Abstract
Children with elevated liver enzymes are occasionally discovered through laboratory work-up from different clinical scenarios. Although the majority will have transient and/or benign conditions, a subgroup will have underlying liver disorders. The differential diagnosis is broad and therefore, a systematic approach is of utmost importance. In this article, we reviewed the most recent and relevant literature to provide a comprehensive overview of the main disease processes that cause hypertransaminasemia in children. Ultimately, we propose a practical stepwise approach to guide primary care physicians in the evaluation of abnormal liver enzymes in asymptomatic children. The first step is to obtain a complete history along with a thorough physical examination to exclude red flags, which should dictate urgent consultation with a paediatric gastroenterologist or hepatologist.
Conclusion: Hypertransaminasemia is a challenging scenario in the primary care setting. The aetiology can be broad, ranging from hepatic and extrahepatic to transient versus chronic liver disease. Timely referral to a specialised centre is of paramount importance for conducting targeted research and to not miss the chance of identifying a progressive, but still asymptomatic, treatable liver disease.
What is Known: • Elevated liver enzyme is a challenging scenario in the primary care setting. • There are few studies guiding the evaluation of asymptomatic hypertransaminasemia in the paediatric population and a standardised approach is lacking. | |
What is New: • We propose a practical stepwise approach to guide primary care physicians in the evaluation of abnormal liver enzymes. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary care physicians are increasingly faced with elevated liver enzymes found in a laboratory work-up from different scenarios, both in symptomatic and asymptomatic patients [1,2,3,4,5]. Although the majority will have benign conditions, a subgroup will have underlying liver disorders that will require appropriate investigations. In adults, the causes of elevated liver enzymes, other than viral hepatitis and obesity-related liver disease, are more liver-specific and its evaluation is well-stablished in the literature [6, 7]. In the paediatric population, liver diseases gather a large spectrum of diagnoses, from hepatic and non-hepatic aetiologies to multisystemic disorders, making them a challenge for primary care physicians [1].
Several studies report that the prevalence of abnormal liver enzymes varies according to the country, type of food, sanitation conditions, time of the year, and the quality of healthcare [3]. It is estimated that between 3.5 and 12.4% of asymptomatic adolescents have elevated liver enzymes [3, 8,9,10]. The most common cause in underdeveloped countries is infection, mainly caused by hepatitis A virus (HAV) [3]. On the other hand, in developed countries, non-alcoholic fatty liver disease (NAFLD) is the leading cause, although hepatobiliary, genetic, and autoimmune disorders are important contributors [6, 11]. However, the prevalence and aetiology of hypertransaminasemia in European children from all age groups are not well-known, probably because the condition is underestimated [4]. In addition, there are few studies guiding the evaluation of the asymptomatic hypertransaminasemia in the paediatric population and a standardised approach in the primary care setting is lacking.
The aim of this article is to provide a comprehensive overview of the basic disease processes that cause hypertransaminasemia in children. Then, we developed a stepwise algorithm to guide primary care physicians in the evaluation of abnormal liver enzymes in asymptomatic children. The first step is to obtain a complete history and perform a thorough physical examination in an effort to exclude the presence of red flags [12]. In these cases, timely referral to a specialised centre is of paramount importance so as not to miss the chance of identifying progressive, but still asymptomatic, treatable liver disease [4, 6].
Keywords in paediatric hepatology
Markers of cytolysis: aspartate aminotransferase (AST) and alanine aminotransferase (ALT)
Aminotransferases (transaminases) are intracellular enzymes found in various tissues at different proportions and normally found in the plasma in low levels [3]. AST is found, in decreasing order of concentration, in the liver, heart, skeletal muscle, kidneys, brain, pancreas, lungs, leukocytes, and erythrocytes, and its half-life in circulation is about 17 − 18 h [1, 5, 7, 13, 14]. ALT is found in low concentrations in other tissues beyond the liver, making this enzyme more specific of liver injury. Its half-life is longer than that of AST (45 − 47 h) [1, 5, 13]. In clinical settings, their elevation occurs due to the enzyme leakage following cell damage or change in cell membrane permeability [15] in those tissues. Thus, the aetiology can be broad, ranging from hepatic and extrahepatic to transient versus chronic liver disease. Additionally, the degree of AST and ALT elevation does not always correlate with the degree of hepatocellular damage [3, 6, 7, 16].
