Abstract
Aerococcus urinae (A. urinae) is primarily recognized as a common pathogen in the geriatric population, causing urinary tract infection (UTI), sepsis, and endocarditis, predominantly in female patients. In the paediatric population, only a few case reports exist suggesting A. urinae causes malodorous urine in otherwise healthy boys. In this study, we investigated the spectrum of clinical and laboratory presentations of A. urinae detection in children. A retrospective, single-centre, case series including all patients with the detection of A. urinae during a 7-year study period. Patients with detection of A. urinae only in non-urogenital skin swabs were excluded. A total of 40 samples from 33 patients were identified of which 20 patients were included in the final analysis. The median (IQR) age was 6.8 (2.9–9.5) years; 18 (90%) patients were boys. Four patients were diagnosed with a UTI, six had malodorous urine without UTI, three were diagnosed with balanitis and seven showed A. urinae colonization in the urine culture. Urogenital disorders were present in 12 patients. Additional pathogens were detected in 13 patients. Recurrence of detection during our study period was observed in four (20%) patients.
Conclusion: Beyond malodorous urine, A. urinae detection is associated with more severe presentations including UTI in the paediatric population. Pre-existing urogenital disorders were frequent, and therefore, a nephro-urological investigation should be considered in all cases of A. urinae detection in the paediatric population.
What is Known: • Aerococcus urinae (A. urinae) is known to be a common pathogen in the geriatric population, causing urinary tract infection (UTI), sepsis, and endocarditis, predominantly in female patients. • In the paediatric population, A. urinae is mainly described as a low-grade pathogen. Some case reports describe A. urinae as the cause of extraordinary malodorous urine in otherwise healthy boys. | |
What is New: • Beyond malodorous urine, A. urinae detection is associated with more severe presentations including UTI in the paediatric population. • A. urinae was mainly detected in boys with pre-existing urogenital disorders; therefore, a nephro-urological investigation should be considered in cases of A. urinae detection in the paediatric population. |
Similar content being viewed by others
Introduction
Aerococcus urinae is a Gram-positive, alpha-haemolytic and catalase-negative bacterium first described in 1953 [1]. The detection has been challenging due to morphotype similarities with streptococci and coagulase-negative staphylococci. Since the introduction of matrix-assisted laser desorption ionization time of flight mass spectrometry (MALDI-TOF MS), A. urinae is increasingly detected and reported in the literature [2].
Previously thought to be a contaminant, A. urinae is now primarily recognized as a pathogen in the geriatric population, causing urinary tract infection (UTI), sepsis, and endocarditis [3]. Predisposing factors for colonization and UTI with A. urinae are as follows: age above 65 years, female sex, underlying systemic medical conditions (e.g. diabetes mellitus, heart disease), and urogenital disorders [4].
It has been suggested, that A. urinae is a rare cause of extraordinary malodorous urine in otherwise healthy boys [5, 6]. This is in contrast to the fact that generally, parental reporting of “smelly urine” is not indicative of a UTI [7]. In the case of A. urinae, the presence of additional pathogens in urine culture is reported potentially enhancing the extraordinary odour [6]. However, monoculture has been more frequently reported in case reports when A. urinae is detected with malodorous urine [5, 8, 9]. For A. urinae infection, most case reports suggest it is a low-grade pathogen, with only a few cases of more severe presentations. These include the case of a 12-year-old boy with an acute pyelonephritis [10]. Two further cases (in an 11-year-old and a 17-year-old boy) had a subacute infective endocarditis, both with underlying congenital heart disease and an initial history of malodorous urine [11, 12].
Only little is known about the risk factors and the spectrum of clinical and laboratory presentation of A. urinae in children, particularly in those with more severe presentations.
We therefore aim to describe the spectrum of clinical and laboratory presentation of all retrospectively identified cases with the detection of A. urinae.
Methods
Study design and setting
The study is a retrospective case series including patients identified using the laboratory records of the division of clinical bacteriology at the University Hospital of Basel between January 1st, 2014, and December 31st, 2020. Inclusion criteria were the isolation of A. urinae in any sample (urine, blood or swab) of patients cared for at the University Children’s Hospital in Basel, Switzerland and with parental consent to participate in research. Exclusion criteria were the detection of A. urinae in non-urogenital skin swabs only and/or missing consent to participate. The study was approved by the ethics commission of Northwestern and Central Switzerland (EKNZ 2021–00321) and was done in accordance with the tenets of the Declaration of Helsinki and in compliance with Swiss patient data protection regulations.
