Abstract
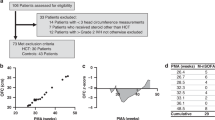
Hydrocortisone is used in preterm infants. However, early disruption of growth velocities was observed in infants exposed to hydrocortisone. This retrospective study aimed to explore the postnatal brain growth of extremely preterm infants requiring hydrocortisone treatment as well as its association with perinatal factors. Extremely preterm infants exposed to hydrocortisone from 2011 to 2016 who survived up to 12 months were included. Each of them was matched with two infants not treated with hydrocortisone exhibiting similar gestational ages and nearly similar birth head circumferences. The outcome variables were brain tissue areas on MRIs performed at term-equivalent age and postnatal head circumference growth up to a corrected age of 12 months. Univariate and multiple regression analyses were performed. Infants treated with hydrocortisone (n=20) were matched with 40 infants not exposed to hydrocortisone. The infants exposed to hydrocortisone exhibited a lower birth weight (p=0.04) and a longer duration of mechanical ventilation (p<0.0001). Infants treated with hydrocortisone exhibited a smaller basal ganglia/thalamus area (p=0.04) at term-equivalent age and a smaller head circumference at a corrected age of 12 months (p=0.003). However, the basal ganglia/thalamus area and the postnatal brain growth were independently associated with the duration of mechanical ventilation and not with hydrocortisone. Interestingly, a significant interaction between hydrocortisone and sex was observed (p=0.04).
Conclusion: This study supports previous data that indicated no obvious impact of hydrocortisone on brain growth and highlights the relationship between the severity of the neonatal course and postnatal brain growth in extremely preterm infants.
What is Known: • Postnatal hydrocortisone disrupts transiently growth velocities including the head circumference growth. • Postnatal hydrocortisone has less impact on neurodevelopment than dexamethasone. | |
What is New: • Hydrocortisone prescribed for infants in the most severe conditions did not show independent effect on brain growth up to the corrected age of 12 months. However, a different effect of hydrocortisone according to sex can't be excluded and needs further explorations. • Perinatal factors as birth weight and duration of mechanical ventilation were determinant for the subsequent brain growth. |

Similar content being viewed by others
Data availability
N/A
Code availability
N/A
Abbreviations
- BGT:
-
Basal ganglia and thalamus
- BPD:
-
Bronchopulmonary dysplasia
- FiO2 :
-
Fraction of inspired oxygen
- HC:
-
Head circumference
- MRI:
-
Magnetic resonance imaging
- TEA:
-
Term-equivalent age
References
Gui L, Loukas S, Lazeyras F, Hüppi PS, Meskaldji DE, Borradori Tolsa C (2019) Longitudinal study of neonatal brain tissue volumes in preterm infants and their ability to predict neurodevelopmental outcome. NeuroImage 185:728–741. https://doi.org/10.1016/j.neuroimage.2018.06.034
Keunen K, Išgum I, van Kooij BJM, Anbeek P, van Haastert IC, Koopman-Esseboom C, Fieret-van Stam PC, Nievelstein RAJ, Viergever MA, de Vries LS, Groenendaal F, Benders MJNL (2016) Brain volumes at term-equivalent age in preterm infants: imaging biomarkers for neurodevelopmental outcome through early school age. J Pediatr 172:88–95. https://doi.org/10.1016/j.jpeds.2015.12.023
Anderson PJ, Treyvaud K, Neil JJ, Cheong JLY, Hunt RW, Thompson DK, Lee KJ, Doyle LW, Inder TE (2017) Associations of newborn brain magnetic resonance imaging with long-term neurodevelopmental impairments in very preterm children. J Pediatr 187:58-65.e1. 187:58–65.e1. https://doi.org/10.1016/j.jpeds.2017.04.059
Scharf RJ, Stroustrup A, Conaway MR, DeBoer MD (2016) Growth and development in children born very low birthweight. Arch Dis Child Fetal Neonatal Ed 101:F433–F438. https://doi.org/10.1136/archdischild-2015-309427
Hack M, Breslau N, Weissman B, Aram D, Klein N, Borawski E (1991) Effect of very low birth weight and subnormal head size on cognitive abilities at school age. N Engl J Med 325:231–237. https://doi.org/10.1056/NEJM199107253250403
Franz AR, Pohlandt F, Bode H, Mihatsch WA, Sander S, Kron M, Steinmacher J (2009) Intrauterine, early neonatal, and postdischarge growth and neurodevelopmental outcome at 5.4 years in extremely preterm infants after intensive neonatal nutritional support. Pediatrics 123:e101–e109. https://doi.org/10.1542/peds.2008-1352
Ghods E, Kreissl A, Brandstetter S, Fuiko R, Widhalm K (2011) Head circumference catch-up growth among preterm very low birth weight infants: effect on neurodevelopmental outcome. J Perinat Med 39:579–586. https://doi.org/10.1515/jpm.2011.049
