Abstract
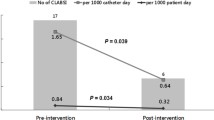
Central line–associated bloodstream infection (CLABSI) is a significant cause of morbidity and mortality in neonatal intensive care units (NICUs). A “bundle” is defined as a combination of evidence-based interventions that provided they are followed collectively and reliably, are proven to improve patient outcomes. The aim of this quasi-experimental study was to assess the impact of new central line insertion, dressing, and maintenance “bundles” on the rate of CLABSI and catheter-related complications. We performed a quality improvement (QI), prospective, before-after study. In the first 9-month period, the old “bundles” and pre-existing materials were used/applied. An intervention period then occurred with changes made to materials used and the implementation of new “bundles” related to various aspects of central lines care. A second 6-month period was then assessed and the CLABSI rates were measured in the NICU pre- and post-intervention period. The QI measures were the rate of CLABSI and catheter-related complications. Data are still being collected after the study to verify sustainability. The implementation of the new “bundles” and the change of certain materials resulted in a significantly decreased rate of CLABSI (8.4 to 1.8 infections per 1000 central venous catheter (CVC) days, p = 0.02,) as well as decreased catheter-related complications (47 to 10, p < 0.007).
Conclusions: The analysis of pre-existing “bundles” and the implementation of updated central line “bundles” based on best practice recommendations are crucial for reducing the rate of CLABSI in the NICU. The implementation of the new evidence-based central line “bundles” was associated with a significant reduction in CLABSI rate in our unit soon after implementation.
What is Known: • Central line–associated bloodstream infection (CLABSI) is a major cause of morbidity and mortality in the neonatal population. • The implementation of evidence-based “bundles” in the NICU is associated with a reduction in the incidence of CLABSI. | |
What is New: • For the improvement in quality care in the NICU, audits are necessary to assess the existing systems. • The “Plan-Do-Study-Act cycle” is an effective tool to use when tackling challenges in an existing system. Using this tool assisted in the approach to reducing CLABSI in our NICU. |








Similar content being viewed by others
Abbreviations
- CVC:
-
Central venous catheter
- CLABSI:
-
Central line–associated bloodstream infection
- CRBSI:
-
Catheter-related bloodstream infection
- NICU:
-
Neonatal intensive care unit
- VLBW:
-
Very low birth weight
- ELBW:
-
Extremely low birth weight
- QI:
-
Quality improvement
- UVC:
-
Umbilical venous catheter
- CICC:
-
Centrally inserted central venous catheter
- ECCs:
-
Epicutaneo-cava catheters
- CDC:
-
Centers for Disease Control and Prevention
References
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
Payne V, Hall M, Prieto J, Johnson M (2018) Care bundles to reduce central line-associated bloodstream infections in the neonatal unit: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 103:F422–F429
Adams-Chapman I, Stoll BJ (2006) Neonatal infection and long-term neurodevelopmental outcome in the preterm infant. Curr Opin Infect Dis 19:290–297
Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA, Hintz SR, Vohr B, Higgins RD, National Institute of Child H, Human Development Neonatal Research N (2004) Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 292:2357–2365
Shah DK, Doyle LW, Anderson PJ, Bear M, Daley AJ, Hunt RW, Inder TE (2008) Adverse neurodevelopment in preterm infants with postnatal sepsis or necrotizing enterocolitis is mediated by white matter abnormalities on magnetic resonance imaging at term. J Pediatr 153:170–175 175 e171
Mahieu LM, Buitenweg N, Beutels P, De Dooy JJ (2001) Additional hospital stay and charges due to hospital-acquired infections in a neonatal intensive care unit. J Hosp Infect 47:223–229
Goudie A, Dynan L, Brady PW, Rettiganti M (2014) Attributable cost and length of stay for central line-associated bloodstream infections. Pediatrics 133:e1525–e1532
Bannatyne M, Smith J, Panda M, Abdel-Latif ME, Chaudhari T (2018) Retrospective cohort analysis of central line associated blood stream infection following introduction of a central line bundle in a neonatal intensive care unit. Int J Pediatr 2018:4658181
Emoli A, Cappuccio S, Marche B, Musaro A, Scoppettuolo G, Pittiruti M, Gruppo Aperto di Studio sugli Accessi Venosi Centrali a Lungo T (2014) The ISP (safe insertion of PICCs) protocol: a bundle of 8 recommendations to minimize the complications related to the peripherally inserted central venous catheters (PICC). Assist Inferm Ric 33:82–89
Graham PL 3rd (2010) Simple strategies to reduce healthcare associated infections in the neonatal intensive care unit: line, tube, and hand hygiene. Clin Perinatol 37:645–653
Pittet D, Allegranzi B, Boyce J, World Health Organization World Alliance for Patient Safety First Global Patient Safety Challenge Core Group of E (2009) The World Health Organization guidelines on hand hygiene in health care and their consensus recommendations. Infect Control Hosp Epidemiol 30:611–622
