Abstract
Neurally adjusted ventilatory assist (NAVA) improves patient-ventilator synchrony during invasive ventilation and leads to lower peak inspiratory pressures (PIP) and oxygen requirements. The aim of this trial was to compare NAVA with current standard ventilation in preterm infants in terms of the duration of invasive ventilation. Sixty infants born between 28 + 0 and 36 + 6 weeks of gestation and requiring invasive ventilation due to neonatal respiratory distress syndrome (RDS) were randomized to conventional ventilation or NAVA. The median durations of invasive ventilation were 34.7 h (quartiles 22.8–67.9 h) and 25.8 h (15.6–52.1 h) in the NAVA and control groups, respectively (P = 0.21). Lower PIPs were achieved with NAVA (P = 0.02), and the rapid reduction in PIP after changing the ventilation mode to NAVA made following the predetermined extubation criteria challenging. The other ventilatory and vital parameters did not differ between the groups. Frequent apneas and persistent pulmonary hypertension were conditions that limited the use of NAVA in 17 % of the patients randomized to the NAVA group. Similar cumulative doses of opiates were used in both groups (P = 0.71).
Conclusions: NAVA was a safe and feasible ventilation mode for the majority of preterm infants suffering from RDS, but the traditional extubation criteria were not clinically applicable during NAVA.
What is known: • NAVA improves patient-ventilator synchrony during invasive ventilation. • Lower airway pressures and oxygen requirements are achieved with NAVA during invasive ventilation in preterm infants by comparison with conventional ventilation. |
What is new: • Infants suffering from PPHN did not tolerate NAVA in the acute phase of their illness. • The traditional extubation criteria relying on inspiratory pressures and spontaneous breathing efforts were not clinically applicable during NAVA. |
Similar content being viewed by others
Introduction
Respiratory distress syndrome (RDS), caused by lung immaturity and surfactant deficiency, is the leading cause of neonatal morbidity in preterm infants. Despite an increasing desire to use non-invasive ventilatory support, RDS still remains the main reason for invasive ventilation in neonates [12, 15, 19, 28]. Although mechanical ventilation is often life-saving, it carries the risk of causing additional lung injury and plays a role in the progression of bronchopulmonary dysplasia (BPD) in markedly preterm infants [13].
The risk of ventilator-induced lung injury may be reduced by using small tidal volumes, ensuring an adequate level of positive end-expiratory pressure (PEEP) and synchronizing the support with the patient’s spontaneous breaths [5, 22, 27]. Small tidal volumes, high breathing frequency, and the use of uncuffed intubation tubes causing an air leak from the circuit pose challenges for optimizing ventilation in a neonatal population. Consequently, pneumatic triggers are suboptimal in this group of patients [5]. Neurally adjusted ventilatory assist (NAVA) provides ventilatory support proportional to the electrical activity of the patient’s diaphragm (Edi) and enables physiological variations in both tidal volume and inspiratory time [23]. NAVA has been shown to reduce the work of breathing and improve patient-ventilator synchrony in neonates, resulting in lower peak inspiratory pressures (PIP) and oxygen requirements than with conventional ventilation [2, 16, 24, 25]. NAVA is increasingly being used in neonatal intensive care units, but data concerning its impact on clinical outcomes in preterm population are sparse [1].
The aim of this trial was to compare NAVA with the current standard ventilation in preterm infants born between 28 + 0 and 36 + 6 weeks of gestation and requiring invasive ventilation due to RDS. We hypothesized that the use of NAVA ventilation would reduce the duration of mechanical ventilation.
Materials and methods
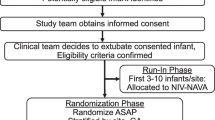
All preterm infants born at Oulu University Hospital between 28 + 0 and 36 + 6 weeks of gestation, who required invasive ventilation for at least 4 h due to RDS, were eligible for this trial. Neonates with a known defect of the diaphragm and those who were unable to receive a nasogastric or orogastric tube due to congenital anomalies were excluded, as were patients suffering from severe perinatal asphyxia (pH <7.0 or signs of hypoxic-ischemic encephalopathy) or known chromosomal abnormalities. Written informed consent was obtained from a parent or legal guardian before performing any procedures related to this trial. The patients were enrolled at the neonatal (NICU) and pediatric intensive care units (PICU) of Oulu University Hospital, Finland, from July 2010 to May 2013. The ClinicalTrials.gov. Identifier for this study is NCT01156467.
