Abstract
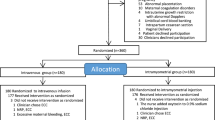
Necrotizing enterocolitis (NEC) treatment remains unchanged for years. Data suggest that mild controlled hypothermia could potentially improve NEC outcomes. Our units presented unfavourable outcomes on NEC. The aim was to assess our experience with low technology, mild controlled hypothermia on NEC outcomes, and improve preterm infants’ healthcare. This was a single-center quality improvement study with retrospective cohort design at the neonatal intensive care unit in the university hospital. Forty-three preterm infants with NEC (Modified Bell’s Stage II/III) were included: 19 in the control group (2015–2018) and 24 in the hypothermia group (2018–2020). The control group received standard treatment (fasting, abdominal decompression, and broad-spectrum antibiotics). The hypothermia group underwent cooling to 35.5 °C for 48 h after NEC diagnosis, along with conventional treatment. The primary outcomes are intestinal perforation, need for surgery, duration of parenteral nutrition, death, and extensive resection of the small intestine. There was no statistical difference in the NEC score. The hypothermia group required less surgery (aRR 0.40; 95% CI 0.19–0.85), presented less bowel perforation (aRR 0.39; 95% CI 0.18; 0.83), had a shorter duration of parenteral nutrition (aHR 5.28; 95% CI 1.88–14.89), did not need extensive intestinal resection, (0 vs 15.7%), and did not experience any deaths (0 vs 31.6%).
Conclusions: In our experience, low technology, mild controlled hypothermia was feasible, not related to adverse effects, and effective treatment for NEC Modified Bell’s Stage II/III. It avoided surgery, bowel perforation, and extensive intestinal resection; reduced mortality; and shortened parenteral nutrition duration.
What is Known: • New approaches have been proposed to avoid enterocolitis incidence; however, the treatment of enterocolitis stage 2 has been the same for decades, and unfavourable outcomes remain despite conventional management. • Studies suggest that hypothermia can be an alternative to enterocolitis treatment. | |
What is New: • Mild controlled hypothermia can be an additional practice to treat enterocolitis stage 2, is feasible, and is not related to adverse effects to preterm infants. • It can decrease surgery needs, duration of parenteral nutrition, and death and avoids extensive intestinal resection in preterm infants. |


Similar content being viewed by others
Data availability
all the data are available for inquiry or analysis.
Code availability
N/A
Abbreviations
- CPAP:
-
Continuous positive airway pressure
- NEC:
-
Necrotizing enterocolitis
- NICU:
-
Neonatal intensive care unit
- nSOFA:
-
Sequential organ failure assessment
- VLBW:
-
very low birth weight
References
Neu J, Walker WA (2011) Necrotizing enterocolitis. N Engl J Med 364(3):255–264. https://doi.org/10.1056/NEJMra1005408
Warner BB, Deych E, Zhou Y, Hall-Moore C, Weinstock GM, Sodergren E, Shaikh N, Hoffmann JA, Linneman LA, Hamvas A, Khanna G, Rouggly-Nickless LC, Ndao IM, Shands BA, Escobedo M, Sullivan JE, Radmacher PG, Shannon WD, Tarr PI (2016) Gut bacteria dysbiosis and necrotising enterocolitis in very low birthweight infants: a prospective case-control study. Lancet. 387(10031):1928–1936. https://doi.org/10.1016/S0140-6736(16)00081-7
Ganapathy V, Hay JW, Kim JH (2012) Costs of necrotizing enterocolitis and cost-effectiveness of exclusively human milk-based products in feeding extremely premature infants. Breastfeed Med 7(1):29–37. https://doi.org/10.1089/bfm.2011.0002
Sankaran K, Puckett B, Lee DSC, Seshia M, Boulton J, Qiu Z, Lee SK, Canadian Neonatal Network (2004) Variations in incidence of necrotizing enterocolitis in Canadian neonatal intensive care units. J Pediatr Gastroenterol Nutr 39(4):366–372. https://doi.org/10.1097/00005176-200410000-00012