Ista E, van der Hoven B, Kornelisse RF, van der Starre C, Vos MC, Boersma E, Helder OK (2016) Effectiveness of insertion and maintenance bundles to prevent central-line-associated bloodstream infections in critically ill patients of all ages: a systematic review and meta-analysis. Lancet Infect Dis 16:724–734
Schmid S, Geffers C, Wagenpfeil G, Simon A (2018) Preventive bundles to reduce catheter-associated bloodstream infections in neonatal intensive care. GMS Hyg Infect Control 13:10
Kinoshita D, Hada S, Fujita R, Matsunaga N, Sakaki H, Ohki Y (2019) Maximal sterile barrier precautions independently contribute to decreased central line-associated bloodstream infection in very low birth weight infants: a prospective multicenter observational study. Am J Infect Control 47:1365–1369
Raad II, Hohn DC, Gilbreath BJ, Suleiman N, Hill LA, Bruso PA, Marts K, Mansfield PF, Bodey GP (1994) Prevention of central venous catheter-related infections by using maximal sterile barrier precautions during insertion. Infect Control Hosp Epidemiol 15:231–238
Leistner R, Piening B, Gastmeier P, Geffers C, Schwab F (2013) Nosocomial infections in very low birthweight infants in Germany: current data from the National Surveillance System NEO-KISS. Klin Padiatr 225:75–80
Garcia H, Martinez-Munoz AN, Peregrino-Bejarano L (2014) Epidemiology of nosocomial infections in a neonatal intensive care unit. Rev Med Inst Mex Seguro Soc 52 Suppl 2:S30-S37
Sharpe E, Kuhn L, Ratz D, Krein SL, Chopra V (2017) Neonatal peripherally inserted central catheter practices and providers: results from the Neonatal PICC1 Survey. Adv Neonatal Care 17:209–221
Di Puccio F, Giacomarro D, Mattei L, Pittiruti M, Scoppettuolo G (2018) Experimental study on the chemico-physical interaction between a two-component cyanoacrylate glue and the material of PICCs. J Vasc Access 19:58–62
Barone G, Pittiruti M (2019) Epicutaneo-caval catheters in neonates: new insights and new suggestions from the recent literature. J Vasc Access:1129729819891546
Zhang S, Guido AR, Jones RG, Curry BJ, Burke AS, Blaisdell ME (2019) Experimental study on the hemostatic effect of cyanoacrylate intended for catheter securement. J Vasc Access 20:79–86
Scoppettuolo G, Dolcetti L, Emoli A, La Greca A, Biasucci DG, Pittiruti M (2015) Further benefits of cyanoacrylate glue for central venous catheterisation. Anaesthesia 70:758
Waller SC, Anderson DW, Kane BJ, Clough LA (2019) In vitro assessment of microbial barrier properties of cyanoacrylate tissue adhesives and pressure-sensitive adhesives. Surg Infect 20:449–452
Salzman MB, Isenberg HD, Shapiro JF, Lipsitz PJ, Rubin LG (1993) A prospective study of the catheter hub as the portal of entry for microorganisms causing catheter-related sepsis in neonates. J Infect Dis 167:487–490
Breimer L, Geijer H, Berggren L (2018) Disinfection of injection ports - a systematic overview of optimal scrub-time. Lakartidningen 115
Bjorkman L, Ohlin A (2015) Scrubbing the hub of intravenous catheters with an alcohol wipe for 15 sec reduced neonatal sepsis. Acta Paediatr 104:232–236
Gutierrez Nicolas F, Nazco Casariego GJ, Vina Romero MM, Gonzalez Garcia J, Ramos Diaz R, Perez Perez JA (2016) Reducing the degree of colonisation of venous access catheters by continuous passive disinfection. Eur J Hosp Pharm 23:131–133
Casey AL, Karpanen TJ, Nightingale P, Elliott TSJ (2018) An in vitro comparison of standard cleaning to a continuous passive disinfection cap for the decontamination of needle-free connectors. Antimicrob Resist Infect Control 7:50
Sengupta A, Lehmann C, Diener-West M, Perl TM, Milstone AM (2010) Catheter duration and risk of CLA-BSI in neonates with PICCs. Pediatrics 125:648–653
Milstone AM, Reich NG, Advani S, Yuan G, Bryant K, Coffin SE, Huskins WC, Livingston R, Saiman L, Smith PB, Song X (2013) Catheter dwell time and CLABSIs in neonates with PICCs: a multicenter cohort study. Pediatrics 132:e1609–e1615
Erdei C, McAvoy LL, Gupta M, Pereira S, McGowan EC (2015) Is zero central line-associated bloodstream infection rate sustainable? A 5-year perspective. Pediatrics 135:e1485–e1493
Schulman J, Stricof R, Stevens TP, Horgan M, Gase K, Holzman IR, Koppel RI, Nafday S, Gibbs K, Angert R, Simmonds A, Furdon SA, Saiman L, New York State Regional Perinatal Care C (2011) Statewide NICU central-line-associated bloodstream infection rates decline after bundles and checklists. Pediatrics 127:436–444
Author information
Authors and Affiliations
Contributions
SB and FP designed and wrote the article.
KC collected the data.
OD revised the manuscript for intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 40 kb)
Rights and permissions
About this article
Cite this article
Bierlaire, S., Danhaive, O., Carkeek, K. et al. How to minimize central line–associated bloodstream infections in a neonatal intensive care unit: a quality improvement intervention based on a retrospective analysis and the adoption of an evidence-based bundle. Eur J Pediatr 180, 449–460 (2021). https://doi.org/10.1007/s00431-020-03844-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-020-03844-9