Microbiology
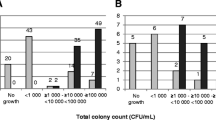
Microbiological growth was assessed by inoculating 1 µL of urine stabilized by boric acid (Sarstedt urotubes) on a 5% sheep blood agar and non-selective chromagar plate (bioMérieux, Lyon, France). We determined the bacterial species from single bacterial isolates using MALDI-TOF MS (Bruker, Bremen, Germany) using the mass-spectrum library and the MALDI Biotyper 3 software (OC 3.1. Bruker Daltonics) at standard settings. Subsequent antibiotic resistance testing was conducted according to EUCAST recommendations. According to the local resistance situation, all A. urinae strains were considered susceptible to amoxicillin. Antibiotic resistance testing was therefore only done on request.
Data sources
Electronic medical records were used to extract the following data: baseline epidemiological characteristics, clinical presentation, laboratory measurements including bacterial cultures, imaging, treatment and clinical outcome. A database was used for the storage of encoded data extracted from the electronic medical records.
Data analysis and statistical methods
Stratified analysis was performed in the following groups: UTI, malodorous urine without UTI, balanitis, and colonization. Criteria for UTI were used according to the Swiss Consensus Recommendations [13]. These include clinical signs and symptoms (fever, pollakiuria, dysuria, and loin tenderness) and significant growth of a single uropathogen (≥ 100,000 CFU/ml in midstream urine samples with pyuria and symptoms, ≥ 10,000 CFU/ml obtained through catheterization). Exception for distinct clinical symptoms was made in Neurogenic Bladder, where UTI was diagnosed with none or mild symptoms if significant growth of a single uropathogen and pyuria was present. Diagnosis of acute focal bacterial nephritis (AFBN) was based on magnetic resonance imaging. It is described, that AFBN may occur without significant growth of a uropathogen and with normal urinalysis [14]. Cases without clinical signs of UTI, normal urine analysis and a non-significant bacterial growth with a single dominating uropathogen were classified as colonization. The group “malodorous urine” was differentiated from colonization if an extremely unpleasant smell was reported with a high level of distress in the affected children. Significant pyuria was defined using the current cut-off from the laboratory of the University Hospital Basel (WBC > 20/µl, from July 1st, 2020, WBC > 56/µl after a change of flow cytometry devices). The software used for descriptive statistics was IBM SPSS Statistics (Version 24.0.0.0).
Results
Study population
During the 7-year study period, A. urinae was isolated from 40 samples in 33 patients. A total of 13 patients were excluded from further analysis for the following reasons: parents not available for consent (n = 8), consent refused (n = 2) or A. urinae detection in a non-urogenital skin swab (n = 3). Hence, we included 20 patients in the final analysis (Fig. 1). The median (IQR) age was 6.8 (2.9–9.5) years; 18 (90%) patients were boys (Table 1). A. urinae was detected in 17 urine cultures and 3 urogenital swabs but not in blood cultures. The final diagnoses were as follows: UTI (n = 4), of which two fulfilled the criteria of an AFBN; malodorous urine without UTI (n = 6), balanitis (n = 3) and colonization without UTI (n = 7). The age in the four groups was comparable; however, patients with UTI and malodorous urine tended to be older than patients with balanitis or colonization (Table 1).
Clinical findings
The most common reason for the presentation was malodorous urine (n = 5, 25%). Further reasons included the following: balanitis (n = 3), fever (n = 3), abdominal pain (n = 2), incontinence (n = 2) and acute urinary retention, recurrent UTI and testicular pain (one each). Fever at presentation and during admission/follow-up was reported in five patients, of which three were diagnosed with an A. urinae UTI and two had a fever without laboratory proof of UTI. Both patients with AFBN presented with fever and abdominal pain; one patient also complained about more specific one-sided flank pain.
Urogenital disorders
Urogenital disorders were present in 12/20 patients (60%). Nine patients had an underlying congenital anomaly of the kidney and urinary tract (CAKUT), including the following with several options possible per patient: posterior urethral valves (n = 5), epispadias (n = 2) and hypospadias (n = 2), and one each with hydronephrosis, vesicoureteral reflux (VUR), urethral diverticulum, bladder diverticulum, urethral fistula and bladder exstrophy. Further urogenital disorders included the following: bladder bowel dysfunction (n = 3), neurogenic bladder because of myelomeningocele (n = 2) and phimosis (n = 1) (Table 2). In patients with urogenital disorders, 4/12 (33.3%) had repeated A. urinae detection in urine cultures, whereas in patients without an underlying disorder, none had repeated A. urinae detection.