Markers of cholestasis: bilirubin, bile acids, alkaline phosphatase (ALP), and g-glutamyl transferase (GGT)
Unconjugated bilirubin is a heme degradation product transported to the liver and conjugated by the UDP-glucuronyl transferase into a water-soluble form—conjugated/direct bilirubin—secreted across the canalicular membrane into the bile [14]. Increase in conjugated bilirubin is due to decreased excretion into the bile and leakage from the hepatocytes into the serum and may result from impairment of the hepatocyte’s canalicular membrane, damage to the canaliculi, and/or obstruction of extrahepatic bile ducts [17].
ALP is an enzyme that is responsible for transportation of metabolites across the cell membrane. Under normal conditions, it is predominantly of liver and bone origin. Elevation of ALP levels can be present in several hepatic and non-hepatic processes. In hepatobiliary diseases, ALP elevation results from increased de novo synthesis in the liver followed by release into the circulation. Retained bile acids appear to play a central role in this process [14].
Gamma glutamyl-transferase (GGT) is located on the membrane of cells with high secretory or absorptive activities, being more abundant in the liver, kidney, pancreas, intestine, and prostate, but not in bone. Its activity can be useful to determine whether an elevation of alkaline phosphatase is of liver or bone origin. High ALP levels in conjunction with elevated GGT point to cholestatic disorders with hepatobiliary injury (e.g. primary sclerosing cholangitis) [14].
Liver function tests
The liver synthesises both albumin and many of the blood coagulation factors required to produce a normal prothrombin time. Thus, serum albumin and prothrombin time are essential tests when assessing liver function, although not liver-specific.
The half-life of serum albumin is around 19 to 21 days, whereas the half-life of blood coagulation factor may be less than 1 day, so these tests, along with physical examination findings, can be used to assess both acute and chronic liver dysfunctions [14].
The liver plays a fundamental role in the detoxification of the human body, and ammonia, the final product of the urea cycle, is the utmost illustrative metabolite of this role. Increased serum ammonia levels may result from substrate overload and/or decreased ability to metabolise and eliminate, and they are usually associated with variable degrees of encephalopathy [18].
Transaminase reference values
In common practice, reference ranges are defined as the mean value within ± 2 standard deviations obtained in healthy individuals [5, 6]. By definition, we should consider hypertransaminasemia as an elevation of liver enzymes greater than 1.5 to 2 times the upper limit or higher than the 97th percentile, which is a difficult definition to apply in the paediatric population [13], mainly because of the high variability of ALT and AST with age, sex, weight, time of day, and level of exercise [2, 5, 19]. For an ALT reference range, England et al. [20] proposed ALT centiles stratified by sex and age in a healthy European population as shown in Table 1. AST and GGT also reveal sex-specific differences and age-dependent fluctuations [21, 22].
The magnitude of aminotransferase alterations can be classified as ‘mild’ (2 − 5 times the upper reference limit), ‘moderate’ (5 − 10 times the upper reference limit), or ‘marked or severe’ (> 10 times the upper reference limit) [5, 6, 13]. Mild or moderate hypertransaminasemia is often seen with chronic liver disease (e.g. chronic viral hepatitis, nonalcoholic steatohepatitis), although transient elevations may also be seen in children with mild hepatic insults [13]. For patients with severe elevations of serum aminotransferases, markers of liver failure should be promptly excluded.
Understanding the scope of elevated liver enzymes
Elevated liver enzymes are often a challenging scenario in common clinical practise. Although a normal physiological phenomenon in certain instances, it may also reflect liver disease. The differential diagnosis is broad; however, it is not intended that primary care providers pursue extensive evaluations and work-up. We believe that primary care providers should be aware of the main disease processes affecting each age group, as they have a pivotal role in the referral of these patients for further assessment and management. Conversely, missing the referral of mild or moderate liver enzyme elevations could mean missing a progressive, yet treatable, condition.
To guide primary care clinicians in the interpretation of elevated liver enzymes in asymptomatic children, we can divide the main causes into hepatic and extrahepatic (Table 2) and consider the most prevalent diseases in each age group (Fig. 1) to help with the selection of the most appropriate complementary tests.
Causes of hepatic origin
-
(I)
Non-alcoholic fatty liver disease
NAFLD has emerged as the most common cause of hypertransaminasemia in children and adolescents in developed countries with a prevalence that rounds 2.6 − 9.8% [23]. The increased burden of NAFLD is strongly related to the increase in fructose consumption, overweight/obesity, and metabolic syndrome [23,24,25,26]. It usually affects children older than 10 years and rarely appears under 3 years. In this age group, NAFLD should alert for secondary causes, such as endocrine disorders or inborn errors of metabolism.
NASPGHAN guidelines define the screening for NAFLD in obese children (BMI ≥ 95 percentile) between 9 and 11 years old or overweight children (95 < BMI ≥ 85 percentile) with risk factors such as hypertension, hyperinsulinemia, hypertriglyceridemia, hyperuricemia, and dyslipidaemia [26].