Doyle LW, Ehrenkranz RA, Halliday HL (2010) Dexamethasone treatment after the first week of life for bronchopulmonary dysplasia in preterm infants: a systematic review. Neonatology 98:289–296. https://doi.org/10.1159/000286212
Onland W, Cools F, Kroon A, Rademaker K, Merkus MP, Dijk PH, van Straaten HL, te Pas AB, Mohns T, Bruneel E, van Heijst AF, Kramer BW, Debeer A, Zonnenberg I, Marechal Y, Blom H, Plaskie K, Offringa M, van Kaam AH, for the STOP-BPD Study Group (2019) Effect of hydrocortisone therapy initiated 7 to 14 days after birth on mortality or bronchopulmonary dysplasia among very preterm infants receiving mechanical ventilation: a randomized clinical trial. JAMA 321:354–363. https://doi.org/10.1001/jama.2018.21443
Morris IP, Goel N, Chakraborty M (2019) Efficacy and safety of systemic hydrocortisone for the prevention of bronchopulmonary dysplasia in preterm infants: a systematic review and meta-analysis. Eur J Pediatr 178:1171–1184. https://doi.org/10.1007/s00431-019-03398-5
Benders MJNL, Groenendaal F, van Bel F, Ha Vinh R, Dubois J, Lazeyras F, Warfield SK, Hüuppi PS, de Vries LS (2009) Brain development of the preterm neonate after neonatal hydrocortisone treatment for chronic lung disease. Pediatr Res 66:555–559. https://doi.org/10.1203/PDR.0b013e3181b3aec5
Kersbergen KJ, de Vries LS, van Kooij BJM, Išgum I, Rademaker KJ, van Bel F, Hüppi PS, Dubois J, Groenendaal F, Benders MJNL (2013) Hydrocortisone treatment for bronchopulmonary dysplasia and brain volumes in preterm infants. J Pediatr 163:666–671.e1. https://doi.org/10.1016/j.jpeds.2013.04.001
Rademaker K, Uiterwaal C, Groenendaal F, et al (2007) Neonatal hydrocortisone treatment: neurodevelopmental outcome and MRI at school age in preterm-born children. In: J. Pediatr. https://pubmed.ncbi.nlm.nih.gov/17382109/. Accessed 25 Jul 2020
Parikh NA, Kennedy KA, Lasky RE, McDavid GE, Tyson JE (2013) Pilot randomized trial of hydrocortisone in ventilator-dependent extremely preterm infants: effects on regional brain volumes. J Pediatr 162:685–690.e1. https://doi.org/10.1016/j.jpeds.2012.09.054
Parikh NA, Kennedy KA, Lasky RE, Tyson JE (2015) Neurodevelopmental outcomes of extremely preterm infants randomized to stress dose hydrocortisone. PLoS One 10:e0137051. https://doi.org/10.1371/journal.pone.0137051
Patra K, Greene MM, Silvestri JM (2015) Neurodevelopmental impact of hydrocortisone exposure in extremely low birth weight infants: outcomes at 1 and 2 years. J Perinatol 35:77–81. https://doi.org/10.1038/jp.2014.133
Peltoniemi OM, Lano A, Yliherva A, Kari MA, Hallman M, for The Neonatal Hydrocortisone Working Group (2016) Randomised trial of early neonatal hydrocortisone demonstrates potential undesired effects on neurodevelopment at preschool age. Acta Paediatr 105:159–164. https://doi.org/10.1111/apa.13074
Karemaker R, Heijnen CJ, Veen S, Baerts W, Samsom J, Visser GHA, Kavelaars A, van Doornen LJP, van Bel F (2006) Differences in behavioral outcome and motor development at school age after neonatal treatment for chronic lung disease with dexamethasone versus hydrocortisone. Pediatr Res 60:745–750. https://doi.org/10.1203/01.pdr.0000246200.76860.de
Tijsseling D, ter Wolbeek M, Derks JB, de Vries WB, Heijnen CJ, van Bel F, Mulder EJH (2018) Neonatal corticosteroid therapy affects growth patterns in early infancy. PLoS One 13:e0192162. https://doi.org/10.1371/journal.pone.0192162
Xu Y, Morel B, Dahdouh S, et al (2018) The challenge of cerebral magnetic resonance imaging in neonates: a new method using mathematical morphology for the segmentation of structures including diffuse excessive high signal intensities. In: Med. Image Anal. https://pubmed.ncbi.nlm.nih.gov/29852312/?from_single_result=Morel+B+AND+Dahdouh+S+AND+2018. Accessed 25 Jul 2020
Fenton T, Kim J (2013) A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. In: BMC Pediatr. https://pubmed.ncbi.nlm.nih.gov/23601190/?from_term=Fenton+TR+2003&from_pos=1. Accessed 14 Mar 2020
WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. https://www.who.int/publications-detail-redirect/924154693X. Accessed 1 Jan 2021
Jobe AH, Bancalari E (2001) Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163:1723–1729. https://doi.org/10.1164/ajrccm.163.7.2011060
Papile L-A, Burstein J, Burstein R, Koffler H (1978) Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 92:529–534. https://doi.org/10.1016/S0022-3476(78)80282-0
