Abstract
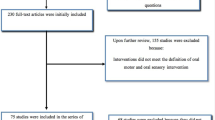
The NOMAS is by far the most used tool to screen early oral-motor skills in newborns. Here we provide an updated review of scientific literature on the use of the Neonatal Oral Motor Assessment Scale (NOMAS) to screen early oral-motor skills in newborns. An integrative review has been carried out consistent with PRISMA guidelines and standardized qualitative appraisal. Data abstracting and synthesis were executed by two independent co-authors who solved disagreement in conference. Twenty records have been included and reviewed. The efficacy of the NOMAS in screening and identifying precocious oral-motor skills received inconsistent support. Moderate validity and low reliability emerged. Moreover, despite the NOMAS’ adequately screen efficient and inefficient feeders, limited evidence emerged for predictive value of NOMAS score on feeding and psychomotor developmental trajectories during the first 2 years of age.
Conclusion: The present review highlights benefits and limitations of the NOMAS. Future research is needed to develop observational and clinically-relevant tools to better identify newborns which are at lower- and higher-risk of developing less-than-optimal feeding behaviors and to guide with greater precision the diagnostic and therapeutic journey of these newborns.
What is Known: • The assessment of oral-motor skills in newborns and infants is critical for early intervention • The NOMAS is the most adopted tool to assess oral-motor skills in newborns and infants |
What is New: • The ability of the NOMAS to target newborn at risk for feeding disorders is confirmed • Nonetheless, the capacity to predict long-term developmental outcomes is limited |

Similar content being viewed by others
Abbreviations
- BPD:
-
Bronchopulmonary dysplasia
- NOMAS:
-
Neonatal Oral Motor Assessment Scale
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- SGA:
-
small for gestational age
References
Jadcherla SR (2017) Advances with neonatal aerodigestive science in the pursuit of safe swallowing in infants: invited review. Dysphagia 32:15–26. https://doi.org/10.1007/s00455-016-9773-z
Miller CK (2009) Updates on pediatric feeding and swallowing problems. Curr Opin Otolaryngol Head Neck Surg 17:194–199. https://doi.org/10.1097/MOO.0b013e32832b3117
Manikam R, Perman JA (2000) Pediatric feeding disorders. J Clin Gastroenerol 30:34–46
Newman LA, Keckley C, Petersen MC (2001) Swallowing function and medical diagnoses in infants suspected of dysphagia. Pediatrics 108:E106
Schädler G, Süss-Burghart H, Toschke AM, von Voss H, von Kries R (1998) Feeding disorders in ex-prematures: causes-response to therapy-long term outcome. Eur J Pediatr 166:803–808. https://doi.org/10.1007/s00431-006-0322-x
Howe TH, Lin KC, Fu CP, Su CT, Hsieh CL (2008) A review of psychometric properties of feeding assessment tools used in neonates. JOGNN 37:338–349. https://doi.org/10.1111/j.1552-6909.2008.00240.x
Bickell M, Barton C, Dow K et al (2017) A systematic review of clinical and psychometric properties of infant oral motor feeding assessments. Dev Neurorehabil 8:1–11
Braun MA, Palmer MM (1985) A pilot study of oral-motor dysfunction in “at risk” infants. Phys Occup Ther Pediatr 5:13–26
Howe TH, Sheu CF, Hinojosa J et al (2007) Multiple factors related to bottle-feeding performance in preterm infants. Nurs Res 56:307–311. https://doi.org/10.1097/01.NNR.0000289498.99542.dd
Zarem C, Kidokoro H, Neil J, Wallendorf M, Inder T, Pineda R (2013) Psychometrics of the neonatal oral motor assessment scale. Dev Med Child Neurol 55:1115–1120. https://doi.org/10.1111/dmcn.12202
Palmer MM, Crawley K, Blanco IA (1993) Neonatal oral-motor assessment scale: a reliability study. J Perinatol 13:28–35
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ Open 339:b2700
Case Smith J, Cooper P, Scala V (1989) Feeding efficiency of premature neonates. Am J Occup Ther 43:245–250
