Abstract
During proportional assist ventilation (PAV), the applied pressure is servo-controlled based on continuous input from the infant’s breathing. In addition, elastic and resistive unloading can be employed to compensate for the abnormalities in the infant’s lung mechanics. The aim of this study was to test the hypothesis that in very prematurely born infants remaining ventilated beyond the first week, PAV compared to assist control ventilation (ACV) would be associated with superior oxygenation. A randomised crossover study was undertaken. Infants were studied for 4 hours each on PAV and ACV in random order; at the end of each 4-h period, the oxygenation index (OI) was calculated. Eight infants, median gestational age of 25 (range 24–33) weeks, were studied at a median of 19 (range 10–105) days. It had been intended to study 18 infants but as all the infants had superior oxygenation on PAV (p = 0.0039), the study was terminated after recruitment of eight infants. The median inspired oxygen concentration (p = 0.049), mean airway pressure (p = 0.012) and OI (p = 0.012) were all lower on PAV.
Conclusion: These results suggest that PAV compared to ACV is advantageous in improving oxygenation for prematurely born infants with evolving or established BPD.
What is known: •During proportional assist ventilation (PAV), the applied pressure is servo controlled throughout each spontaneous breath. •Elastic and resistive unloading can compensate for the infant’s abnormalities in lung mechanics. |
What is new: •In a randomised crossover study, infants with evolving/established BPD were studied on PAV and ACV each for 4 h. •The oxygenation index was significantly lower on PAV in all infants studied. |
Similar content being viewed by others
Introduction
During proportional assist ventilation (PAV), the applied pressure is servo controlled, based on continuous input from the infant’s breathing throughout each spontaneous breath. In addition, the ventilator can provide inflation pressure in phase with the tidal volume change in order to reduce the compliance load (i.e. the load due to the stiffness of infant’s lungs) and in phase with the flow change to reduce the resistance load (i.e. the load due to airflow obstruction), termed elastic and resistive unloading, respectively [6]. Very prematurely born infants developing or with established bronchopulmonary dysplasia (BPD) will have stiff lungs (that is non-compliant) despite a very compliant chest wall, so may be particularly likely to benefit from elastic unloading. PAV has only been assessed in neonates in a few studies. In a previous crossover study, we demonstrated that infants with evolving or established bronchopulmonary dysplasia (BPD) on PAV compared to assist control ventilation (ACV) had better oxygenation indices, a lower work of breathing and better respiratory muscle strength. The infants, however, were only studied on each ventilator mode for 1 h [1]. The longest infants have been studied on PAV is 4 h [7], but during that study, only changes in pulse oximetry results were assessed. During PAV, the applied pressure is servo controlled throughout each breath, whereas during ACV, only the initiation of inflation is sycnchronised to the start of inspiration; hence, we hypothesised that oxygenation would be superior on PAV compared to ACV. During PAV, however, we have demonstrated a trigger delay of 60 ms using an in vitro model [4]; hence, it was important to assess blood gases over a longer period that studied previously [1]. The aim of this study, therefore, was to test the hypothesis that infants with evolving or established BPD would have superior oxygenation index results after 4 h on PAV compared to after a similar period on ACV.
Methods
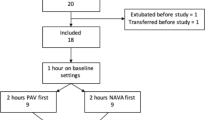
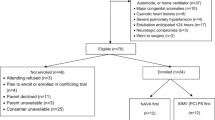
A randomised, crossover study was undertaken. Prematurely born infants remaining ventilated after the first week after birth were eligible for entry into the study if they were being supported by ACV. Evolving BPD was defined as ventilator dependence beyond 14 days and established BPD as ventilator dependence beyond 28 days. Infants were ineligible for inclusion in the study if they had a major congenital cardiac abnormality or were receiving a neuromuscular blockade agent. Infants were entered into the study if their parents gave informed written consent. The study was approved by the South East London Research Ethics Committee and King’s College Hospital Research Ethics Committee. During the 8-h study period, no other changes were made to the infant care than the changes in ventilator mode.
Infants at King’s College Hospital NHS Foundation Trust are routinely supported by the SLE 5000. The infants were transferred from the SLE 5000 ventilator to ACV on the Stephanie ventilator using the same ventilator settings (baseline). All infants as per the unit’s routine policy were ventilated via shouldered endotracheal tubes which have been shown to have minimal or no leaks [2]. One hour was allowed for stabilisation of the infant on the Stephanie ventilator. A blood gas analysis was then performed and the baseline ventilator settings were noted. During the stabilisation period, the ventilator displayed compliance and resistance settings were noted every 10 min and the six results meaned. The ventilator calculated the compliance from the inflation pressure (PIP-PEEP) and the resultant tidal volume. The value of the reciprocal of the compliance, elastance, was used to set the level of the elastic unloading. Each infant was then randomised to receive first either PAV or ACV mode for 4 h and for the second 4 h received the alternative mode. During ACV, the peak inspiratory pressure (PIP), positive end expiratory pressure (PEEP) and the inflation time were kept the same as at baseline. During PAV, the maximum PIP was set at 5 cm H2O above the PIP on ACV. The PEEP level during PAV was the same as at baseline, and the PEEP and the inflation time during back up ventilation were the same as at baseline. Whenever cessation of spontaneous breathing occurred for more than 5 s during PAV, mandatory backup inflations were automatically delivered by the ventilator. The backup rate set at 40 breaths per minute was delivered to the infant for 10 s with a backup inflation peak pressure of 5 cm H2O above the PIP used during ACV. Elastic unloading, which was used only during inspiration, was initially set at 75 % of full unloading. Full unloading was the level of unloading which increased the infant’s compliance to the expected ‘normal’, that is, 2.0 mL/cm H2O/kg. If after 10 min the infant remained stable and no airway pressure waveform abnormalities were observed [4], the unloading was increased to 100 %. If airway pressure waveform abnormalities were then noted by looking at the pressure display, the unloading was to be reduced back to 75 %. Resistive unloading was not used as, an in vitro model, oscillations in the airway pressure waveforms appeared when the resistive unloading was greater than 100 cm H2O/L/s [4].