The sample size was calculated based on the Finnish National Institute for Health and Welfare database information concerning the duration of invasive ventilation among preterm infants. The mean duration of invasive ventilation among infants born at 32 + 0 weeks during the years 2005 and 2006 was 38.4 h, with a standard deviation (SD) of 15.6 h. We considered a reduction of 12 h clinically significant. With α = 0.05 and a power of 0.8, the calculated sample size was 54 (27 patients/group). To ensure this number in the final analysis, 60 patients were recruited. A stratified randomization was used to evenly allocate neonates below and above 32 weeks of gestation to the NAVA and control groups for invasive ventilation. A computerized random number generator was used for randomization and each group code was sealed in an opaque envelope that was opened after written informed consent had been received. The protocol was approved by the Research Ethics Committee of the Northern Ostrobothnia Health Care District.
Detailed patient characteristics are shown in Table 1. All the patients were invasively ventilated using a Servo-i ventilator, versions 4.0 to 6.1 (Maquet Nordic, Solna, Sweden). An Edi catheter was inserted for the patients randomized to the NAVA group as soon as the procedures required on arrival (intravenous and intra-arterial lines, thorax x-ray, surfactant treatment if not given in the delivery room) had been performed and a stable clinical condition had been achieved so that changing a nasogastric tube was not expected to cause significant deterioration in hemodynamics or oxygenation. Adequate size of the Edi catheter (6 Fr 49 cm, 6 Fr 50 cm or 8 Fr 100 cm) was chosen in accordance with patient weight and the correct position was checked as instructed by the manufacturer. The ventilation mode was changed to NAVA when a continuous Edi signal was obtained and the patient was hemodynamically stable. The NAVA level was estimated to reach the same peak inspiratory pressure (PIP) as in the previous ventilation mode and was adjusted during NAVA ventilation to aim at a peak Edi between 5 and 15 μVs. The control group received patient-triggered time-cycled pressure-limited ventilation (PC) following the current treatment practices in the NICU, aiming at small tidal volumes (4–6 ml/kg) and support for spontaneous breaths by optimizing the preset frequency to allow patient triggering. The patients who required high-frequency oscillatory ventilation (HFOV) were ventilated according to the protocol for this trial only in the weaning phase of the treatment. It was the clinician responsible for the treatment who made the final decision regarding the ventilation mode to be used in each situation. The extubation criteria, determined following the current clinical practice in the unit, were as follows: (1) fraction of inspired oxygen less than 0.4; (2) PIP ≤ 16 cmH2O; and (3) an adequate spontaneous breathing drive, i.e., sufficient frequency and tidal volumes despite reduction in the level of support. Non-invasive respiratory support was used after extubation when relevant, i.e., nasal continuous positive airway pressure or bilevel positive airway pressure for the patients in the control group and non-invasive NAVA (NIV NAVA) for the patients in the NAVA group.
Analgesics and sedative agents were administered to both groups following the routine practice in the NICU. Intravenous paracetamol with a 20 mg/kg loading dose followed by 7.5 mg/kg every 6 h was used as the primary analgesic agent [9]. The need for opiates and sedative agents were assessed on a clinical basis together with use of the Neonatal Infant Acute Pain Assessment Scale (NIAPAS), which was under validation and had been introduced for routine use in our intensive care units at time of the trial [21].
The primary end point was the duration of invasive ventilation, while the secondary end points were the length of stay in the NICU, the amount of sedative agent, ventilatory parameters (oxygenation index [OI], tidal volume [TV], airway pressures and breathing frequency), vital parameters (heart rate, blood pressure and oxygen saturation), arterial blood gas (ABG) values, treatment complications (pneumonia, atelectasis, air leak, and reintubation within 24 h), clinical outcome measures, the duration of non-invasive respiratory support, and success in enteral feeding. Data collection was started as soon as written informed consent had been obtained from a parent or legal guardian and the patient’s condition allowed insertion of the Edi catheter. The parameters were recorded at the start, after 30 min (all except ABG analysis), 1 h, 3 h, and 6 h, every 6 h thereafter until extubation, and 1 h after extubation. The amount of sedative agent and surfactant doses were recorded from the Centricity Critical Care Clinisoft monitoring database and a special data collection sheet was used for the other parameters. Ventilator parameters were collected directly from the ventilator screen and from the trend curves (averaged over 1 min) in cases of high variability from breath to breath (PIP, Edi min and max).