Microbiology
A. urinae was detected in 17/20 cases (85%) in urine cultures and in 3/20 cases (15%) in urogenital swabs. Of those patients with A. urinae detected in urine cultures, 7 were monocultures and 10 (all non-UTI) had other potential pathogens identified: including Escherichia coli, Klebsiella oxytoca, Enterococcus species, Facklamia species and Staphylococcus epidermidis in urine. In urogenital skin swabs, none was a monoculture for A. urinae and further potential pathogens were identified including Streptococcus anginosus, Enterococcus faecalis, Proteus vulgaris, Morganella morganii and Corynebacterium aurimucosum. The resistance pattern was available in one patient only as this is not routinely performed and only tested on request.
Laboratory findings and imaging
Overall, pyuria was found in nine patients (45%) (Table 2). C-reactive protein (CRP) was measured in six patients and elevated (> 5 mg/L) in five. Kidney function was measured in five patients and reported as normal in all. Both patients with AFBN had an elevated CRP, nephritic foci in magnetic resonance imaging (MRI) and no other pathogen detection.
Treatment
Overall, 14/20 patients (70%) were treated with antibiotics, including all patients with UTI or malodorous urine. Oral amoxicillin, amoxicillin/clavulanic acid or cefpodoxime or intravenous third-generation cephalosporins (ceftriaxone or ceftazidime) were used for treatment. Patients with AFBN were treated with third-generation cephalosporins for 3 weeks. Patients with malodorous urine were all treated with oral amoxicillin or amoxicillin/clavulanic acid for 5–7 days. Five patients required hospital admission, due to decreased general condition and/or the need for intravenous antibiotic treatment.
Outcome
All patients with UTI were successfully treated with a clinical cure. However, the recurrence of A. urinae detection occurred in two patients, one after 2 months and one after 2 years. In patients with malodorous urine, the disappearance of the extraordinary unpleasant smell was achieved in all patients. One patient had recurrent episodes with malodourous urine and A. urinae detection until the surgical treatment of urethral valves.
Discussion
Our study indicates that A. urinae in children is predominantly detected in boys. Malodorous urine and UTI with A. urinae were only seen in boys. Interestingly, this finding contrasts reports in adults, in whom A. urinae bacteriuria is found more often in females or at similar frequencies in both sexes [4, 15,16,17]. Invasive infections with A. urinae bacteraemia, however, are typically found in elderly men with urogenital disorders [18]. The reason for this variable sex distribution between the different age groups remains unclear.
In our study population, urogenital disorders were present in two-thirds of the patients, including all patients with a urinary tract infection. Patients with urogenital disorders were also more likely to have recurrent A. urinae infections. Our findings correlate with the literature in adults, which describes an association of urogenital disorders with A. urinae bacteriuria or infections [4, 18]. Urogenital disorders were also described in some of the case reports on A. urinae infections in children. A bladder diverticulum was found in a 5-year-old boy with malodorous urine [8], and prior pyeloplasty and VUR were described in a 12-year-old boy with an A. urinae UTI [10]. The association of urogenital disorders and recurrent detection also correlates with data from a mouse model that showed susceptibility to prolonged bacteriuria with A. urinae in mice with inherent vesicoureteral reflux [19]. Our findings together with the existing literature suggest that A. urinae bacteriuria may indicate an underlying urogenital disorder.
Mixed infections were documented in this case series, suggesting that A. urinae is part of the urogenital flora. Also, mixed cultures including A. urinae have been described to lead to malodorous urine [6]; however, this seems not always to be the case, as shown in one of our patients who had a malodorous urine without a mixed culture. It is well known, that pathogens produce different bacteria-specific volatile organic compounds that can cause a characteristic smell [20]. Physicians in our study described the malodorous urine as a foul or with a fishy smell. This smell has been attributed trimethylaminuria which can be produced by bacteria species such as Pseudomonas and E. coli [21] and likely also by A. urinae.
Our study is the first to show more severe presentations associated with the detection of A. urinae in several children. So far, only one previous case was described with an A. urinae infection causing a UTI in a 12-year-old boy [10]. In our study, we detected four cases of UTI with A. urinae, all of which occurred in boys and were associated with urogenital disorders. Two of these cases were diagnosed with AFBN. Whether A. urinae was the cause of the infection in these two children is debatable. There is an association between urogenital disorders and AFBN, which might lead to A. urinae being present as a bystander bacterium and not as an infective cause [14]. However, the detection of A. urinae monocultures in both cases with AFBN suggests there is a causal relationship. Bacteraemia and systemic infection with A. urinae were described in the literature including two case reports with endocarditis in the paediatric population [11, 12]. These findings suggest that invasive infections with A. urinae like AFBN are conceivable.