NAFLD represents a spectrum of fatty liver disease, encompassing three categories, defined by histologic findings: non-alcoholic fatty liver (NAFL), non-alcoholic steatohepatitis (NASH), and NASH cirrhosis. The utility of histology for routine clinical assessment of NAFLD is limited by its invasive nature. Thus, in clinical practice the diagnosis relies on either evidence of hepatic steatosis from imaging (mostly ultrasound) and/or elevations in serum aminotransferase levels, especially ALT [24, 26,27,28].
-
(II)
Viral infections
Hepatitis caused by viral infection due hepatotropic virus such as A, B, C, E, and non-A-E virus, as well as other viral systemic febrile infections, is a common cause of hypertransaminasemia. In developing countries, infections are one of the main causes of abnormal transaminases levels, especially hepatitis A (HAV). Consequently, ethno-geographic origin and other risk factors for infection should be carefully assessed, such as vaccination status, history of blood product transfusion, sexual behaviour, tattooing, or ingestion of potentially contaminated food [3, 6, 23, 24, 29].
HAV is usually an acute and self-limited condition; fulminant hepatic failure occurs in fewer than 1 percent of cases [29, 30]. HAV infection is preventable via vaccination, but outbreaks still occur in countries with high endemicity such us Middle East and Northern African region. AST, ALT, GGT, and bilirubin rise as the infection starts and ALT rapidly increases before symptoms emerge. After that, ALT gradually decreases and normalises when jaundice disappears. However, in paediatric patients, HAV may be followed by up to 1 year of intermittent hypertransaminasemia due to relapsing viremia [6, 29, 30].
Most patients with chronic viral hepatitis have minimal elevations in ALT/AST levels, with a ratio of approximately 1 [17]. Hepatitis B (HBV) vaccination largely reduced the infection in children and mother-to-infant transmission; however, travel and immigration maintain an ample reservoir of HBV. Concerning hepatitis C (HCV), although less infectious than HBV, it remains a global issue in the absence of an effective vaccine [6]. In addition, paediatric HCV carriers may have fluctuating transaminase levels even in the presence of serious liver damage [6, 29, 30].
Other viral infections caused by hepatotropic non-A-E virus, such as Epstein-Barr, cytomegalovirus, adenovirus, coxsackievirus, enterovirus, herpes simplex, and rubella, should be considered in the appropriate clinical setting. Similarly, non-viral infections (bacteria or parasites) could also be the responsible agent [29, 31,32,33].
Coronavirus disease-19 (COVID-19) is the latest global pandemic caused by SARS-CoV-2 (severe acute respiratory syndrome). Although it predominantly causes respiratory symptoms, liver damage is among the main extrapulmonary manifestations. It typically leads to a temporary slight to moderate elevation of liver enzymes without significant hepatic synthetic function impairment [34, 35]. The mechanism of liver injury is related to the high ACE2 expression in cholangiocytes and hepatocytes, supporting the hypothesis of virus-related hepatic damage [36].
-
(III)
Drug-induced liver injury (DILI)
DILI is an important but often unrecognised cause of hypertransaminasemia in children. Most are subclinical with only laboratory abnormalities but can progress to a symptomatic or even a fulminant hepatitis [37]. Acetaminophen hepatotoxicity is a paradigmatic and well-documented example of predictable, dose-dependent injury; however, the majority of drugs causing DILI have idiosyncratic hepatotoxicity with variable latency periods, even in individuals with a long and previously uneventful exposure [37]. Antimicrobials (amoxicillin, amoxicillin-clavulanic, minocycline) and drugs acting on the central nervous system (antiepileptics, antidepressants, attention deficit hyperactivity disorder medications) represent most paediatric DILI cases. However, over-the-counter medications, herbal medicines, or even illicit drugs or substance abuse should be considered, especially in adolescents. Additionally, several drugs (e.g. minocycline, lamotrigine, azithromycin, or amoxicillin) can induce an idiosyncratic reaction with an immune-allergic component that resembles an autoimmune hepatitis. Thus, DILI diagnosis requires a high index of suspicion and a methodical exclusion of other paediatric liver diseases [3, 21, 26].
-
(IV)
Alpha1-antitrypsin deficiency
Alpha1 antitrypsin deficiency is an autosomal codominant disease that predisposes to lung and liver damage. Liver disease predominates in children but has a variable presentation depending on the disease phenotype. It may manifest with neonatal cholestasis in those with severe deficiency (e.g. PI ZZ phenotype) or with elevated liver enzymes in infancy and early childhood or cirrhosis with hepatosplenomegaly in the adolescent or young adult [38,39,40].
