Abstract
Bone health is extremely important in early childhood because children with low bone mineral density (BMD) are at a greater risk of bone fractures. While physical activity and intake of both calcium and vitamin D benefit BMD in older children, there is limited research on the determinants of good bone health in early childhood. The aim of this cross-sectional study was to investigate the impact of diet, physical activity, and body composition on BMD at five years of age. Dietary intakes and physical activity levels were measured through questionnaires. Whole body BMD was measured by dual-energy X-ray absorptiometry in 102 children. Child weight, height, circumferences, skinfolds and serum 25-hydroxyvitamin D (25OHD) concentrations were assessed. There was no association between BMD and dietary calcium, dietary vitamin D, 25OHD, physical activity, or sedentary behaviour. Several measures of body composition were significantly positively associated with BMD; however, neither fat mass nor lean body mass was associated with BMD.
Conclusion: Although we found no association between self-reported dietary and lifestyle factors and bone health in early years, increased body size was linked with higher BMD. These findings are important as identifying modifiable factors that can improve bone health at a young age is of utmost importance.
What is Known: • Bone health is extremely important in early childhood, as children with low bone mineral density (BMD) are at greater risk of bone fractures. • Physical activity has been found to be beneficial for bone health in adolescents, and body composition has also been associated with BMD in teenage years. • Limited research on the determinants of good bone health in early childhood. | |
What is New: • No association between self-reported lifestyle and dietary factors with bone health in early childhood. • Increased body size was associated with higher BMD at five years of age. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During normal childhood and adolescence, the skeleton undergoes tremendous change. Unlike the adult skeleton where bone remodelling is the dominant activity, the younger skeleton is both growing and remodelling. It is estimated that more than half of peak bone mass is acquired during the teenage years [1]. Thus, factors that influence bone health during early life are extremely important. Dual-energy X-ray absorptiometry (DXA) is the best measure of bone health by estimating areal bone mineral density (BMD) and areal bone mineral content (BMC) [28]. Children with low BMD are at higher risk of fractures throughout childhood [7]. Individuals with low BMD in childhood who have concomitant multiple bone fractures are also at a higher risk of being diagnosed with osteoporosis in later life [21]. In order to delay the onset of osteoporosis, it is vital to ensure that BMD is at an optimum level throughout childhood and adolescence.
Heredity is the principal determinant of BMD [10, 22, 36], but identifying modifiable factors has the potential for benefit. The relationship between bone health and diet is well established, particularly focusing on calcium and vitamin D [23, 30, 41,42,43]. Since effective sunlight exposure in Ireland is curtailed to 7 months yearly, oral intake of vitamin D from all sources (natural foodstuffs, fortified foods and supplements) is essential to maintain serum 25-hydroxyvitamin D (25OHD) levels year round [6]. Calcium intake in Ireland tends to be at the high end of the international spectrum in adults in view of the ready availability of dairy products but intake can vary widely [3]. Physical activity has a positive association with BMD in children and adolescents [5, 16, 44]. An intervention study demonstrated that a school-based jumping programme significantly increased BMD in prepubertal boys and girls [31, 32].
The association between body composition and bone health is conflicting. In adults, BMD had a stronger relationship with lean body mass than with fat mass [19, 39]. It has been suggested that adipose tissue is not beneficial to bone structure in healthy mature adolescents and young adults [18, 34]. However, in prepubertal children, it is proposed that adipose tissue may stimulate bone growth [8], and it has been reported that fat mass was positively associated with bone mass in children [24, 38].
The aim of this research project is to provide insight into modifiable factors that may be related to bone health in preschool-aged Irish children. Based on secondary analysis of data from the ROLO Kids Study, we aimed to investigate the associations between diet, physical activity and body composition with child bone mineral density in 5-year-old children.
