Abstract
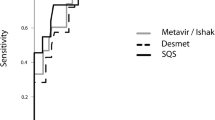
The objectives of this prospective case-control study were to determine liver stiffness (LSM) by transient elastography (TE) in children with newly diagnosed chronic liver disease (CLD) and to find out normal values in healthy Indian children. Two groups (A: 50 CLD who underwent liver biopsy and B: 50 healthy) aged 5–18 years were recruited prospectively. Liver biopsies were scored as per Metavir scoring and compared with TE. The median age of 100 recruited children was 13.6 years. In group B, normal LSM was 4.9 (2.5–7.3) kPa with significantly higher LSM in adolescent males (5.6 (4.1–7.3) kPa) as compared with females (4.3 (3.7–4.9) kPa), p = 0.001. In group A, TE was excellent in discriminating significant fibrosis (≥ F2) (P = 0.001) at a cut-off value of 10.6 kPa with area under receiver operating characteristic curve of 0.96. Metavir fibrosis stage (β = 0.611; R2 = 0.586) and age (β = 0.230; R2 = 0.586) were independent variables associated with higher LSM in stepwise multiple logistic regression analysis.
Conclusions: TE is an excellent non-invasive tool to assess significant liver fibrosis and can be used as an alternative to liver biopsy. Normative value of TE in adolescent males is higher than in females.
What is Known: • Transient elastography is a good non-invasive test for liver fibrosis assessment. • Normal liver stiffness depends on race, gender, and age. | |
What is New: • This is the first study from India to show the normative data of transient elastography in healthy Indian children. • We have documented that liver stiffness measurement by fibroscan in treatment naïve chronic liver disease has excellent correlation in significant fibrosis, severe fibrosis, and cirrhosis. |

Similar content being viewed by others
Change history
26 February 2020
The author regrets that one of the author’s name was incorrectly presented in the published version of this article. The third author’s name original read as “<Emphasis Type="Bold">Tajwar Singh Negi</Emphasis>” this should have been “<Emphasis Type="Bold">Tajwer Singh Negi</Emphasis>”.
Abbreviations
- AUROC:
-
Area under the receiver operating characteristic
- ANA:
-
Anti-nuclear antibody
- Anti HBe:
-
Antibody to hepatitis B e-antigen
- BMI:
-
Body mass index
- CLD:
-
Chronic liver disease
- CTP:
-
Child–Turcotte–Pugh
- EGD:
-
Esophagogastroduodenoscopy
- HBsAg:
-
Hepatitis B surface antigen
- HBeAg:
-
Hepatitis B e-antigen
- HBV-DNA:
-
Hepatitis B deoxyribonucleic acid
- HCV RNA:
-
Hepatitis C ribonucleic acid
- IQR:
-
Interquartile range
- LSM:
-
Liver stiffness measurement
- LKM:
-
Liver kidney microsomal antibody
- MELD:
-
Model for end-stage liver disease
- NAFLD:
-
Non-alcoholic fatty liver disease
- PELD:
-
Pediatric end-stage liver disease
- ROC:
-
Receiver operating characteristic
- SMA:
-
Anti-smooth muscle antibody
- TE:
-
Transient elastography
References
Sokol RJ (2002) Liver cell injury and fibrosis. J Pediatr Gastroenterol Nutr 35(1):S7–S10
Tanner MS (2002) Mechanisms of liver injury relevant to pediatric hepatology. Crit Rev Clin Lab Sci 39:1–61. https://doi.org/10.1080/10408360290795439
Sun Y, Zhou J, Wang L et al (2017 May) New classification of liver biopsy assessment for fibrosis in chronic hepatitis B patients before and after treatment. Hepatology. 65(5):1438–1450. https://doi.org/10.1002/hep.29009
Cadranel JF, Rufat P, Degos F (2000) Practices of liver biopsy in France: results of a prospective nationwide survey. For the Group of Epidemiology of the French Association for the Study of the liver (AFEF). Hepatology 32:477–481. https://doi.org/10.1053/jhep.2000.16602
Poniachik J, Bernstein DE, Reddy KR, Jeffers LJ, Coelho-Little ME, Civantos F, Schiff ER (1996) The role of laparoscopy in the diagnosis of cirrhosis. Gastrointest Endosc 43:568–571. https://doi.org/10.1016/s0016-5107(96)70192-x