Morel B, Bertault P, Favrais G, Tavernier E, Tosello B, Bednarek N, Barantin L, Chadie A, Proisy M, Xu Y, Bloch I, Sirinelli D, Adamsbaum C, Tauber C, Saliba E, EPIRMEX study group (2021) Automated brain MRI metrics in the EPIRMEX cohort of preterm newborns: correlation with the neurodevelopmental outcome at 2 years. Diagn Interv Imaging 102:225–232. https://doi.org/10.1016/j.diii.2020.10.009
Guillot M, Guo T, Ufkes S, Schneider J, Synnes A, Chau V, Grunau RE, Miller SP (2020) Mechanical ventilation duration, brainstem development, and neurodevelopment in children born preterm: a prospective cohort study. J Pediatr S0022347620306533:87–95.e3. https://doi.org/10.1016/j.jpeds.2020.05.039
Brouwer MJ, Kersbergen KJ, van Kooij BJM, Benders MJNL, van Haastert IC, Koopman-Esseboom C, Neil JJ, de Vries LS, Kidokoro H, Inder TE, Groenendaal F (2017) Preterm brain injury on term-equivalent age MRI in relation to perinatal factors and neurodevelopmental outcome at two years. PLoS One 12:e0177128. https://doi.org/10.1371/journal.pone.0177128
Lee J-M, Choi Y-H, Hong J, Kim NY, Kim E, Lim JS, Kim JD, Park HK, Lee HJ (2019) Bronchopulmonary dysplasia is associated with altered brain volumes and white matter microstructure in preterm infants. Neonatology 116:163–170. https://doi.org/10.1159/000499487
Baud O, Maury L, Lebail F, Ramful D, el Moussawi F, Nicaise C, Zupan-Simunek V, Coursol A, Beuchée A, Bolot P, Andrini P, Mohamed D, Alberti C (2016) Effect of early low-dose hydrocortisone on survival without bronchopulmonary dysplasia in extremely preterm infants (PREMILOC): a double-blind, placebo-controlled, multicentre, randomised trial. Lancet 387:1827–1836. https://doi.org/10.1016/S0140-6736(16)00202-6
Alison M, Tilea B, Toumazi A, Biran V, Mohamed D, Alberti C, Bourmaud A, Baud O, PREMILOC Trial group (2020) Prophylactic hydrocortisone in extremely preterm infants and brain MRI abnormality. Arch Dis Child Fetal Neonatal Ed 105:520–525. https://doi.org/10.1136/archdischild-2019-317720
Baud O, Trousson C, Biran V, Leroy E, Mohamed D, Alberti C, PREMILOC Trial group (2019) Two-year neurodevelopmental outcomes of extremely preterm infants treated with early hydrocortisone: treatment effect according to gestational age at birth. Arch Dis Child Fetal Neonatal Ed 104:F30–F35. https://doi.org/10.1136/archdischild-2017-313756
Bruno C, Bengani S, Gomes W, et al (2017) MRI differences associated with intrauterine growth restriction in preterm infants. In: Neonatology. https://pubmed.ncbi.nlm.nih.gov/28076856/?from_single_result=Bruno+CJ+2017+AND+intrauterine+growth+restriction. Accessed 25 Jul 2020
Parikh NA, Lasky RE, Kennedy KA, McDavid G, Tyson JE (2013) Perinatal factors and regional brain volume abnormalities at term in a cohort of extremely low birth weight infants. PLoS One 8:e62804. https://doi.org/10.1371/journal.pone.0062804
Hintz S, Kendrick D, Vohr B, Kenneth Poole W, Higgins R, THE NICHD NEONATAL RESEARCH NETWORK F (2006) Gender differences in neurodevelopmental outcomes among extremely preterm, extremely-low-birthweight infants. Acta Paediatr 95:1239–1248. https://doi.org/10.1080/08035250600599727
He L, Parikh NA (2013) Automated detection of white matter signal abnormality using T2 relaxometry: application to brain segmentation on term MRI in very preterm infants. NeuroImage 64:328–340. https://doi.org/10.1016/j.neuroimage.2012.08.081
Hammerl M, Zagler M, Zimmermann M, Griesmaier E, Janjic T, Gizewski ER, Kiechl-Kohlendorfer U, Neubauer V (2020) Supratentorial brain metrics predict neurodevelopmental outcome in very preterm infants without brain injury at age 2 years. Neonatology 117:287–293. https://doi.org/10.1159/000506836
Author information
Authors and Affiliations
Contributions
CR and MG collected the data and performed the data analysis. ES contributed to the critical reading of the manuscript. BM performed the MRI segmentation and analysis and helped write and critically read the manuscript. GF designed the study protocol, obtained ethics approval, performed the final data analysis, and wrote the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The local ethics committee (2017-031) and local data protection authority (2017-07) approved the protocol for this study.
Consent to participate and for publication
Oral and written information was provided to parents or authorized guardians. They could refuse the exploitation of their child’s data by expressing their opposition.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rousseau, C., Guichard, M., Saliba, E. et al. Duration of mechanical ventilation is more critical for brain growth than postnatal hydrocortisone in extremely preterm infants. Eur J Pediatr 180, 3307–3315 (2021). https://doi.org/10.1007/s00431-021-04113-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04113-z