Screening tests involve detecting low levels of serum alpha-1 antitrypsin (A1AT). This measurement should be accompanied by an assessment of C-reactive protein, since A1AT is an acute-phase reactant protein that increases during infection or inflammation [41]. Phenotype determination is necessary to confirm the diagnosis [17]. Nevertheless, these patients should be referred to a tertiary paediatric centre for evaluation and follow-up.
-
(V)
Autoimmune liver disease (ALD)
ALD is a chronic progressive inflammatory liver disease that encompasses autoimmune hepatitis (AIH) and autoimmune sclerosing cholangitis (ASC). It is characterised by elevated transaminases and/or GGT levels, hypergammaglobulinemia, presence of specific autoantibodies, and a distinctive histology [6, 42].
ALD often shows a female to male predominance and is frequently associated with a family or personal history of concomitant autoimmune disorders [43]. It can present acutely with a clinical picture of hepatitis, or insidiously with a fluctuating course, either asymptomatically or with unspecific symptoms (fatigue, nausea, abdominal pain) [6, 42, 44]. Incidental elevation of transaminases or a cholestatic biochemical profile can be the only presenting feature. Establishing a definitive diagnosis is sometimes complex and cumbersome, and referral to a tertiary centre is recommended.
-
(VI)
Wilson disease (WD)
WD is an inherited autosomal recessive disorder of copper metabolism, involving a defect in ATP7B, resulting in impaired biliary copper excretion, leading to its accumulation, particularly in the liver and brain [45]. In childhood, WD has a predominant hepatic phenotype with an average age at presentation of 12 years [6, 46]. Liver disease may be completely asymptomatic, presenting with only mildly increased transaminases. Initial evaluation or screening includes testing for serum ceruloplasmin levels (reduced in most patients with WD) and 24-h urinary copper excretion. Definitive diagnosis requires liver biopsy and/or genetic tests [6, 46, 47]. Prompt treatment with copper-chelating agents and/or zinc hampers hepatic damage and/or prevents development of further neurological deterioration [6, 46, 48].
Elevated liver enzymes in multisystemic disorders
-
(I)
Celiac disease (CD)
CD is a systemic autoimmune disease due to dysregulated intestinal mucosal immune response in genetically susceptible individuals exposed to dietary gluten. Although it mainly affects the gut, many extraintestinal manifestations can arise. The liver involvement in CD is characterised by a mild to moderate increase of transaminases, often correlated to duodenal mucosal damage [49]. Normalisation of liver enzymes usually occurs within 12–24 months of a strict gluten-free diet and follows the decline in serum levels of anti-tissue transglutaminase [50,51,52]. In the case of persistent hypertransaminasemia, other possible causes of liver disease should be considered, mainly ALD [6, 52].
-
(II)
Inflammatory bowel disease (IBD)
IBD patients may present with elevated liver enzymes resulting from the disease process itself, or the result of an underlying primary hepatic disorder such as ALD. Although less common, medication toxicity can also induce liver injury. The relation between IBD extent or duration and elevated liver enzymes is controversial; nevertheless, in the absence of concomitant disorders, low-grade elevations are usually transient [53,54,55].
-
(III)
Cystic fibrosis (CF)
CF is a progressive and multisystemic disease resulting from mutations in the cystic fibrosis transmembrane conductance receptor, expressed at the apical membrane of epithelial cells. Therefore, hepatobiliary disease in CF is the result of inspissated bile, causing ductular obstruction and hepatotoxicity. Although hepatic involvement is common, CF rarely has an exclusive hepatic presentation [56,57,58,59,60].
-
(IV)
Inborn errors of metabolism (IEM)
Newborn screening programs with tandem mass spectrometry are used in neonatal screening for several IEM [11] largely identified in the neonatal period. However, many patients will only present later in infancy or childhood, with a wide range of manifestations, and elevated liver enzymes can be the presenting sign. Although individually rare, IEM collectively account for 20 − 30% of liver disease in infancy and childhood [4, 61]. Important indicators of an IEM are consanguinity, previous miscarriages, dysmorphic features, developmental delay, and hepato(spleno)megaly. The diagnostic approach is cumbersome; thus, a high index of suspicion and discussion with a metabolic specialist centre is the key to diagnosis [4, 61, 62].