CasteraL VJ, Foucher J, Le Bail B, Chanteloup E, Haaser M, Darriet M, Couzigou P, De Ledinghen V (2005) Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology 128:343–350. https://doi.org/10.1053/j.gastro.2004.11.018
Corpechot C, El Naggar A, Poujol-Robert A, Ziol M, Wendum D, Chazouillères O, de Lédinghen V, Dhumeaux D, Marcellin P, Beaugrand M, Poupon R (2006) Assessment of biliary fibrosis by transient elastography in patients with PBC and PSC. Hepatology 43:1118–1124. https://doi.org/10.1002/hep.21151
Foucher J, Chanteloup E, Vergniol J, Castéra L, Le Bail B, Adhoute X, Bertet J, Couzigou P, de Ledinghen V (2006) Diagnosis of cirrhosis by transient elastography (FibroScan): a prospective study. Gut 55:403–408. https://doi.org/10.1136/gut.2005.069153
Kazemi F, Kettaneh A, N’kontchou G, Pinto E, Ganne-Carrie N, Trinchet JC, Beaugrand M (2006) Liver stiffness measurement selects patients with cirrhosis at risk of bearing large oesophageal varices. J Hepatol 45:230–235. https://doi.org/10.1016/j.jhep.2006.04.006
Carrion JA, Navasa M, Bosch J, Bruguera M, Gilabert R, Forns X (2006) Transient elastography for diagnosis of advanced fibrosis and portal hypertension in patients with hepatitis C recurrence after liver transplantation. Liver Transpl 12:17918. https://doi.org/10.1002/lt.20857
deLedinghen V, Le Bail B, Rebouissoux L, Fournier C, Foucher J, Miette V, Castéra L, Sandrin L, Merrouche W, Lavrand F, Lamireau T (2007) Liver stiffness measurement in children using FibroScan: feasibility study and comparison with Fibrotest, aspartate transaminase to platelets ratio index, and liver biopsy. J Pediatr Gastroenterol Nutr 45:443–450. https://doi.org/10.1097/MPG.0b013e31812e56ff
Nobili V, Vizzutti F, Arena U, Abraldes JG, Marra F, Pietrobattista A, Fruhwirth R, Marcellini M, Pinzani M (2008) Accuracy and reproducibility of transient elastography for the diagnosis of fibrosis in pediatric nonalcoholic steatohepatitis. Hepatology 48:442–448. https://doi.org/10.1002/hep.22376
Alkhouri N, Sedki E, Alisi A, Lopez R, Pinzani M, Feldstein AE, Nobili V (2013) Combined pediatric NAFLD fibrosis index and transient elastography to predict clinically significant fibrosis in children with fatty liver disease. Liver Int 33:79–85. https://doi.org/10.1111/liv.12024
Fitzpatrick E, Quaglia A, Vimalesvaran S, Basso MS, Dhawan A (2013) Transient elastography is a useful noninvasive tool for the evaluation of fibrosis in pediatric chronic liver disease. J Pediatr Gastroenterol Nutr 56:72–76. https://doi.org/10.1097/MPG.0b013e31826f2760
Raizner A, Shillingford N, Mitchell PD, Harney S, Raza R, Serino J, Jonas MM, Lee CK (2017) Hepatic inflammation may influence liver stiffness measurements by transient elastography in children and young adults. J Pediatr GastroenterolNutr 64(4):512–517. https://doi.org/10.1097/MPG.0000000000001376
Engelmann G, Gebhardt C, Wenning D, Wühl E, Hoffmann GF, Selmi B, Grulich-Henn J, Schenk JP, Teufel U (2012) Feasibility study and control values of transient elastography in healthy children. Eur J Pediatr 171:353–360. https://doi.org/10.1007/s00431-011-1558-7
Goldschmidt I, Streckenbach C, Dingemann C, Pfister ED, di Nanni A, Zapf A, Baumann U (2013) Application and limitations of transient liver elastography in children. J Pediatr Gastroenterol Nutr 57:109–113. https://doi.org/10.1097/MPG.0b013e31829206a0
Lewindon PJ, Balouch F, Pereira TN, Puertolas-Lopez MV, Noble C, Wixey JA, Ramm GA (2016) Transient liver elastography in unsedated control children: impact of age and intercurrent illness. J Paediatr Child Health 52:637–642. https://doi.org/10.1111/jpc.13151