Methods
Study design and population
The ROLO Study was a randomised controlled trial of a low glycaemic index diet during pregnancy, with the aim of reducing foetal macrosomia. In the study, 800 mothers were recruited that had previously given birth to a macrosomic child (birth weight > 4 kg) and had no adverse health conditions. Mothers were randomised into an intervention or control group, where the intervention group received low glycaemic index dietary advice to follow during pregnancy, and the control arm had routine antenatal care. Findings from the ROLO Study and follow-up studies have previously been published [14, 29, 40], but in brief, there was no significant difference in birth weight between the control and intervention groups. Women in the intervention group did, however, reduce their gestational weight gain and improve their glycaemic control. The mothers and infants from this study were then followed up as part of the longitudinal ROLO Kids Study. Mothers were contacted and invited to take part in this analysis when their child turned 5 years of age. Written maternal consent was obtained at the follow-up visit and this study received ethical approval by the Ethics Committee in Our Lady’s Children Hospital, Dublin. Participants were eligible for this analysis if they had taken part in the ROLO Kids Study and had a DXA scan as part of the follow-up. A total of 102 mother and child dyads were included in this secondary analysis.
BMD and body composition measurements
BMD of the mother and child was measured by DXA using the Lunar iDXATM scanner (GE Healthcare, Madison WI) with enCORETM v.14.1 software. Measurements obtained by DXA included BMD (g/cm2), fat mass (kg) and lean mass (kg). Fat mass as a percentage of whole-body tissue was derived. In order to minimise the effect of operator variability factor, one or other of two qualified observers analysed all scans at 5 years follow-up. In terms of clinically relevant findings, based on a sample size calculation, to detect 1 standard deviation (SD) difference in BMD in our cohort, 17 participants are required per group (e.g. 17 males, 17 females) for 80% power at 0.05 level of significance.
Dietary measurements
The children’s mothers completed a food frequency questionnaire (FFQ) on behalf of their child. This measured their child’s habitual dietary intakes over the previous year. The FFQ was divided into different categories—breads/pastas, cakes/confectionary, dairy, sugar sweetened beverages, fruit/vegetables, spreads and meat/fish—and asked mothers to report how frequently their child consumed each food product in the last year. The FFQ was based on the Growing up in Ireland 5-Year Primary Caregiver Main Questionnaire [12] and was a validated method of assessing dietary intakes in children. Using McCance and Widdowson’s The Composition of Foods Seventh Summary Edition [35], habitual dietary intakes of calcium and vitamin D were calculated in milligram per day (mg/day) and microgram per day (μg/day), respectively.
Physical activity and sedentary behaviour
Mothers also completed the Children’s Leisure and Activity Study Survey (CLASS) questionnaire on behalf of their child. The CLASS questionnaire is a baseline proxy report of typical week physical activity and sedentary behaviour questionnaire. This is a validated questionnaire estimating habitual physical activity and sedentary activity levels in children [17]. The CLASS questionnaire also estimated the amount of screen time the child had each week, which was used as a proxy for sedentary behaviour.
Anthropometric measurements
The height and weight of the child was measured using a SECA stadiometer (to the nearest 0.1 cm) and a SECA scales (to the nearest 0.1 kg), respectively, and body mass index (BMI) was calculated as kilogram per square metre (kg/m2), along with standardised scores and centiles, which was scored using the definitions set by the Centre for Disease Control and Prevention [4]. These measurements and calculations were all carried out by the trained research team. Circumferences of the head, neck, mid-upper arm (MUA), chest, abdomen, hip and thigh were measured using a SECA ergonomic circumference measuring tape (to the nearest 0.1 cm). Skinfold measurements of the biceps, triceps, subscapular and thigh were collected (to the nearest 0.2 mm) using a Holtain skinfold caliper, and subscapular to triceps ratio, sum of skinfolds and subscapular and triceps skinfold thicknesses as markers of adiposity were calculated.
25OHD measurement
Blood samples (n = 32) were collected at the follow-up visit by a trained phlebotomist. 25OHD concentrations were quantified using the Elecsys Vitamin D Total (Roche Diagnostics GmbH, Mannheim, Germany) automated competitive binding protein assay.