Main causes of elevated liver enzymes of non-hepatic origin
Elevated transaminases can signify extra-hepatic disorders, most commonly muscle diseases and haemolysis [7]. In the case of muscle disease, elevation of ALT and AST is accompanied by elevation in creatine kinase (CK), signalling muscle breakdown. Thus, CK is an easy and inexpensive marker that can be used as a screening process for muscular dystrophies in children with isolated ALT/AST elevation, in the presence of normal bilirubin and GGT serum levels [63]. CK elevation can also be caused by cellular necrosis induced by drugs or toxins and strenuous exercise [6, 64, 65].
Haemolysis can also be a cause of hypertransaminasemia, along with elevated unconjugated bilirubin, haptoglobin levels, and reticulocyte count.
Isolated elevation of AST in the presence of normal laboratory work-up suggests a diagnosis of macro-aspartate aminotransferase (macro-AST). Macro-AST complexes are formed from self-polymerization or binding to immunoglobulins, leading to decreased renal clearance and a false-positive elevation of AST [66]. The diagnosis of macro-AST is using polyethylene glycol (PEG) precipitation.
Diagnostic work-up
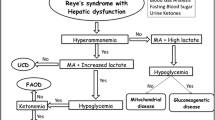
Investigating hypertransaminasemia is fundamental to diagnose treatable liver conditions and to institute specific treatment in a timely manner [6, 13, 16]. The proposed algorithm was designed to guide the approach in primary care facilities, highlighting some diagnostic considerations:
-
(a)
Exclude the presence of red flags, namely pallor, jaundice, hepatomegaly + / − splenomegaly, clinical signs of chronic liver disease (telangiectasias, abdominal collateral circulation, palmar erythema, digital clubbing), clinical or biochemical evidence of liver failure, and personal or family history of liver disease or autoimmune disease.
-
(b)
Discriminate between mild and moderate/severe liver enzyme elevation and manage accordingly:
-
Mild liver enzyme elevation should be re-assessed in 1–2 weeks. In the retesting panel, we should not only include ALT and AST, but also CK, LDH, and complete blood count to ensure that the enzymes are of liver origin, differentiating hepatic from extra-hepatic causes; GGT, bilirubin, albumin, total proteins, and coagulation tests are also valuable tests to guide subsequent management (Fig. 2)
-
Expedite referral of patients with evidence of liver dysfunction (high bilirubin, low albumin, and prolonged PT or INR)
-
Moderate or marked hypertransaminasemia in the context of a clear infectious aetiology must be re-assessed in 48–72 h. In the case of suspected drug-induced liver injury and in the absence of liver failure, the first step should be to stop any presumptive offenders (if possible) and re-evaluate the patient in the following days. Referral should be considered when either the medication cannot be stopped or no improvement is seen after a week. Patients with the possibility of delayed drug-induced hepatotoxicity and those with otherwise undefined circumstances should be referred.
-
-
(c)
We suggest concluding the follow-up of an asymptomatic patient with normal physical examination and normal values of liver function tests in the presence of two consecutive normal tests 1 month apart.
-
(d)
Articulation with a tertiary centre may be needed in all steps and consultation with a specialist is recommended in questionable cases.
Conclusion
Hypertransaminasemia is a challenging scenario in the primary care setting. Throughout this review, we summarised the most important causes of hypertransaminasemia in the paediatric population and proposed an accessible algorithm to guide clinical practise in primary care. Nevertheless, articulation with a tertiary centre is a valuable tool for conducting targeted research, optimising diagnostic resources, and offering the best patient care.