This study was limited by the number of patients and by its retrospective design. Unfortunately, informed consent could not be obtained for ten children, and therefore, these cases were not included. Despite its clinical significance in selected cases, A. urinae remains an unusual pathogen in the paediatric age group. Nevertheless, to the best of our knowledge, this is the largest case series describing the spectrum of A. urinae infection in the paediatric population. Our findings are likely transferable to other similar settings given its long observation period and should raise awareness for this unusual pathogen in the paediatric age group. We suggest further investigations of A. urinae in the context of urinary tract infections with a multi-centre study to provide further evidence. In addition, a prospective study would allow a standardized protocol to collect clinical and laboratory data and give more information about the long-term follow-up.
In conclusion, our findings show that A. urinae is not only causing malodorous urine but may lead to a more severe presentation. Our study suggests that in paediatric populations, A. urinae predominantly affects boys. As most cases were associated with urogenital disorders, a nephro-urological investigation should be considered when A. urinae is detected.
Data availability
Upon request relevant documentation and data can be presented for data transparency.
Abbreviations
- AFBN:
-
Acute focal bacterial nephritis
- AMC:
-
Amoxicillin-clavulanic acid
- AMX:
-
Amoxicillin
- A. urinae :
-
Aerococcus urinae
- BBD:
-
Bladder bowel dysfunction
- CAKUT:
-
Congenital anomaly of the kidney and urinary tract
- CRP:
-
C-reactive protein
- IQR:
-
Interquartile range
- MALDI-TOF MS:
-
Matrix-assisted laser desorption ionization time of flight mass spectrometry
- MRI:
-
Magnetic resonance imaging
- Ns:
-
Not specified
- PUV:
-
Posterior urethral valves
- UTI:
-
Urinary tract infection
- VUR:
-
Vesicoureteral reflux
- WBC:
-
White blood cell
References
Williams RE, Hirch A, Cowan ST (1953) Aerococcus, a new bacterial genus. J Gen Microbiol 8:475–480. https://doi.org/10.1099/00221287-8-3-475
Opota O, Prod’hom G, Andreutti-Zaugg C, Dessauges M, Merz L, Greub G, Chave JP, Jaton K (2016) Diagnosis of Aerococcus urinae infections: importance of matrix-assisted laser desorption ionization time-of-flight mass spectrometry and broad-range 16S rDNA PCR. Clin Microbiol Infect 22:e1–e2. https://doi.org/10.1016/j.cmi.2015.08.026
Rasmussen M (2016) Aerococcus: an increasingly acknowledged human pathogen. Clin Microbiol Infect 22:22–27. https://doi.org/10.1016/j.cmi.2015.09.026
Sierra-Hoffman M, Watkins K, Jinadatha C, Fader R, Carpenter JL (2005) Clinical significance of Aerococcus urinae: a retrospective review. Diagn Microbiol Infect Dis 53:289–292. https://doi.org/10.1016/j.diagmicrobio.2005.06.021
de Vries TW, Brandenburg AH (2012) Foul smelling urine in a 7-year-old boy caused by Aerococcus urinae. Pediatr Infect Dis J 31:1316–1317. https://doi.org/10.1097/INF.0b013e318268d25e
Lenherr N, Berndt A, Ritz N, Rudin C (2014) Aerococcus urinae: a possible reason for malodorous urine in otherwise healthy children. Eur J Pediatr 173:1115–1117. https://doi.org/10.1007/s00431-014-2348-9
Struthers S, Scanlon J, Parker K, Goddard J, Hallett R (2003) Parental reporting of smelly urine and urinary tract infection. Arch Dis Child 88:250–252. https://doi.org/10.1136/adc.88.3.250
Skalidis T, Papaparaskevas J, Konstantinou D, Kapolou E, Falagas ME, Legakis N (2017) Aerococcus urinae, a cause of cystitis with malodorous urine in a child: clinical and microbiological challenges. JMM Case Rep 4:e005083. https://doi.org/10.1099/jmmcr.0.005083
Gibb AP, Sivaraman B (2013) A second case of foul smelling urine in a boy caused by Aerococcus urinae. Pediatr Infect Dis J 32:1300–1301. https://doi.org/10.1097/INF.0b013e3182a64054