Rees CM, Eaton S, Pierro A (2010) National prospective surveillance study of necrotizing enterocolitis in neonatal intensive care units. J Pediatr Surg 45(7):1391–1397. https://doi.org/10.1016/j.jpedsurg.2009.12.002
Yee WH, Soraisham AS, Shah VS, Aziz K, Yoon W, Lee SK, the Canadian Neonatal Network (2012) Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics. 129(2):e298–e304. https://doi.org/10.1542/peds.2011-2022
Zozaya C, García González I, Avila-Alvarez A, et al. Incidence, treatment, and outcome trends of necrotizing enterocolitis in preterm infants: A multicenter cohort study. Front Pediatr. 2020;8(188). https://doi.org/10.3389/fped.2020.00188
Guner YS, Friedlich P, Wee CP, Dorey F, Camerini V, Upperman JS (2009) State-based analysis of necrotizing enterocolitis outcomes. J Surg Res 157(1):21–29. https://doi.org/10.1016/j.jss.2008.11.008
Rees CM, Pierro A, Eaton S (2007) Neurodevelopmental outcomes of neonates with medically and surgically treated necrotizing enterocolitis. Arch Dis Child Fetal Neonatal Ed 92(3):F193–F198. https://doi.org/10.1136/adc.2006.099929
Adams M, Bassler D, Darlow BA, Lui K, Reichman B, Hakansson S, Norman M, Lee SK, Helenius KK, Lehtonen L, San Feliciano L, Vento M, Moroni M, Beltempo M, Yang J, Shah PS, International Network for EvaluatingOutcomes (iNeo) of Neonates (2019) Preventive strategies and factors associated with surgically treated necrotising enterocolitis in extremely preterm infants: an international unit survey linked with retrospective cohort data analysis. BMJ Open 9(10):e031086. https://doi.org/10.1136/bmjopen-2019-031086
Talavera MM, Bixler G, Cozzi C, Dail J, Miller RR, McClead R, Reber K (2016) Quality improvement initiative to reduce the necrotizing enterocolitis rate in premature infants. Pediatrics. 137(5):e20151119. https://doi.org/10.1542/peds.2015-1119
Rolnitsky A, Ng E, Asztalos E, Shama Y, Karol D, Findlater C, Garsch M, Dunn M (2019) A quality improvement intervention to reduce necrotizing Enterocolitis in premature infants with probiotic supplementation. Pediatr Qual Saf 4(5):e201. https://doi.org/10.1097/pq9.0000000000000201
Gephart SM, Hanson C, Wetzel CM, Fleiner M, Umberger E, Martin L, Rao S, Agrawal A, Marin T, Kirmani K, Quinn M, Quinn J, Dudding KM, Clay T, Sauberan J, Eskenazi Y, Porter C, Msowoya AL, Wyles C, Avenado-Ruiz M, Vo S, Reber KM, Duchon J (2017) NEC-zero recommendations from scoping review of evidence to prevent and foster timely recognition of necrotizing enterocolitis. Matern Heal Neonatol Perinatol 3(1):1–14. https://doi.org/10.1186/s40748-017-0062-0
Hall NJ, Eaton S, Peters MJ, et al. Mild controlled hypothermia in preterm neonates with advanced necrotizing enterocolitis. Pediatrics. 2010;125(2). https://doi.org/10.1542/peds.2008-3211
Garrett-Cox RG, Pierro A, Spitz L, Eaton S (2003) Body temperature and heat production in suckling rat endotoxaemia: beneficial effects of glutamine. J Pediatr Surg 38:37–44. https://doi.org/10.1053/jpsu.2003.50006
Vinardi BS, Pierro A, Parkinson EJ et al (2003) Attenuates lung neutrophil infiltration. J Pediatr Surg 38:88–91. https://doi.org/10.1053/jpsu.2003.50017
Kimura Y, Pierro A, Eaton S (2009) Glutathione synthesis in intestinal ischaemia-reperfusion injury: effects of moderate hypothermia. J Pediatr Surg 44:353–357. https://doi.org/10.1016/j.jpedsurg.2008.10.091
Stefanutti G, Pierro A, Vinardi S, Spitz L, Eaton S (2005) Moderate hypothermia protects against systemic oxidative stress in a rat model of intestinal ischemia and reperfusion injury. Shock. 24(2):159–164. https://doi.org/10.1097/01.shk.0000168871.60531.6f