Ferguson A, Blaymore Bier JA, Cucca J et al (1996) The quality of sucking in infants with colic. Infant Ment Health J 17:161–169
Palmer MM, Heyman MB (1999) Developmental outcome for neonates with dysfunctional and disorganized sucking patterns: preliminary findings. Infant-Toddler Interv 9:299–308
MacMullen NJ, Dulski LA (2000) Factors related to sucking ability in healthy newborns. JOGNN 29:390–396
Howe TH, Sheu CF, Hsieh YW et al (2007) Psychometric characteristics of the neonatal oral–motor assessment scale in healthy preterm infants. Dev Med Chi Neurol 2:915–919
Masarei AG, Sell D, Habel A, Mars M, Sommerlad BC, Wade A (2007) The nature of feeding in infants with unrepaired cleft lip and/or palate compared with healthy noncleft infants. Cleft Palate Craniofac J 44:321–328. https://doi.org/10.1597/05-185
da Costa SP, Van Der Schans CP (2008) The reliability of the neonatal oral-motor assessment scale. Acta Paed 97:21–26. https://doi.org/10.1111/j.1651-2227.2007.00577.x
da Costa SP, van der Schans CP, Zweens MJ, Boelema SR, van der Meij E, Boerman MA, Bos AF (2010) The development of sucking patterns in preterm, small-for-gestational age infants. J Pediatr 157:603–609. https://doi.org/10.1016/j.jpeds.2010.04.037
da Costa SP, Van Der Schans CP, Zweens MJ (2010) Development of sucking patterns in pre-term infants with bronchopulmonary dysplasia. Neonatology 98:268–277. https://doi.org/10.1159/000281106
da Costa SP, van der Schans CP, Boelema SR, van der Meij E, Boerman MA, Bos AF (2010) Sucking patterns in fullterm infants between birth and 10 weeks of age. Inf Behav Dev 33:61–67
Tsai SW, Chen CH, Lin MC (2010) Prediction for developmental delay on neonatal oral motor assessment scale in preterm infants without brain lesion. Pediatr Int 52:65–68
Bingham PM, Ashikaga T, Abbasi S (2012) Relationship of neonatal oral motor assessment scale to feeding performance of premature infants. J Neonat Nurs 18:30–36. https://doi.org/10.1016/j.jnn.2010.09.004
Nieuwenhuis T, da Costa SP, Bilderbeek E et al (2008) Uncoordinated sucking patterns in preterm infants are associated with abnormal general movements. J Pediatr 161:792–798
Törölä H, Lehtihalmes M, Yliherva A, Olsén P (2012) Feeding skill milestones of preterm infants born with extremely low birth weight (ELBW). Infant Beh Dev 35:187–194. https://doi.org/10.1016/j.infbeh.2012.01.005
Wolthuis-Stigter MI, Luinge MR, Da Costa SP et al (2015) The association between sucking behavior in preterm infants and neurodevelopmental outcomes at 2 years of age. J Pediatr 166:26–30
da Costa SP, Hübl N, Kaufman N et al (2016) New scoring system improves inter-rater reliability of the neonatal oral-motor assessment scale. Acta Paed 105:e339–e344. https://doi.org/10.1111/apa.13461
Jackson N, Waters E (2015) Criteria for the systematic review of health promotion and public health interventions. Health Promot Int 20:367–374. https://doi.org/10.1093/heapro/dai022
Acknowledgements
We are grateful to the colleagues of the Neuropsychiatry and Neuro-rehabilitation Unit and of the 0-3 Center for the at-Risk Infant for their daily support in clinical and research activities.
Author information
Authors and Affiliations
Contributions
Author LL performed literature search, Author AC and author DS provided clinical supervision, LP wrote the first manuscript draft, GSDM provided thorough revision of the final draft, and RB conceived the study. All authors approved the final manuscript for submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Informed consent
Not applicable.
Additional information
Communicated by Mario Bianchetti
Rights and permissions
About this article
Cite this article
Longoni, L., Provenzi, L., Cavallini, A. et al. Predictors and outcomes of the Neonatal Oral Motor Assessment Scale (NOMAS) performance: a systematic review. Eur J Pediatr 177, 665–673 (2018). https://doi.org/10.1007/s00431-018-3130-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3130-1