The severity of RDS was graded from thorax x-rays taken prior to inclusion in the trial, following the criteria described by Edwards et al. [7], and all the x-rays and head ultrasound scans taken during the trial were analyzed for treatment complications. The pediatric radiologist assessing these findings (MS-P) was blind with respect to the two groups. An oxygen reduction test was performed on all the infants requiring supplemental oxygen at 36 weeks of post-conceptional age in order to diagnose possible bronchopulmonary dysplasia (BPD) [30].
The data were analyzed on an intention-to-treat basis. Kaplan-Meier survival curves were plotted for the time on the ventilator and the length of stay in the NICU, and the log-rank test was used to evaluate distributions between the groups. A linear mixed model (LMM) with random intercept and a first-order autoregressive (AR1) covariance structure for repeated measurements was used to evaluate the ventilatory and vital parameter levels over time between the NAVA and control groups [4]. Repeated measurements were nested within subjects. Group-by-time interaction was used to test differences between the groups at each point in time. The differences between proportions were tested using the binomial Standardized Normal Deviate (SND) test for two groups and a chi-square test for more than two groups. Differences between means were compared using Student’s t test. The data analyses were performed with IBM SPSS Statistics version 22 and StatsDirect statistical software version 2.7.9.
Results
The median duration of invasive ventilation was 34.7 h (quartiles 22.8–67.9 h) in the NAVA group and 25.8 h (15.6–52.1 h) in the control group, P = 0.21. The median length of stay in the NICU was 18 (9–36) days and 13 (8–31) days in the NAVA and control groups, respectively (P = 0.36). Treatment times were similar in the two groups even after splitting the data according to gestation weeks (Fig. 1). The Edi catheter was easy to insert in all 29 neonates randomized into the NAVA group. NAVA could be started immediately after insertion of the Edi catheter in 24 cases (83 %), and 21 of these (72 %) were successfully ventilated with NAVA until extubation, without any periods of conventional ventilation after starting NAVA. The time on NAVA varied from 0.2 to 108 h, accounting for 79 ± 33 % of the invasive ventilation provided after inclusion in the trial and 60 ± 26 % of the total duration of invasive ventilation. Ventilation modes and NAVA parameters (Edi min, Edi max, and NAVA level) for the NAVA patients at each data collection point are presented in Fig. 2.
Durations of invasive ventilation and length of stay in the NICU. a The median durations of invasive ventilation for infants born between 28 + 0 and 31 + 6 weeks of gestation were 52.5 and 26.9 h in the NAVA and control groups, respectively (log rank P = 0.31), and those for infants born between 32 + 0 and 36 + 6 weeks 34.7 h in the NAVA group and 23.3 h in the controls (P = 0.35). b The length of stay in the NICU is more dependent on other prematurity-related conditions than on the requirement for invasive ventilation, as seen from the Kaplan-Meier curves plotted separately for infants born before and after 32 weeks of gestation. The length of stay did not differ between the NAVA and control groups (log rank P = 0.18 for infants <32 weeks and 0.45 for infants ≥32 weeks of gestation)
Frequent apnea was the most common reason for NAVA proving unsuccessful immediately after insertion of the Edi-catheter (n = 3) or switching back to the conventional ventilation mode after starting NAVA (n = 2). Low Edi activity, even during hypercapnic episodes, was observed in one patient who later was diagnosed with a mitochondrial disease. Three patients in the NAVA group required HFOV after inclusion in the trial but were successfully ventilated with NAVA after recovery from PPHN.
