML, Richmond P, Lim FJ, Fathima P, Moore HC (2019) Geographical disparities in emergency department presentations for acute respiratory infections and risk factors for presenting: a population-based cohort study of Western Australian children. BMJ Open 9:e025360. https://doi.org/10.1136/bmjopen-2018-025360
Strobel NA, Peter S, McAuley KE, McAullay DR, Marriott R, Edmond KM (2017) Effect of socioeconomic disadvantage, remoteness and Indigenous status on hospital usage for Western Australian preterm infants under 12 months of age: a population-based data linkage study. BMJ Open 7:e013492. https://doi.org/10.1136/bmjopen-2016-013492
Acknowledgements
The authors also wish to thank the Linkage and Client Services Teams at the Western Australian Data Linkage Branch, as well as the custodians for the following data collections: Western Australian Register of Developmental Anomalies (WARDA)-Birth Defects, Midwives Notification System (MNS) and WA Death Registrations.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. Mohammed Junaid is being supported by the Australian Government International Research Training Program Scholarship and the Stan and Jean Perron Top-Up Scholarship.
Author information
Authors and Affiliations
Contributions
MJ, LSS, and HL conceptualized this study. MJ, LSS, TH, JB, GB, and HL planned the data analysis, participated in drafting, and reviewing the manuscript. MJ and KW were involved in the data analysis. MJ led writing of paper, and all authors contributed to drafting and reviewing the manuscript and have read and approved the final document.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. The protocol was approved by the Human Research Ethics Committee of the WA Department of Health (HREC#2011/64), Western Australian Aboriginal Health Ethics Committee (HREC#2015/613), and The University of Western Australia (RA/4/20/5843).
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Gregorio Milani.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Junaid, M., Slack-Smith, L., Wong, K. et al. Patterns, trends, and factors influencing hospitalizations for craniosynostosis in Western Australia. A population-based study. Eur J Pediatr 182, 2379–2392 (2023). https://doi.org/10.1007/s00431-023-04922-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04922-4