Statistical analysis
The distribution and normality of each variable was determined by visual assessment of histograms. Mean and SD were reported for normally distributed data with median and interquartile range (IQR) being reported for non-normal data. To measure unadjusted correlations between each variable and the child’s BMD, Pearson’s correlation was used for normally distributed data and Spearman’s correlation for non-normal data to explore the relationship. A significance level of p < 0.05 was used to set a cut-off for further analysis with each variable. Multiple regression analysis was then used to identify the extent of the relationship between child BMD and each variable with a significant correlation, while controlling the following confounders: child sex, maternal BMD, maternal education level (as a marker of socioeconomic status) and whether the child was breastfed or not. Each variable was run individually with its own model, with 12 models being created in total. The population was dichotomized based on child’s adherence to recommended nutrient intakes (> 800 mg/day calcium, > 5 μg/day vitamin D, optimal serum 25OHD status (> 50 nmol/L), physical activity (> 420 min/week), screen time (< 1 h/day) and BMI normal weight status (< 85th percentile). Differences in BMD between these groups were assessed using independent sample t tests for normally distributed data and Mann-WhitneyU tests for non-normal data. All analysis was carried out using the Statistical Package for the Social Sciences (SPSS) version 24 (SPSS Inc., Chicago, USA).
Results
Descriptive statistics
The mean age of participants in this cohort was 5.09 years (51% female) and they were all Caucasian, with one being of Asian descent, with highly educated mothers, over 60% having completed third-level education (Table 1). There was no significant difference in any potential confounding factors between the sexes; however, there was a significant difference in BMD with males having a significantly higher BMD than females (p < 0.01).
Comparing between males and females, there was no difference in calcium or vitamin D intake, 25OHD concentration, physical/sedentary activity or body mass index (BMI)(Table 2). However, there were differences in body composition; male children had significantly higher head, neck and chest circumferences than females, while females had higher thigh circumferences and central adiposity measurements (p < 0.01).
The mean calcium intake across the population was 824 mg with 866 mg and 787 mg being the mean intake for male and female participants, respectively. The median vitamin D intake was 1.83 μg with similar intakes found between males and females (p = 0.931) Reported physical activity and screen time levels were 500 min/week and 600 min/week, respectively.
Achieving recommended intakes
Almost half of the participants met the Irish recommended daily allowance for calcium intake for children of 800 mg/day [3], whereas only 6% had an adequate vitamin D intake of 5 ug/day(Table 3) [13]. Over 68% of the children were reported to exercise for more than 420 min/week [11] but just over a quarter had the recommended less than 1 hour of screen time/day [9]. Over 80% of the study population were within the ranges for a healthy BMI centile (< 85th centile) with almost 20% being in the overweight (85th–95th) or obese category (> 95th BMI centile).
Associations with BMD
Neither meeting calcium recommendations having adequate 25OHD concentrations, nor meeting physical activity recommendations was significantly associated with BMD at 5 years of age (p > 0.05, Table 4). BMD was significantly lower in children who were in the normal weight category (< 85th BMI centile) than those who were in the overweight category (> 85th BMI centile) (p < 0.01). When the participants were split into male and female categories, this relationship with BMD and BMI centile was only seen in female participants (p < 0.01).
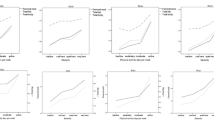
Unadjusted correlations
All dietary factors, physical and sedentary activity and anthropometric measurements were then correlated with BMD, for the total group and according to each sex (Table 5). In the total group, no dietary factors were significantly correlated with BMD. Physical activity was not significantly correlated with BMD; however, body composition was significantly correlated with BMD at five years of age. Weight (p < 0.01), length (p < 0.05), BMI, weight centile and BMI centile (all p < 0.01), and all circumferences were positively correlated with BMD. Although triceps skinfold (p < 0.01 = 0.000), subscapular skinfold (p < 0.01), sum of skinfolds (p < 0.01) and triceps and subscapular skinfold (p < 0.01) were positively correlated with BMD in females, no skinfold or adiposity measurement was significantly associated with BMD in the total population.