Stefanutti G, Pierro A, Parkinson EJ, Smith VV, Eaton S (2008) Moderate hypothermia as a rescue therapy against intestinal ischemia and reperfusion injury in the rat. Crit Care Med 36(5):1564–1572. https://doi.org/10.1097/CCM.0b013e3181709e9f
Couto LDCA; Souza TR; Ferreira CHF; Calixto C; Carnevale-Silva A; Aragon DC; Maiolini BL; Silva ACB; Souza GA; Martins-Filho PF; Toffolo RO; Fukamichi SL; Gonçalves-Ferri W. Unfavorable evolution of enterocolitis: the mystery continues.In: 3rd Congress of Joint European Neonatal Societies (jENS) 2019, Maastrich, The Netherlands
Bell MJ, Ternberg JL, Feigin RD et al (1978) Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 187(1):1–7. https://doi.org/10.1097/00000658-197801000-00001
Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D (2015 Nov) SQUIRE 2.0 (standards for QUality improvement reporting excellence): revised publication guidelines from a detailed consensus process. J Contin Educ Nurs 46(11):501–507. https://doi.org/10.3928/00220124-20151020-02
Volpe JJ. Neurology of the Newborn. (Saunders, ed.). Philadelphia; 1995. https://doi.org/10.1002/mus.880180822
Singh Y, Tissot C, Fraga M et al (2020) International evidence-based guidelines on point of care ultrasound (POCUS) for critically ill neonates and children issued by the POCUS working Group of the European Society of Paediatric and neonatal intensive care (ESPNIC). Crit Care 24(1):65. https://doi.org/10.1186/s13054-020-2787-9
Wynn JL, Polin RA (2019) A neonatal sequential organ failure assessment score predicts mortality to late-onset sepsis in preterm very low birth weight infants. Pediatr Res 88(1):85–90. https://doi.org/10.1038/s41390-019-0517-2
Gephart SM, Spitzer AR, Effken JA, Dodd E, Halpern M, McGrath JM (2014) Discrimination of GutCheck NEC: a clinical risk index for necrotizing enterocolitis. J Perinatol 34(6):468–475. https://doi.org/10.1038/jp.2014.37
Villar J, Papageorghiou AT, Pang R, Ohuma EO, Cheikh Ismail L, Barros FC, Lambert A, Carvalho M, Jaffer YA, Bertino E, Gravett MG, Altman DG, Purwar M, Frederick IO, Noble JA, Victora CG, Bhutta ZA, Kennedy SH, International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st) (2014) The likeness of fetal growth and newborn size across non-isolated populations in the INTERGROWTH-21st project: the fetal growth longitudinal study and newborn cross-sectional study. Lancet Diabetes Endocrinol 2(10):781–792. https://doi.org/10.1016/S2213-8587(14)70121-4
Meyer MP, Chow SSW, Alsweiler J, Bourchier D, Broadbent R, Knight D, Lynn AM, Patel H (2020) Probiotics for prevention of severe necrotizing enterocolitis: experience of New Zealand neonatal intensive care units. Front Pediatr 8(April):1–9. https://doi.org/10.3389/fped.2020.00119
Wang ZL, Liu L, Hu XY, Guo L, Li QY, An Y, Jiang YJ, Chen S, Wang XQ, He Y, Li LQ (2019) Probiotics may not prevent the deterioration of necrotizing enterocolitis from stage I to II/III. BMC Pediatr 19(1):1–7. https://doi.org/10.1186/s12887-019-1524-5
Drucker NA, McCulloh CJ, Li B, Pierro A, Besner GE, Markel TA (2018) Stem cell therapy in necrotizing enterocolitis: current state and future directions. Semin Pediatr Surg 27(1):57–64. https://doi.org/10.1053/j.sempedsurg.2017.11.011
McCulloh CJ, Olson JK, Wang Y et al (2018) Treatment of experimental necrotizing enterocolitis with stem cell-derived exosomes. J Pediatr Surg 53:1215–1220. https://doi.org/10.1016/j.jpedsurg.2018.02.086
Sim N Therapeutic controlled hypothermia in the treatment of neonates with severe necrotizing enterocolitis (CoolNEC). Bethesda (MD): ClinicalTrials.gov; 2011. doi:NCT01330576
De Almeida MFB, Guinsburg R, Sancho GA et al (2014) Hypothermia and early neonatal mortality in preterm infants. J Pediatr 164(2):271–276. https://doi.org/10.1016/j.jpeds.2013.09.049