The patients in the NAVA group had lower PIPs than those in the control group (P = 0.02), but none of the other ventilatory parameters (PEEP, mean airway pressure [MAP], TV, breathing frequency or OI) differed between the groups (Fig. 3). The first PIP recorded during NAVA was below the predetermined extubation pressure, i.e., 16 cmH2O, in 20 patients (69 %), ranging from 7 to 22 cmH2O (mean 13.7 cmH2O). Four patients in the control group (13 %) were extubated at PIP levels higher than 16 cmH2O. The ABGs and vital parameters were similar in both groups.
Ventilatory parameters in the NAVA and control groups during the trial. Lower peak inspiratory pressures (a) were found in the NAVA group (P = 0.02). Breathing frequency (b), tidal volume (c) and oxygenation index (d) did not differ between the groups (P = 0.08, 0.33, and 0.58, respectively). The numbers of patients in the groups at each time point are shown in panel (b) (control/NAVA). Estimated marginal means with standard errors are presented at each point in time
Paracetamol, administered intravenously in 97 % of cases, was used as the primary analgesic agent for all the patients. Opiates were used for analgesia and sedation in 34 patients altogether (57 %), and after commencement of the trial, in 15 (52 %) of the NAVA patients and 13 (42 %) of those in the control group (P = 0.45). The amount of opiates did not differ between the groups (Table 2). Other sedatives (phenobarbital, midazolam or lorazepam) were administered to 4 patients in the NAVA group and 3 in the control group (P = 0.47).
The number of treatment complications did not differ between the groups (Table 3). There were no deaths in either group. Two patients in each group suffered late-onset sepsis during their stay in the NICU, and 4 altogether were diagnosed with BPD at 36 weeks of gestation, three of whom were in the NAVA group. The mean duration of non-invasive respiratory support after extubation was 2.3 (sd 1.9) days for the NAVA patients and 2.0 (1.6) days in the control group (P = 0.54). One of the control patients was treated with NIV NAVA after an accidental extubation, thereby avoiding reintubation. Reintubation was required once due to pneumothorax drainage in a patient in the NAVA group 24.5 h after extubation. Enteral nutrition, 100 ml/kg, was achieved at 6.1 (3.5) days in the NAVA group and 5.7 (3.2) days in the control group (P = 0.65).
Discussion
We found NAVA to be a safe and feasible ventilation mode for the majority of preterm infants born between 28 + 0 and 36 + 6 weeks of gestation and suffering from RDS. The Edi catheters were easy to insert and an active Edi signal was found immediately in virtually all the patients. Most of the patients were successfully ventilated with NAVA soon after insertion of the Edi catheter, and this continued until the moment of extubation. Lower peak inspiratory pressures were achieved with NAVA, but it did not reduce the duration of invasive ventilation or the length of our patients’ stay in the NICU.
NAVA has been shown to improve patient-ventilator synchrony and to lead to lower airway pressures in all patient groups, including preterm infants [2, 16, 20, 24, 25, 29]. The patient is in control of both inspiratory time and tidal volume during NAVA, while a fixed inspiratory time during PC inevitably leads to some extent of asynchrony on a spontaneously breathing individual. Our results are in line with previous findings, as the patients in the NAVA group had equal tidal volumes but lower airway pressures than those in the control group. We believe that reduction in PIP during NAVA is a result of improved synchrony, i.e., perfect timing of positive inspiratory pressure generated by the ventilator to negative pleural pressure created by patient effort, leading to adequate transpulmonary pressure even with low PIP. This might explain why two thirds of our NAVA patients fulfilled the predetermined extubation criteria at the first data collection after switching to this ventilation mode, even though the clinical and radiological findings on enrolment for the trial led us to expect that these patients would require several hours of invasive ventilation and possibly additional doses of surfactant.
Patient comfort, together with low airway pressures during NAVA, was probably the reason why extubations were so easily delayed in the NAVA group. The extubation criteria were not strictly followed by the clinicians on call during the night shift, and it seems that the tiny patients were not disturbed when peacefully asleep, even though they fulfilled the criteria. On the other hand, some control group patients were extubated, mainly due to hyperventilation, prior to fulfilling the predetermined criteria. Obviously, hyperventilation never becomes a problem with NAVA, and it seems that extubation criteria based solely on airway pressures and spontaneous breathing efforts are not clinically applicable during NAVA. More research and further experience with NAVA would be required to establish adequate criteria for future trials and clinical use.