Multiple regression analysis
In total, 12 separate multiple regression models were created to estimate BMD using measures of body composition, all of which are summarised in Table 6. Apart from abdominal circumference, lean body mass and fat mass, all body composition measurements were significant at p < 0.05 level, when all confounding factors were controlled.
Discussion
In this study, we aimed to investigate the associations of diet, physical activity and body composition with child BMD at 5 years of age. For dietary intakes, there was no evidence for an association with BMD at 5 years of age. Similarly, no evidence was found for an association between parental-reported physical activity levels or sedentary behaviour on child BMD. However, we found strong evidence for an association between body composition at 5 years of age and child BMD, particularly with weight, child BMI and body circumferences.
According to a recent American study, the proportion of 4–8 years old children meeting the 800 mg/day recommendation of calcium is 80% in boys and 67% in girls [2]. Our findings suggest that Irish children are behind their American counterparts for calcium intake. However, after splitting the population into those who met and did not meet the recommended 800 mg (47% vs 53%), we found no significant difference in BMD between these two groups. Other studies have, however, reported an association between calcium supplementation and BMD [23, 25]. Similar results were seen in relation to vitamin D intake. The frequency of adequate dietary intake of vitamin D was much lower than calcium intake, with only 6% of the study cohort meeting recommendations of a daily intake of 5 μg. This is not uncommon in young children; European reports estimate that up to 40% of children have inadequate D status [6]. Although vitamin D supplementation has shown no effect on BMD in children with adequate vitamin D intakes [41, 42], an on-going study in vitamin D-deficient children should provide an interesting outlook on vitamin D’s effect on child bone health [43]. Taking this into account, further research into habitual dietary calcium and vitamin D intakes and bone health in young children is required.
While we found no association between physical activity levels and child BMD, intervention studies which implemented an exercise activity or studies which compared children who engage in a competitive sport with untrained controls showed significant associations between physical activity and higher BMD [37, 44]. As our population had a high level of physical activity, this may make it difficult to identify associations. Other research indicates how important physical activity can be when looking to optimise bone accrual and the importance of regular exercise during childhood cannot be dismissed. We also found that parental-reported sedentary behaviour had no association with BMD, which is comparable with current research. Recent studies suggested that only objectively measured sedentary time, using methods like accelerometers, was negatively associated with lower extremity bone outcomes in schoolchildren and that subjectively measured sedentary time (use of questionnaires) had no association with bone outcomes [20]. Although our results are in line with current research, it’s important to note that this relates to screen time as a measure of sedentary behaviour. Other characteristics of sedentary behaviour such as being in a sitting, reclining or lying posture may also have a significant effect on BMD. Even though sedentary behaviour was not strongly associated with a decrease in bone health, and our findings suggest no association between physical activity and BMD, interventions in other studies have shown how influential physical activity can be to bone health [26, 27]. Therefore, replacing sedentary activities with increased physical activity during childhood and adolescence could prove to have a prolific effect on bone health and aid the optimisation of bone accrual amidst this crucial growth phase.
We found that child body composition at 5 years of age was significantly associated with BMD. Eighty percent of our cohort was classified as having a healthy BMI. These findings are parallel with recent Irish figures, which estimate that 1 in 4 children is overweight or has obesity in Ireland [33], and US figures, stating that 16% of 2–5-year-old children are overweight or have obesity [15]. Results from our study support the theory that increased body mass leads to increased bone strength, since weight, BMI, weight centile and BMI centile were all significantly positively correlated with BMD (all p < 0.001) and remained statistically significant when all confounders were controlled. Although overall weight and circumferences had a significant association with child BMD, neither lean body mass nor fat mass was associated. Current research investigating the impact of fat mass on BMD is conflicting, while lean body mass has been shown to have a positive relationship with bone health [19, 39]. Previous studies have concluded that adipose tissue was not beneficial to bone structure [18, 34], while another study suggested that fat mass is on the causal pathway, having a positive relationship with bone mass in children [38].