Lyu Y, Shah PS, Ye XY, Warre R, Piedboeuf B, Deshpandey A, Dunn M, Lee SK, Canadian Neonatal Network (2015) Association between admission temperature and mortality and major morbidity in preterm infants born at fewer than 33 weeks’ gestation. JAMA Pediatr 169(4):4–11. https://doi.org/10.1001/jamapediatrics.2015.0277
de Siqueira Caldas JP, Ferri WAG, Marba STM, Aragon DC, Guinsburg R, de Almeida MFB, Diniz EMA, Silveira RCS, Alves Junior JMS, Pavanelli MB, Bentlin MR, Ferreira DMLM, Vale MS, Fiori HH, Duarte JLMB, Meneses JA, Cwajg S, Carvalho WB, Ferrari LSL, Silva NMM, da Silva RPGVC, Anchieta LM, Santos JPF, Kawakami MD (2019) Admission hypothermia, neonatal morbidity, and mortality: evaluation of a multicenter cohort of very low birth weight preterm infants according to relative performance of the center. Eur J Pediatr 178(7):1023–1032. https://doi.org/10.1007/s00431-019-03386-9
Chaudhary R, Farrer K, Broster S, Mcritchie L, Austin T (2013) Active versus passive cooling during neonatal transport. Pediatrics. 132(5):841–846. https://doi.org/10.1542/peds.2013-1686
Lin L, Xia X, Liu W, Wang Y, Hua Z (2019) Clinical characteristics of neonatal fulminant necrotizing enterocolitis in a tertiary Children’s hospital in the last 10 years. PLoS One 14(11):3–11. https://doi.org/10.1371/journal.pone.0224880
Robinson JR, Rellinger EJ, Hatch LD, Weitkamp JH, Speck KE, Danko M, Blakely ML (2017) Surgical necrotizing enterocolitis. Semin Perinatol 41(1):70–79. https://doi.org/10.1053/j.semperi.2016.09.020
Niemarkt HJ, De Meij TG, Van Ganzewinkel CJ et al (2019) Necrotizing enterocolitis, gut microbiota, and brain development: role of the brain-gut axis. Neonatology. 115(4):423–431. https://doi.org/10.1159/000497420
Biouss G, Antounians L, Li B, O’Connell JS, Seo S, Catania VD, Guadagno J, Rahman A, Zani-Ruttenstock E, Svergun N, Pierro A, Zani A (2019) Experimental necrotizing enterocolitis induces neuroinflammation in the neonatal brain. J Neuroinflammation 16(1):1–14. https://doi.org/10.1186/s12974-019-1481-9
Liu X, Wen S, Zhao S et al (2018) Mild therapeutic hypothermia protects the brain from ischemia/reperfusion injury through upregulation of iASPP. Aging Dis 9(3):401–411. https://doi.org/10.14336/AD.2017.0703
Cuna AC, Lee JC, Robinson AL, Allen NH, Foley JE, Chan SS (2018) Bowel ultrasound for the diagnosis of necrotizing enterocolitis: a meta-analysis. Ultrasound Q 34(3):113–118. https://doi.org/10.1097/RUQ.0000000000000342
Garami A, Steiner AA, Romanovsky AA (2018) “Fever and hypothermia in systemic inflammation.” In handbook of clinical neurology, 157:565–97. Elsevier B.V. https://doi.org/10.1016/B978-0-444-64074-1.00034-3
Neu J, Pammi M (2018) Necrotizing enterocolitis: the intestinal microbiome, metabolome and inflammatory mediators. Semin Fetal Neonatal Med 23(6):400–405. https://doi.org/10.1016/j.siny.2018.08.001
Ding W, Shen Y, Li Q, Jiang S, Shen H (2018) Therapeutic mild hypothermia improves early outcomes in rats subjected to severe sepsis. Life Sci 199(February):1–9. https://doi.org/10.1016/j.lfs.2018.03.002
Watkins C, Murphy K, Yen S, Carafa I, Dempsey EM, O’Shea CA, Vercoe EA, Ross RP, Stanton C, Ryan CA (2017) Effects of therapeutic hypothermia on the gut microbiota and metabolome of infants suffering hypoxic-ischemic encephalopathy at birth. Int J Biochem Cell Biol 93(April):110–118. https://doi.org/10.1016/j.biocel.2017.08.017
Prashantha YN, Suman Rao PN, Nesargi S et al. (2018) Therapeutic hypothermia for moderate and severe hypoxic ischaemic encephalopathy in newborns using low-cost devices – ice packs and phase changing material. Paediatr Int Child Health, 1–6. https://doi.org/10.1080/20469047.2018.1500805