For a certain proportion of the NAVA patients (17 %), NAVA could only be used after several hours or days of conventional ventilation or HFOV. Apnea of prematurity limited its use in the early stages of the trial, since the shortest possible apnea time in the first NAVA software version was 5 s. Shorter apnea time limit (2 s), which readily responds to patients’ demands, is now available and should be used for very preterm infants in risk of having prolonged apneic events. Three patients had PPHN associated with severe RDS and attempts to use NAVA in two of these cases led to deterioration in oxygenation and hemodynamics. The Hering-Breuer deflation reflex might be expected to help in optimizing lung volume and to improve oxygenation during NAVA, but in these cases, it seemed that strong spontaneous breathing efforts exacerbated pulmonary hypertension and NAVA could safely be used only in the weaning phase of treatment [3, 8, 10, 23].
Our population consisted of invasively ventilated preterm infants, 50 % of whom required at least two doses of surfactant. Patient selection led to a 7 % incidence of BPD, despite the fact that infants born at less than 28 weeks of gestation were not included. A major advantage of NAVA by comparison with conventional modes is the more gentle ventilation, with lower airway pressures and better patient-ventilator synchrony, which leads to a reduced need for supplemental oxygen and should be beneficial in preventing BPD [13, 24–26]. Three out of four of our patients later diagnosed with BPD were in the NAVA group, but they had several risk factors other than the ventilation mode, principally bacterial infections, severe RDS, long overall duration of invasive ventilation, and in one case an underlying mitochondrial disease [11]. It is obvious that our population was too small to allow us to detect any possible impact of the ventilation mode on long-term pulmonary complications.
Possible harmful effects of opiates and sedatives on neurodevelopment in preterm infants have directed current treatment strategies to avoid routine administration of these drugs in a NICU [6, 14, 18]. Paracetamol was the main analgesic agent used in our series, and opiates were resorted to when paracetamol together with non-pharmacological treatment were unable to provide adequate pain relief and patient comfort [9]. This led to equally low overall doses of opiates in both groups. A recent report comparing NAVA with pressure-regulated volume-controlled ventilation (PRVC) for preterm infants in two non-randomized 12-h periods reported decreased use of fentanyl during NAVA [17]. Improved patient comfort, together with the desire to maintain regular spontaneous breathing, is undoubtedly a feature of NAVA that favors a reduction in opiate use [20], but if larger doses of opiates are required only in the most severely ill, who cannot tolerate spontaneous breathing or NAVA in the acute phase of their illness, the lack of any difference is easily understood.
There are some limitations inherent in our protocol. First, we started enrolment soon after NAVA was available in our unit, which may have led to situations where the clinicians who made the final decision were not equally familiar with the two ventilation modes. This may have hindered the emergence of some differences between the groups. However, when including vulnerable preterm infants in a clinical trial such as this, it is essential that patient safety should come first, and that the clinician responsible for the treatment should make all the decisions. Secondly, the randomization led to some heterogeneity in patient characteristics between the groups, although the differences were not statistically significant. Thirdly, the extubation criteria written into the protocol were not strictly followed, so that our results concerning the duration of ventilation should be interpreted with caution. Finally, the fact that the shortest apnea time in the first NAVA software was 5 s highlights the challenge that apnea of prematurity presented for NAVA at the early stages in the trial.
In conclusion, we found NAVA to be a safe and feasible ventilation mode for the majority of preterm infants suffering from RDS. The traditional extubation criteria relying on inspiratory pressures and spontaneous breathing efforts were not clinically applicable during NAVA, so it did not reduce the duration of invasive ventilation. Larger randomized controlled trials on NAVA in neonatal intensive care are clearly needed, but comprehensive clinical experience with NAVA along with clinically applicable extubation criteria are prerequisites for the reliable performance of future trials.