This study had many strengths in that we used DXA to measure the children’s bone density as this is the gold standard of measuring bone density. We also used validated questionnaires to measure physical activity and screen time levels [17]. Another major strength of this study was the intentional recruitment of children within a very narrow age range (4.83–5.5 years old) which allowed us to investigate bone health at this time point without too much variation. One potential limitation is the sample size of 102 participants in this study. While it would have been interesting to investigate the impact of ethnicity on bone health, 99% of participants in this analysis were Caucasian, and further research is required in other ethnic groups. Another limitation is the use of a food frequency questionnaire to estimate micronutrient status, because a more detailed measure, such as a food diary, would be more appropriate and this should be considered for future research investigating associations with vitamin D and calcium. A final potential limitation to this study is that the information on the season that the blood samples were drawn was not noted and therefore any association made between 25OHD levels and BMD may be compromised.
Future research should be carried out in children of similar age, as the current volume of research on modifiable factors impacting bone health at this age is quite limited. Although there are a multitude of such studies conducted in preadolescents and older children, there is a dearth in studies in children in early childhood which is a vital time of growth and development.
We found that increased body size was associated with higher BMD. As this relationship was identified predominantly in the female cohort and was weaker when analysing males only, further research is warranted in this area in order to identify the potential differential effect of sex on BMD during childhood. We identified no association between self-reported lifestyle and dietary factors and bone health in early childhood as measured by BMD analysis using DXA. This suggests that in early childhood body weight may be an important indicator of child bone health. Thus, child body size could potentially be identified as a modifiable factor in interventions aiming to improve bone health, and monitoring body size throughout childhood may also be beneficial in terms of bone health. This is important for bone health in later life as optimising BMD during childhood can reduce the risk of fractures in adolescence and adult life. Identifying modifiable factors that can improve bone health at a young age is of utmost importance. Further research is required in this area to elucidate the exact mechanisms whereby body weight can influence bone health and to identify methods of ensuring children reach peak bone mass for optimal bone health later in life.
Abbreviations
- 25OHD:
-
25-hydroxyvitamin D
- BMC:
-
Bone mineral content
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- CLASS:
-
Children’s Leisure and Activities Study Survey
- DXA:
-
Dual-energy X-ray absorptiometry
- FFQ:
-
Food frequency questionnaire
- IQR:
-
Interquartile range
- MUA:
-
Mid-upper arm
- RDA:
-
Recommended daily allowance
- SD:
-
Standard deviation
References
Bachrach LK (2001) Acquisition of optimal bone mass in childhood and adolescence. Trends Endocrinol Metab 12:22–28. https://doi.org/10.1016/S1043-2760(00)00336-2
Bailey RL, Dodd KW, Goldman JA, Gahche JJ, Dwyer JT, Moshfegh AJ, Sempos CT, Picciano MF (2010) Estimation of total usual calcium and vitamin D intakes in the United States. J Nutr 140:817–822. https://doi.org/10.3945/jn.109.118539