Murray TS, Muldrew KL, Finkelstein R, Hampton L, Edberg SC, Cappello M (2008) Acute pyelonephritis caused by Aerococcus urinae in a 12-year-old boy. Pediatr Infect Dis J 27:760–762. https://doi.org/10.1097/INF.0b013e318170af46
Sous N, Piwoz JA, Baer AZ, Bhavsar SM (2019) Subacute Aerococcus urinae infective endocarditis with mycotic aneurysms in a pediatric patient: case report and literature review. J Pediatric Infect Dis Soc 8:492–494. https://doi.org/10.1093/jpids/piz016
Qureshi NK, Patel E (2018) Aerococcus urinae as the causative agent in infective endocarditis of the aortic valve in a pediatric patient. Pediatr Infect Dis J 37:1065–1066. https://doi.org/10.1097/INF.0000000000001944
Buettcher M, Trueck J, Niederer-Loher A, Heininger U, Agyeman P, Asner S, Berger C, Bielicki J, Kahlert C, Kottanattu L, Meyer Sauteur PM, Paioni P, Posfay-Barbe K, Relly C, Ritz N, Zimmermann P, Zucol F, Gobet R, Shavit S, Rudin C, Laube G, von Vigier R, Neuhaus TJ (2021) Swiss consensus recommendations on urinary tract infections in children. Eur J Pediatr 180:663–674. https://doi.org/10.1007/s00431-020-03714-4
Bitsori M, Raissaki M, Maraki S, Galanakis E (2015) Acute focal bacterial nephritis, pyonephrosis and renal abscess in children. Pediatr Nephrol 30:1987–1993. https://doi.org/10.1007/s00467-015-3141-3
Cattoir V, Kobal A, Legrand P (2010) Aerococcus urinae and Aerococcus sanguinicola, two frequently misidentified uropathogens. Scand J Infect Dis 42:775–780. https://doi.org/10.3109/00365548.2010.485576
Senneby E, Petersson AC, Rasmussen M (2015) Epidemiology and antibiotic susceptibility of aerococci in urinary cultures. Diagn Microbiol Infect Dis 81:149–151. https://doi.org/10.1016/j.diagmicrobio.2014.11.009
Shelton-Dodge K, Vetter EA, Kohner PC, Nyre LM, Patel R (2011) Clinical significance and antimicrobial susceptibilities of Aerococcus sanguinicola and Aerococcus urinae. Diagn Microbiol Infect Dis 70:448–451. https://doi.org/10.1016/j.diagmicrobio.2010.09.001
Senneby E, Petersson AC, Rasmussen M (2012) Clinical and microbiological features of bacteraemia with Aerococcus urinae. Clin Microbiol Infect 18:546–550. https://doi.org/10.1111/j.1469-0691.2011.03609.x
Gilbert NM, Choi B, Du J, Collins C, Lewis AL, Putonti C, Wolfe AJ (2021) A mouse model displays host and bacterial strain differences in Aerococcus urinae urinary tract infection. Biol Open. https://doi.org/10.1242/bio.058931
Thorn RM, Reynolds DM, Greenman J (2011) Multivariate analysis of bacterial volatile compound profiles for discrimination between selected species and strains in vitro. J Microbiol Methods 84:258–264. https://doi.org/10.1016/j.mimet.2010.12.001
Bos LD, Sterk PJ, Schultz MJ (2013) Volatile metabolites of pathogens: a systematic review. PLoS Pathog 9:e1003311. https://doi.org/10.1371/journal.ppat.1003311
Funding
Open access funding provided by University of Basel
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Data collection was performed by Adrian Egli and Dimitri Rast. Data analysis was performed by Nicole Ritz and Dimitri Rast. The first draft of the manuscript was written by Dimitri Rast, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the ethics commission of Northwestern and Central Switzerland (EKNZ 2021–00321) and was done in accordance with the tenets of the Declaration of Helsinki and in compliance with Swiss patient data protection regulations.
Consent to participate
Informed consent was obtained from all caregivers of participants in the study.
Consent for publication
Not applicable. No individual images or videos are shown.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Tobias Tenenbaum
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rast, D., Evers, K.S., Egli, A. et al. Aerococcus urinae — significance of detection in the paediatric urinary tract: a case series. Eur J Pediatr 182, 749–756 (2023). https://doi.org/10.1007/s00431-022-04730-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04730-2