Abbreviations
- A1AT:
-
Alpha1-antitrypsin
- AIH:
-
Autoimmune hepatitis
- ASC:
-
Autoimmune sclerosing cholangitis
- ALD:
-
Autoimmune liver disease
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- CD:
-
Celiac disease
- COVID-19:
-
Coronavirus disease-19
- CF:
-
Cystic fibrosis
- CK:
-
Creatine kinase
- GGT:
-
G-glutamyl transferase
- DILI:
-
Drug-induced liver injury
- HAV:
-
Hepatitis A
- HCV:
-
Hepatitis C
- HBV:
-
Hepatitis B
- IBD:
-
Inflammatory bowel disease
- IEM:
-
Inborn errors of metabolism
- NAFL:
-
Nonalcoholic fatty liver
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH:
-
Non-alcoholic steatohepatitis
- WD:
-
Wilson disease
References
Costaguta A, Álvarez F (2014) El niño con hipertransaminasemia: ¿Cómo continuar? Arch Argent Pediatr 12(4):369–374
Musana KA, Yale SH, Abdulkarim AS (2004) Tests of liver injury. Clin Med Res 2(2):129–131
Serdaroglu F, Koca T, Dereci S, Akcam M (2016) The etiology of hypertransaminasemia in Turkish children. Bosn J Basic Med Sci 16(2):151–156
Iorio R, Sepe A, Giannattasio A, Cirillo F, Vegnente A (2005) Hypertransaminasemia in childhood as a marker of genetic liver disorders. J Gastroenterol 40(8):820–826
Giannini EG, Testa R, Savarino V (2005) Liver enzyme alteration: a guide for clinicians. CMAJ 172(3):367–379
Vajro P, Maddaluno S, Veropalumbo C (2013) Persistent hypertransaminasemia in asymptomatic children: a stepwise approach. World J Gastroenterol 19(18):2740–2751
Pratt D, Kaplan M (2000) Evaluation of abnormal liver-enzyme results in asymptomatic patients. N Eng J Med 342:1266–1271
Fraser A, Longnecker MP, Lawlor DA (2007) Prevalence of elevated alanine aminotransferase among US adolescents and associated factors: NHANES 1999–2004. Gastroenterology 133(6):1814–1820
Park SH, Park HY, Kang JW, Park J, Shin KJ (2012) Aminotransferase upper reference limits and the prevalence of elevated aminotransferases in the Korean adolescent population. J Pediatr Gastroenterol Nutr 55(6):668–672
Purcell M, Flores YN, Zhang ZF, Denova-Gutiérrez E, Salmeron J (2013) Prevalence and predictors of alanine aminotransferase elevation among normal weight, overweight and obese youth in Mexico. J Dig Dis 14(9):491–499
Moreira-Silva H, Maio I, Bandeira A, Gomes-Martins E, Santos-Silva E (2019) Metabolic liver diseases presenting with neonatal cholestasis: at the crossroad between old and new paradigms. Eur J Pediatr 178(4):515–523
Al-Busafi SA, Hilzenrat N (2013) Mild hypertransaminasemia in primary care. ISRN Hepatol 2013:1–6
Nobre S (2017) Criança assintomática com elevação das transaminases - algoritmo de investigação. Soc Port Gastroenterol Hepatol e Nutr Pediátrica 1–7
Green RM, Flamm S (2002) AGA technical review on the evaluation of liver chemistry tests. Gastroenterology 123(4):1367–1384
Hegarty R, Dhawan A (2018) Fifteen-minute consultation: the child with an incidental finding of elevated aminotransferases. Arch Dis Child Educ Pract Ed 103(5):228–230
Kohli R, Harris DC, Whitington PF (2005) Relative elevations of serum alanine and aspartate aminotransferase in muscular dystrophy. J Pediatr Gastroenterol Nutr 41(1):121–124
Malakouti M, Kataria A, Ali SK, Schenker S (2017) Elevated liver enzymes in asymptomatic patients – what should i do? J Clin Transl Hepatol 5(4):394–403
Squires JE, Alonso EM, Ibrahim SH, Kasper V, Kehar M, Martinez M et al (2022) North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition position paper on the diagnosis and management of pediatric acute liver failure. J Pediatr Gastroenterol Nutr 74(1):138–158
Stirnadel-Farrant HA, Galwey N, Bains C, Yancey C, Hunt CM (2015) Children’s liver chemistries vary with age and gender and require customized pediatric reference ranges. Regul Toxicol Pharmacol 73(1):349–355. https://doi.org/10.1016/j.yrtph.2015.07.013
England K, Thorne C, Pembrey L, Tovo PA, Newell ML (2009) Age-and sex-related reference ranges of alanine aminotransferase levels in children: European paediatric HCV Network. J Pediatr Gastroenterol Nutr 49(1):71–77
Schwimmer JB, Dunn W, Norman GJ, Pardee PE, Middleton MS, Kerkar N et al (2010) SAFETY study: alanine aminotransferase cutoff values are set too high for reliable detection of pediatric chronic liver disease. Gastroenterology 138(4):1357-1364.e2. https://doi.org/10.1053/j.gastro.2009.12.052