Balk EM, Adam GP, Langberg VN, Earley A, Clark P, Ebeling PR, Mithal A, Rizzoli R, Zerbini CAF, Pierroz DD, Dawson-Hughes B (2017) Global dietary calcium intake among adults: a systematic review. Osteoporos Int. https://doi.org/10.1007/s00198-017-4230-x
Barlow SE, the Expert Committee (2007) Expert Committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 120(4):S 164–S 192. https://doi.org/10.1542/peds.2007-2329C
Bradney M, Pearce G, Naughton G, Sullivan C, Bass S, Beck T, Carlson J, Seeman E (1998) Moderate exercise during growth in prepubertal boys: changes in bone mass, size, volumetric density, and bone strength: a controlled prospective study. J Bone Miner Res 13:1814–1821. https://doi.org/10.1359/jbmr.1998.13.12.1814
Cashman KD, Dowling KG, Škrabáková Z, Gonzalez-Gross M, Valtueña J, De Henauw S, Moreno L, Damsgaard CT, Michaelsen KF, Mølgaard C, Jorde R, Grimnes G, Moschonis G, Mavrogianni C, Manios Y, Thamm M, Mensink GBM, Rabenberg M, Busch MA, Cox L, Meadows S, Goldberg G, Prentice A, Dekker JM, Nijpels G, Pilz S, Swart KM, Van Schoor NM, Lips P, Eiriksdottir G, Gudnason V, Cotch MF, Koskinen S, Lamberg-Allardt C, Durazo-Arvizu RA, Sempos CT, Kiely M (2016) Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr 103:1033–1044. https://doi.org/10.3945/ajcn.115.120873
Clark EM, Ness AR, Bishop NJ, Tobias JH (2006) Association between bone mass and fractures in children: a prospective cohort study. J Bone Miner Res 21:1489–1495. https://doi.org/10.1359/jbmr.060601
Clark EM, Ness AR, Tobias JH (2006) Adipose tissue stimulates bone growth in prepubertal children. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2006-0332
Council on Communications and Media (2016) Media use in school-aged children and adolescents. Pediatrics 138:e20162592. https://doi.org/10.1542/peds.2016-2592
Deng FY, Lei SF, Li MX, Jiang C, Dvornyk V, Deng HW (2006) Genetic determination and correlation of body mass index and bone mineral density at the spine and hip in Chinese Han ethnicity. Osteoporos Int 17:119–124. https://doi.org/10.1007/s00198-005-1930-4
Department of Health and Children (2009) Health Service Executive, The national guidelines on physical activity for Ireland. https://doi.org/10.1152/japplphysiol.00137.2005.
Dohc, Growing up in Ireland (2009) 58–59. http://www.growingup.ie/fileadmin/user_upload/documents/1st_Report/Barcode_Growing_Up_in_Ireland_-_The_Lives_of_9-Year-Olds_Main_Report.pdf
Food Safety Authority of Ireland (2011) Scientific recommendations for healthy eating guidelines in Ireland
Geraghty AA, Alberdi G, O’Sullivan EJ, O’Brien EC, Crosbie B, Twomey PJ, McAuliffe FM (2016) Maternal blood lipid profile during pregnancy and associations with child adiposity: findings from the ROLO study. PLoS One 11. https://doi.org/10.1371/journal.pone.0161206
Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL (2018) Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. 4–6. https://doi.org/10.1001/jama.2018.3060
Hind K, Burrows M (2007)Weight-bearing exercise and bone mineral accrual in children and adolescents: a review of controlled trials. Bone. https://doi.org/10.1016/j.bone.2006.07.006
Huang YJ, Wong SHS, Salmon J (2009) Reliability and validity of the modified Chinese version of the Children’s Leisure Activities Study Survey (CLASS) questionnaire in assessing physical activity among Hong Kong children. Pediatr Exerc Sci 21:339–353. https://doi.org/10.1123/pes.21.3.339