Daetwyler K, Brotschi B, Berger TM, Wagner BP (2013) Feasibility and safety of passive cooling in a cohort of asphyxiated newborn infants. Swiss Med Wkly 143(March):1–6. https://doi.org/10.4414/smw.2013.13767
Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG, Cochrane Neonatal Group (2013) Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev 2013(1):CD003311. https://doi.org/10.1002/14651858.CD003311.pub3
Alsaied A, Islam N, Thalib L (2020) Global incidence of necrotizing Enterocolitis: a systematic review and meta-analysis. BMC Pediatr 20(1):344. https://doi.org/10.1186/s12887-020-02231-5
Acknowledgments
We acknowledge the preterm infants and his families who accepted contributed to this study and neonatology staff from Ribeirão Preto Medical School-University of São Paulo, who works with these patients.
Author information
Authors and Affiliations
Contributions
Walusa Assad Gonçalves–Ferri: Conception and design of the study. Statistical analysis. Contribution to analysis. Interpretation of data. Drafting of the study.
Cristina Helena Faleiros Ferreira. Acquisition of the data. Contribution to analysis Interpretation of data. Drafting of the study. Revising it critically for important intellectual content.
Laryssa de Carli: Acquisition of the data. Contribution to analysis Interpretation of data. Revising it critically for important intellectual content.
Thaissa Rodrigues Souza. Acquisition of the data. Contribution to analysis Interpretation of data. Revising it critically for important intellectual content.
Thayane de Castro Peres. Acquisition of the data. Contribution to analysis Interpretation of data. Revising it critically for important intellectual content.
Fabio Carmona. Conception and design. Acquisition of the data. Contribution to analysis Interpretation of data. Revising it critically for important intellectual content.
Davi Casale Aragon. Conception and design. Statistical analysis. Contribution to analysis Interpretation of data. Drafting of the study. Revising it critically for important intellectual content.
Gerson Crott. Acquisition of the data. Contribution to analysis Interpretation of data. Drafting of the study. Revising it critically for important intellectual content.
Marisa Mussi. Conception and design. Contribution to analysis Interpretation of data. Revising it critically for important intellectual content.
Jose Simon Camelo Junior. Contribution to analysis Interpretation of data. Drafting of the study. Revising it critically for important intellectual content.
Anelise Roosch. Contribution to analysis interpretation of data. Drafting of the study. Revising it critically for important intellectual content.
Lourenço Sbragia Neto: Contribution to analysis. Interpretation of data. Drafting of the study. Revising it critically for important intellectual content.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the study.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethics approval
This study was approved by the Institutional Review Board of Ribeirão Preto Medical School, University of São Paulo (FMRP-USP, CAAE number 29879620.5.0000.5440, approval number 3.920.223). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
N/A
Consent for publication
N/A
Additional information
Communicated by Daniele De Luca
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gonçalves-Ferri, W.A., Ferreira, C.H.F., Couto, L.d. et al. Low technology, mild controlled hypothermia for necrotizing enterocolitis treatment: an initiative to improve healthcare to preterm neonates.. Eur J Pediatr 180, 3161–3170 (2021). https://doi.org/10.1007/s00431-021-04014-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04014-1