Bussler S, Vogel M, Pietzner D, Harms K, Buzek T, Penke M et al (2018) New pediatric percentiles of liver enzyme serum levels (alanine aminotransferase, aspartate aminotransferase, γ-glutamyltransferase): effects of age, sex, body massa index, and pubertal stage. Hepatology 1
Nobili V, Reale A, Alisi A, Morino G, Trenta I, Pisani M et al (2009) Elevated serum ALT in children presenting to the emergency unit: relationship with NAFLD. Dig Liver Dis 41(10):749–752
Bugeac N, Pacht A, Mandel H, Iancu T, Tamir A, Srugo I et al (2007) The significance of isolated elevation of serum aminotransferases in infants and young children. Arch Dis Child 92(12):1109–1112
Veropalumbo C, Del Giudice E, Esposito G, Maddaluno S, Ruggiero L, Vajro P (2012) Aminotransferases and muscular diseases: a disregarded lesson. Case reports and review of the literature. J Paediatr Child Health 48(10):886–890
Vos MB, Abrams SH, Barlow SE, Caprio S, Daniels SR, Kohli R et al (2018) HHS Public Access. 64:319–334
Janczyk W, Socha P (2012) Non-alcoholic fatty liver disease in children. Clin Res Hepatol Gastroenterol 36(3):297–300. https://doi.org/10.1016/j.clinre.2012.03.026
Vajro P, Lenta S, Socha P, Dhawan A, McKiernan P, Baumann U et al (2012) Diagnosis of nonalcoholic fatty liver disease in children and adolescents: position paper of the ESPGHAN hepatology committee. J Pediatr Gastroenterol Nutr 54(5):700–713
Kang KS (2013) Abnormality on liver function test. Pediatr Gastroenterol Hepatol Nutr 16(4):225–232
Chugh A, Maximos M, Perlman M, Gonzalez-Peralta RP (2016) Viral hepatitis in children: a through E. Pediatr Ann 45(12):e420–e426
Crum NF (2006) Epstein Barr Virus hepatitis: case series and review. South Med J 99(5):544–547
Bolis V, Karadedos C, Chiotis I, Chaliasos N, Tsabouri S (2016) Atypical manifestations of Epstein-Barr virus in children: a diagnostic challenge. J Pediatr (Versão em Port) 92(2):113–121. https://doi.org/10.1016/j.jpedp.2016.01.007
Demmler-Harrison GJ (2020) Overview of cytomegalovirus infections in children. UPTODATE
Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J et al (2020) Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol 115(5):766–773
Matthai J, Shanmugam N, Sobhan P (2020) Coronavirus disease (COVID-19) and the gastrointestinal system in children. Indian Pediatr 57(6):533–535
Gracia-Ramos AE, Jaquez-Quintana JO, Contreras-Omaña R, Auron M (2021) Liver dysfunction and SARS-CoV-2 infection. World J Gastroenterol 27(26):3951–3970
Amin MD, Harpavat S, Leung DH (2015) Drug-induced liver injury in children. Curr Opin Pediatr 27:625–633
Bornhorst JA, Greene DN, Ashwood ER, Grenache DG (2013) α1-Antitrypsin phenotypes and associated serum protein concentrations in a large clinical population. Chest 143(4):1000–1008. https://doi.org/10.1378/chest.12-0564
Townsend S, Newsome P, Turner AM (2018) Presentation and prognosis of liver disease in alpha-1 antitrypsin deficiency. Expert Rev Gastroenterol Hepatol 12(8):745–747. https://doi.org/10.1080/17474124.2018.1477589
Ruiz M, Lacaille F, Berthiller J, Joly P, Dumortier J, Aumar M et al (2019) Liver disease related to alpha1-antitrypsin deficiency in French children: the DEFI-ALPHA cohort. Liver Int 39(6):1136–1146
Strnad P, McElvaney NG, Lomas DA (2020) Alpha 1-antitrypsin deficiency. N Engl J Med 382(15):1443–1455
Porta G, de Carvalho E, Santos JL, Gama J, Borges CV, Seixas RBPM et al (2019) Autoimmune hepatitis in 828 Brazilian children and adolescents: clinical and laboratory findings, histological profile, treatments, and outcomes. J Pediatr (Rio J) 95(4):419–427. https://doi.org/10.1016/j.jped.2018.04.007
Mieli-Vergani G, Vergani D, Baumann U, Czubkowski P, Debray D, Dezsofi A et al (2018) Diagnosis and management of pediatric autoimmune liver disease: ESPGHAN Hepatology Committee position statement. J Pediatr Gastroenterol Nutr 66:345–360
Pape S, Schramm C, Gevers TJG (2019) Clinical management of autoimmune hepatitis. United Eur Gastroenterol J 7(9):1156–1163
Schilsky ML (2017) Wilson disease Wilson disease copper ceruloplasmin liver failure. Clin Liver Dis 21:6520. https://doi.org/10.1016/j.cld.2017.06.011