Janicka A, Wren TAL, Sanchez MM, Dorey F, Kim PS, Mittelman SD, Gilsanz V (2007) Fat mass is not beneficial to bone in adolescents and young adults. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2006-0794
Kerr DA, Papalia S, Morton A, Dick I, Dhaliwal S, Prince RL (2007) Bone mass in young women is dependent on lean body mass. J Clin Densitom 10:319–326. https://doi.org/10.1016/j.jocd.2007.05.001
Koedijk JB, van Rijswijk J, Oranje WA, van den Bergh JP, Bours SP, Savelberg HH, Schaper NC (2017) Sedentary behaviour and bone health in children, adolescents and young adults: a systematic review. Osteoporos Int 28:2507–2519. https://doi.org/10.1007/s00198-017-4076-2
Laine CM, Laine T (2013) Diagnosis of osteoporosis in children and adolescents. Eur Endocrinol 9:141–144
Lazcano-Ponce E, Tamayo J, Díaz R, Burguete AI, Salmerón J (2009) Correlation trends for bone mineral density in Mexican women: evidence of familiar predisposition. Salud Publica Mex. https://doi.org/10.1590/S0036-36342009000700012
Lee JCWT, Leung SS, Wang SH, Zeng WP, Lau J, Oppenheimer SJ (1994) Double-blind, controlled calcium supplementation and bone mineral accretion in children accustomed to a low-calcium diet. Am J Clin Nutr 60:1994
Leonard MB, Shults J, Wilson BA, Tershakovec AM, Zemel BS (2004) Obesity during childhood and adolescence augments bone mass and bone dimensions. Am J Clin Nutr 80:514–523 http://www.scopus.com/inward/record.url?eid=2-s2.0-4143073991&partnerID=40&md5=12e67ea74f3efe9a354295b52261dad6
Ma XM, Huang ZW, Yang XG, Su YX (2014) Calcium supplementation and bone mineral accretion in Chinese adolescents aged 12-14 years: a 12-month, dose-response, randomised intervention trial. Br J Nutr 112:1510–1520. https://doi.org/10.1017/S0007114514002384
Mackelvie KJ, Mckay HA, Petit MA, Moran O, Khan KM (2002) Bone mineral response to a 7-month randomized controlled, school-based jumping intervention in 121 prepubertal boys: associations with ethnicity and body mass index. J Bone Miner Res 17:834–844. https://doi.org/10.1359/jbmr.2002.17.5.834
MacKelvie KJ, Khan KM, Petit MA, Janssen PA, McKay HA (2003) A school-based exercise intervention elicits substantial bone health benefits: a 2-year randomized controlled trial in girls. Pediatrics. 112:e447–e452. https://doi.org/10.1542/peds.112.6.e447
Mazess RB, Barden HS, Bisek JP, Hanson J (1990)Dual-energy X-ray absorptiometry for total-body and regional bone-mineral and soft-tissue composition. Am J Clin Nutr 51:1106–1112
McVey MK, Geraghty AA, O’Brien EC, Kilbane MT, Crowley RK, Twomey PJ, McKenna MJ, McAuliffe FM (2019) An exploratory analysis of associations of diet, sun exposure, and body composition with 25OHD at five years of age: findings from the ROLO Kids Study. J Steroid Biochem Mol Biol. https://doi.org/10.1016/j.jsbmb.2018.12.014
Murphy S, Khaw K-T, May H, Compston JE (1994) PAPERS Milk consumption and bone mineral density in middle aged and elderly women. BMJ. 308:939–941
Nickols-Richardson SM, O’Connor PJ, Shapses SA, Lewis RD (1999) Longitudinal bone mineral density changes in female child artistic gymnasts. J Bone Miner Res. https://doi.org/10.1359/jbmr.1999.14.6.994
Nickols-Richardson SM, Modlesky CM, O’connor PJ, Lewis RD (2000) Premenarcheal gymnasts possess higher bone mineral density than controls. Med Sci Sports Exerc 32:63–69
Perry I, Millar S, Balanda K, Dee A, Bergin D, Carter L, Doherty E, Fahy L, Hamilton D, Jaccard A, Knuchel-Takano A, McCarthy L, McCune A, O’ Malley G, Pimpin L, Queally M, Webbe L (2017) What are the estimated costs of childhood overweight and obesity on the island of Ireland?