Abbreviations
- ABG:
-
Arterial blood gas
- BPD:
-
Bronchopulmonary dysplasia
- Edi:
-
Electrical activity of the diaphragm
- GA:
-
Gestational age
- HFOV:
-
High-frequency oscillatory ventilation
- IUGR:
-
Intrauterine growth retardation
- LMM:
-
Linear mixed model
- MAP:
-
Mean airway pressure
- MED:
-
Morphine equivalent dose
- NAVA:
-
Neurally adjusted ventilatory assist
- NICU:
-
Neonatal intensive care unit
- NIV:
-
Non-invasive ventilation
- OI:
-
Oxygenation index
- PC:
-
Pressure-controlled ventilation
- PEEP:
-
Positive end-expiratory pressure
- PIP:
-
Peak inspiratory pressure
- PPHN:
-
Persistent pulmonary hypertension of the newborn
- RDS:
-
Respiratory distress syndrome
- TV:
-
Tidal volume
References
Alander M, Peltoniemi O, Saarela T, Anttila E, Pokka T, Kontiokari T (2013) Current trends in paediatric and neonatal ventilatory care—a nationwide survey. Acta Paediatr 102:123–128
Alander M, Peltoniemi O, Pokka T, Kontiokari T (2012) Comparison of pressure-, flow-, and NAVA-triggering in pediatric and neonatal ventilatory care. Pediatr Pulmonol 47:76–83
Bendapudi P, Rao GG, Greenough A (2015) Diagnosis and management of persistent pulmonary hypertension of the newborn. Paediatr Respir Rev 16:157–161
Brown H, Prescott R (2006) Applied mixed models in medicine. John Wiley & Sons Ltd, Chichester England
Brown MK, DiBlasi RM (2011) Mechanical ventilation of the premature neonate. Respir Care 56:1298–1311 discussion 1311-3
COMMITTEE ON FETUS AND NEWBORN and SECTION ON ANESTHESIOLOGY AND PAIN MEDICINE (2016) Prevention and management of procedural pain in the neonate: an update. Pediatrics 137:1–13
Edwards DK, Hilton SV, Merritt TA, Hallman M, Mannino F, Boynton BR (1985) Respiratory distress syndrome treated with human surfactant: radiographic findings. Radiology 157:329–334
Hannam S, Ingram DM, Rabe-Hesketh S, Milner AD (2001) Characterisation of the Hering-Breuer deflation reflex in the human neonate. Respir Physiol 124:51–64
Harma A, Aikio O, Hallman M, Saarela T (2016) Intravenous paracetamol decreases requirements of morphine in very preterm infants. J Pediatr 168:36–40
Jain A, McNamara PJ (2015) Persistent pulmonary hypertension of the newborn: advances in diagnosis and treatment. Semin Fetal Neonatal Med 20:262–271
Jensen EA, Schmidt B (2014) Epidemiology of bronchopulmonary dysplasia. Birth Defects Res A Clin Mol Teratol 100:145–157
Jobe AH, Bancalari E (2001) Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163:1723–1729
Kinsella JP, Greenough A, Abman SH (2006) Bronchopulmonary dysplasia. Lancet 367:1421–1431
Kocek M, Wilcox R, Crank C, Patra K (2016) Evaluation of the relationship between opioid exposure in extremely low birth weight infants in the neonatal intensive care unit and neurodevelopmental outcome at 2 years. Early Hum Dev 92:29–32
Koivisto M, Marttila R, Kurkinen-Raty M, Saarela T, Pokela ML, Jouppila P, Hallman M (2004) Changing incidence and outcome of infants with respiratory distress syndrome in the 1990s: a population-based survey. Acta Paediatr 93:177–184
Lee J, Kim HS, Sohn JA, Lee JA, Choi CW, Kim EK, Kim BI, Choi JH (2012) Randomized crossover study of neurally adjusted ventilatory assist in preterm infants. J Pediatr 161:808–813
Longhini F, Ferrero F, De Luca D, Cosi G, Alemani M, Colombo D, Cammarota G, Berni P, Conti G, Bona G, Della Corte F, Navalesi P (2015) Neurally adjusted ventilatory assist in preterm neonates with acute respiratory failure. Neonatology 107:60–67
McPherson C, Grunau RE (2014) Neonatal pain control and neurologic effects of anesthetics and sedatives in preterm infants. Clin Perinatol 41:209–227
Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB, Trial Investigators COIN (2008) Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med 358:700–708
Pdl O, Schuffelmann C, Gomez-Zamora A, Villar J, Kacmarek RM (2012) Asynchrony, neural drive, ventilatory variability and COMFORT: NAVA versus pressure support in pediatric patients. A non-randomized cross-over trial. Intensive Care Med 38:838–846