Roberts EA, Socha P (2017) Wilson disease in children. Handbook of clinical neurology, 1st ed. vol. 142. Elsevier B.V, 141–156 p. https://doi.org/10.1016/B978-0-444-63625-6.00012-4
Socha P, Janczyk W, Dhawan A, Baumann U, D’Antiga L, Tanner S et al (2018) Wilson’s disease in children: a position paper by the Hepatology Committee of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 66(2):334–344
Hui J, Yuen YP, Chow CM, Chong J, Chiang G, Cheung CK et al (2013) Isolated persistent elevation of alanine transaminase for early diagnosis of pre-symptomatic Wilson’s disease in Chinese children. World J Pediatr 9(4):361–364
Nardecchia S, Auricchio R, Discepolo V, Troncone R (2019) Extra-intestinal manifestations of coeliac disease in children: clinical features and mechanisms. Front Pediatr 7:1–9
Joshi A, Falodia S, Kumar N, Gupta P, Khatri PC (2018) Prevalence of celiac disease among pediatric patients with cryptogenic cirrhosis and effect of gluten-free-diet. Indian J Gastroenterol 37(3):243–247
Hujoel IA, Reilly NR, Rubio-Tapia A (2019) Celiac disease: clinical features and diagnosis. Gastroenterol Clin North Am 48(1):19–37. https://doi.org/10.1016/j.gtc.2018.09.001
Anania C, De Luca E, De Castro G, Chiesa C, Pacifico L (2015) Liver involvement in pediatric celiac disease. World J Gastroenterol 21(19):5813–5822
Vo HD, Xu J, Rabinowitz SS, Fisher SE, Schwarz SM (2014) The liver in pediatric gastrointestinal disease. J Pediatr Gastroenterol Nutr 59(3):288–299
Saubermann LJ, Deneau M, Falcone RA, Murray KF, Ali S, Kohli R et al (2017) Hepatic issues and complications associated with inflammatory bowel disease: a clinical report from the naspghan inflammatory bowel disease and hepatology committees. J Pediatr Gastroenterol Nutr 64(4):639–652
Pusateri AJ, Kim SC, Dotson JL, Balint JP, Potter CJ, Boyle BM et al (2015) Incidence, pattern, and etiology of elevated liver enzymes in pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr 60(5):592–597
Leeuwen L, Fitzgerald DA, Gaskin KJ (2014) Liver disease in cystic fibrosis. Paediatr Respir Rev 15(1):69–74. https://doi.org/10.1016/j.prrv.2013.05.001
VanDevanter DR, Kahle JS, O’Sullivan AK, Sikirica S, Hodgkins PS (2016) Cystic fibrosis in young children: a review of disease manifestation, progression, and response to early treatment. J Cyst Fibros 15(2):147–157. https://doi.org/10.1016/j.jcf.2015.09.008
Leung DH, Narkewicz MR (2021) Cystic fibrosis: hepatobiliary disease. UPTODATE
Sabharwal S, Schwarzenberg SJ (2021) Cystic fibrosis: overview of gastrointestinal disease. UPTODATE
Van De Peppel IP, Bertolini A, Jonker JW, Bodewes FAJA, Verkade HJ (2017) Diagnosis, follow-up and treatment of cystic fibrosis-related liver disease. Curr Opin Pulm Med 23(6):562–569
Matsui A (2005) Hypertransaminasemia: the end of a thread. J Gastroenterol 40:859–860
Chanprasert S, Scaglia F (2015) Adult liver disorders caused by inborn errors of metabolism: review and update. Mol Genet Metabol. 114:1–10
Wright MA, Yang ML, Parsons JA, Westfall JM, Yee AS (2012) Consider muscle disease in children with elevated transaminase. J Am Board Fam Med 25(4):536–540
Pettersson J, Hindorf U, Persson P, Bengtsson T, Malmqvist U, Werkström V et al (2008) Muscular exercise can cause highly pathological liver function tests in healthy men. Br J Clin Pharmacol 65(2):253–259
Artigas M (2009) Hipertransaminasemia moderada en paciente asintomático tras realización de esfuerzo físico en gimnasio. Cart AL Dir 4–5
Jilani OK, Shrensel JA, Kanakadandi V, Ahmad J (2015) Macro-AST: a normal explanation for abnormal liver function tests. Am J Gastroenterol 110:S345
Author information
Authors and Affiliations
Contributions
Joana Meneses Costa and Sara Martins Pinto: drafting of the manuscript. Ermelinda Santos-Silva: critical revision of the manuscript. Helena Moreira-Silva: study concept and design, drafting of the manuscript, and critical revision of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Communicated by Peter de Winter.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Costa, J.M., Pinto, S.M., Santos-Silva, E. et al. Incidental hypertransaminasemia in children—a stepwise approach in primary care. Eur J Pediatr 182, 1601–1609 (2023). https://doi.org/10.1007/s00431-023-04825-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04825-4