Pollock NK, Laing EM, Baile CA, Hamrick MW, Hall DB, Lewis RD (2007) Is adiposity advantageous for bone strength? A peripheral quantitative computed tomography study in late adolescent females 1–3. Am J Clin Nutr 86:1530–1538
Public Health England (2015) Composition of foods integrated dataset (CoFID)-GOV.UK
Runyan SM, Stadler DD, Bainbridge CN, Miller SC, Moyer-Mileur LJ (2003) Familial resemblance of bone mineralization, calcium intake, and physical activity in early-adolescent daughters, their mothers, and maternal grandmothers. J Am Diet Assoc. https://doi.org/10.1016/S0002-8223(03)01075-7
Specker B, Thiex NW, Sudhagoni RG (2015) Does exercise influence pediatric bone? A systematic review. Clin Orthop Relat Res. https://doi.org/10.1007/s11999-015-4467-7
Timpson NJ, Sayers A, Davey-Smith G, Tobias JH (2009) How does body fat influence bone mass in childhood? A mendelian randomization approach. J Bone Miner Res 24:522–533. https://doi.org/10.1359/jbmr.081109
Travison TG, Araujo AB, Esche GR, Beck TJ, McKinlay JB (2007) Lean mass and not fat mass is associated with male proximal femur strength. J Bone Miner Res 23:189–198. https://doi.org/10.1359/jbmr.071016
Walsh JM, McGowan CA, Mahony R, Foley ME, McAuliffe FM (2012) Low glycaemic index diet in pregnancy to prevent macrosomia (ROLO study): randomised control trial. BMJ. 345:e5605–e5605. https://doi.org/10.1136/bmj.e5605
Winzenberg TM, Powell S, Shaw KA, Jones G (2010) Vitamin D supplementation for improving bone mineral density in children. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD006944.pub2
Winzenberg T, Powell S, Shaw KA, Jones G (2011) Effects of vitamin D supplementation on bone density in healthy children: systematic review and meta-analysis. BMJ. 342:c7254. https://doi.org/10.1136/bmj.c7254
Winzenberg T, Lamberg-Allardt C, El-Hajj Fuleihan G, Mølgaard C, Zhu K, Wu F, Riley RD (2018) Does vitamin D supplementation improve bone density in vitamin D-deficient children? Protocol for an individual patient data meta-analysis. BMJ Open 8:e019584. https://doi.org/10.1136/bmjopen-2017-019584
Zanker CL, Gannon L, Cooke CB, Gee KL, Oldroyd B, Truscott JG (2003) Differences in bone density, body composition, physical activity, and diet between child gymnasts and untrained children 7-8 years of age. J Bone Miner Res 18:1043–1050. https://doi.org/10.1359/jbmr.2003.18.6.1043
Acknowledgements
The authors would like to thank parents and children who participated in the research. Recruitment of the ROLO Kids study participants and data collection was carried out by Dr. Aisling Geraghty and Dr. Eileen O’Brien. Laboratory analysis was carried out by St. Vincent’s University Hospital.
Funding
This study was supported by the Health Research Board Ireland, the Health Research Centre for Health and Diet Research, and the European Union's Seventh Framework Programme (FP7/2007-2013), project Early Nutrition under grant agreement no. 289346. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The ROLO and ROLO Kids studies were carried out in accordance with the Helsinki Declaration of 1975 as revised in 1983 with institutional ethical approval from the National Maternity Hospital in November 2006 for the original ROLO study and for the ROLO Kids 6 month and 2 year follow-up in May 2009. The Current Controlled Trials registration number for the ROLO study was ISRCTN54392969. The ROLO Kids 5-year follow-up and DXA scanning AddOn were approved by the Ethics (Medical Research) Committee in Our Lady’s Children’s Hospital, Dublin, REC reference: GEN/279/12.
Informed consent
Informed written maternal consent was obtained during pregnancy and at each subsequent follow-up.
Additional information
Communicated by Peter de Winter
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
McVey, M.K., Geraghty, A.A., O’Brien, E.C. et al. The impact of diet, body composition, and physical activity on child bone mineral density at five years of age—findings from the ROLO Kids Study. Eur J Pediatr 179, 121–131 (2020). https://doi.org/10.1007/s00431-019-03465-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03465-x