Lee CK, Mitchell PD, Raza R, Harney S, Wiggins SM, Jonas MM (2018) Validation of transient elastography cut points to assess advanced liver fibrosis in children and young adults: the Boston Children’s Hospital experience. J Pediatr 198:84–89.e2. https://doi.org/10.1016/j.jpeds.2018.02.062
Mileti E, Rosenthal P, Peters MG (2012) Validation and modification of simplified diagnostic criteria for autoimmune hepatitis in children. Clin Gastroenterol Hepatol 10:417–421. https://doi.org/10.1016/j.cgh.2011.11.030
Lok AS, McMahon BJ (2007) Chronic hepatitis B. Hepatology 45:507–539. https://doi.org/10.1002/hep.21513
Ghany MG, Strader DB, Thomas DL, Seeff LB, American Association for the study of Liver Disease (2009) Diagnosis, management andtreatment of hepatitis C: an update. Hepatology 49:1335–1374. https://doi.org/10.1002/hep.22759
Roberts EA, Schilsky ML (2008) Diagnosis and treatment of Wilson disease: an update. Hepatology 47:2089–2111. https://doi.org/10.1002/hep.22261
Valla DC (2003) The diagnosis and management of the Budd-Chiari syndrome: consensus and controversies. Hepatology 38:793–803. https://doi.org/10.1053/jhep.2003.50415
Foucher J, Castéra L, Bernard PH, Adhoute X, Laharie D, Bertet J, Couzigou P, de Lédinghen V (2006) Prevalence and factors associated with failure of liver stiffness measurement using FibroScan in a prospective study of 2114 examinations. Eur J Gastroenterol Hepatol 18:411–412
Bedossa P, Poynard T (1996) An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology 24:289–293. https://doi.org/10.1002/hep.510240201
Kalantri A, Karambelkar M, Joshi R, Kalantri S, Jajoo U (2010) Accuracy and reliability of pallor for detecting anaemia: a hospital-based diagnostic accuracy study. PLoS One 5(1):e8545. https://doi.org/10.1371/journal.pone.0008545
Yasuda M, Shimizu I, Shiba M, Ito S (1999) Suppressive effects of estradiol on dimethylnitrosamine-induced fibrosis of the liver in rats. Hepatology 29:719–727. https://doi.org/10.1002/hep.510290307
Mederacke I, Wursthorn K, Kirschner J, Rifai K, Manns MP, Wedemeyer H, Bahr MJ (2009) Food intake increases liverstiffness in patients with chronic or resolved hepatitis C virus infection. Liver Int 29:1500–1506. https://doi.org/10.1111/j.1478-3231.2009.02100.x
Cho Y, Tokuhara D, Morikawa H, Kuwae Y, Hayashi E, Hirose M, Hamazaki T, Tanaka A, Kawamura T, Kawada N, Shintaku H (2015) Transient elastography-based liver profiles in a hospital-based pediatric population in Japan. PLoS One 10:e0137239. https://doi.org/10.1371/journal.pone.0137239
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Vikas Jain, Ujjal Poddar, Negi TS, Vivek A Saraswat, Narendra Krishnani, Surender K Yachha, and Anshu Srivastav. The first draft of the manuscript was written by Vikas Jain and Ujjal Poddar. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. The study was conducted after obtaining clearance from the Institutional Ethics Committee (IEC code: 2014-83-DM-77). Informed written consent was obtained from either parent before doing all invasive procedures and TE. Informed consent: Informed written consent was obtained from either parent before doing all invasive procedures and transient elastography.
Additional information
Communicated by Peter de Winter
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The author regrets that one of the author’s name was incorrectly presented in the published version of this article. The third author’s name original read as “Tajwer Singh Negi”, this should have been “Tajwar Singh Negi”.
Rights and permissions
About this article
Cite this article
Jain, V., Poddar, U., Negi, T.S. et al. Utility and accuracy of transient elastography in determining liver fibrosis: a case-control study. Eur J Pediatr 179, 671–677 (2020). https://doi.org/10.1007/s00431-019-03561-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03561-y