Polkki T, Korhonen A, Axelin A, Saarela T, Laukkala H (2014) Development and preliminary validation of the neonatal infant acute pain assessment scale (NIAPAS). Int J Nurs Stud 51:1585–1594
Putensen C, Muders T, Varelmann D, Wrigge H (2006) The impact of spontaneous breathing during mechanical ventilation. Curr Opin Crit Care 12:13–18
Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindstrom L (1999) Neural control of mechanical ventilation in respiratory failure. Nat Med 5:1433–1436
Stein H, Alosh H, Ethington P, White DB (2013) Prospective crossover comparison between NAVA and pressure control ventilation in premature neonates less than 1500 grams. J Perinatol 33:452–456
Stein H, Howard D (2012) Neurally adjusted ventilatory assist in neonates weighing <1500 grams: a retrospective analysis. J Pediatr 160:786–9.e1
Strueby L, Thebaud B (2014) Advances in bronchopulmonary dysplasia. Expert Rev Respir Med 8:327–338
van Kaam A (2011) Lung-protective ventilation in neonatology. Neonatology 99:338–341
van Kaam AH, Rimensberger PC, Borensztajn D, De Jaegere AP, Neovent Study Group (2010) Ventilation practices in the neonatal intensive care unit: a cross-sectional study. J Pediatr 157:767–71.e1-3
Vignaux L, Grazioli S, Piquilloud L, Bochaton N, Karam O, Jaecklin T, Levy-Jamet Y, Tourneux P, Jolliet P, Rimensberger PC (2013) Optimizing patient-ventilator synchrony during invasive ventilator assist in children and infants remains a difficult task*. Pediatr Crit Care Med 14:e316–e325
Walsh MC, Wilson-Costello D, Zadell A, Newman N, Fanaroff A (2003) Safety, reliability, and validity of a physiologic definition of bronchopulmonary dysplasia. J Perinatol 23:451–456
Acknowledgments
We thank the Alma and K.A. Snellman Foundation, Oulu, Finland, for financial support granted to Dr. Kallio, and the Foundation for Pediatric Research, Finland, for project support. We also thank the staff of the Neonatal Intensive Care Unit at Oulu University Hospital for their assistance during the recruitment phase and with collecting the data.
Author contributions
Dr. Kallio participated in protocol development and had the primary responsibility for patient screening, enrolment, outcome data, primary data analysis, and interpretation. She wrote the first version of the manuscript.
Dr. Koskela: patient screening, enrolment, primary data analysis, and writing the manuscript.
Dr. Peltoniemi: study design, patient enrolment, data interpretation, and writing the manuscript.
Dr. Kontiokari: study design, data interpretation, and writing the manuscript.
T. Pokka: statistical analysis, data interpretation, and writing the manuscript.
Dr. Suo-Palosaari assessed the radiological findings and participated in data interpretation and writing the manuscript.
Dr. Saarela: study design, patient enrolment, data interpretation and writing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was funded by the Alma and K.A. Snellman Foundation, Oulu, Finland, and the Foundation for Pediatric Research, Finland.
Ethical approval
All procedures performed in this trial were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from a parent or legal guardian for every individual participant included in the trial.
Conflict of interest
Dr. Kallio has participated as a speaker in scientific meetings and symposia organized and financed by Maquet Critical Care. The other authors declare that they have no conflict of interest.
Additional information
Communicated by Patrick Van Reempts
Revisions received: 22 May 2016; 12 July 2016
Rights and permissions
About this article
Cite this article
Kallio, M., Koskela, U., Peltoniemi, O. et al. Neurally adjusted ventilatory assist (NAVA) in preterm newborn infants with respiratory distress syndrome—a randomized controlled trial. Eur J Pediatr 175, 1175–1183 (2016). https://doi.org/10.1007/s00431-016-2758-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-016-2758-y