The number of desaturations (an oxygen saturation less than 88 %) on each mode was noted. An arterial blood sample was obtained at the end of each 4-h period, the ventilatory settings were noted and the oxygenation index (OI) was calculated. Respiratory rate, tidal volume and mean airway pressure were obtained from the ventilator. The results from the last 5 min of the 4-h study period were averaged. All the infants had continuous oxygen saturation monitoring. During the study, the inspired oxygen concentration was adjusted as necessary to maintain the oxygen saturation level in the range 92–96 %.
Sample size
In our previous study, the mean OI in the PAV group was 6.0 (SD ± 2.4) and in the ACV group was 9.8 (SD ± 3.7) [1]. The planned sample size was 18 infants to allow detection between the two ventilator modes of a within patient difference of 0.7 SD in the oxygenation index results with 80 % power and a two-sided significance of 5 %.
Analysis
Differences were assessed for statistical significance using the paired Wilcoxon signed rank test using IBM SPPS statistical software, V.21 (IBM Corporation, USA).
Results
Recruitment to the trial was stopped at eight infants as all the OI results were in favour of PAV (Table 1). The decision was taken by the clinical team and the study statistician in the knowledge that the probability of all 8/8 results in the same direction (hence favouring PAV) if both modes were in fact equally effective was extremely small (0.58 = 0.0039).
The median birth weight of the infants was 767 (range 650–1926) g, gestational age 25.7 (range 24.4–33.5) weeks and postnatal age at measurement 19 (range 10–105) days; seven of the eight infants were male. All the infants had been exposed to antenatal steroids, received postnatal surfactant and were receiving caffeine at the time of study. None were receiving sedation at the time of study or had received postnatal steroids. Their median baseline compliance was 0.4 (range 0.3–1.1) mL/cmH2O and resistance was 155 (range 66–252) cmH2O/L/s. All infants tolerated 100 % elastic unloading throughout the study. The median FiO2 (p = 0.049), the median mean airway pressure (p = 0.012) and the median oxygenation index (p = 0.012) were all lower on PAV compared to ACV (Table 2). There was no significant difference in the median number of desaturation episodes between the two modes.
Discussion
We have demonstrated that PAV compared to ACV in prematurely born infants ventilated beyond the first week after birth resulted in superior oxygenation index results. Those results are in keeping with those of Schulze et al. [7] who compared PAV to SIMV or ACV in infants with evolving BPD. The 22 infants had a median gestational age of 25.6 weeks and were studied at a mean postnatal age of 22.9 days. They found after a 4-h period of PAV that despite a lower MAP, the inspired oxygen concentration and pulse oximetry readings were not significantly different between the two groups. All the infants in our study had arterial blood gas measurements, and hence, we were able to calculate their oxygenation index. We compared PAV to ACV as both modes provide respiratory support for all the infant’s breaths. During SIMV, only a preset number of the infant’s breaths are supported by the ventilator and hence this might at least partially explain why PAV was superior to SIMV/ACV in the earlier study [7]. We have previously demonstrated that during PAV [1], the inspiratory tidal volume and inflation pressures are closely phase-matched and the oesophageal pressure is out of phase as a result of the proportionality. This does not occur in ACV and likely leads to more efficient support during PAV. We did not record whether compliance was improved on PAV compared to ACV, but in our previous paper [1] demonstrated there was an almost significant (p = 0.05) reduction in thoraco-abdominal asynchrony which could improve oxygenation. In our previous study [1], the respiratory rate was significantly lower during PAV, but the medians were 54 bpm on PAV and 57 bpm on ACV, so unlikely to be of clinical significance. In this study, we did not demonstrate any significant differences in the respiratory rates or delivered tidal volumes. PAV compared to ACV support was not associated with any significant reduction in PaCO2 but the mean airway pressure was significantly lower during PAV, suggesting the PIP was lower and hence that PAV might have resulted in greater CO2 clearance.
In a previous 4-h cross-over study [7], although the incidence of arterial oxygen desaturations was not significantly different, the desaturations lasted longer when infants were supported by PAV. In that study, however, the infants had a history of frequent apnoeas and arterial oxygen desaturations. None of the infants in this study had been ventilated because of a history of apnoea. In addition, in the previous study [7], a time of 10 s was used during which the ventilator software identified cessation of breathing, whereas we used an updated version of the Stephanie software in which a 5-s period was used during which the ventilator software identified the cessation of breathing. It is likely then that this updated version enabled better support during PAV when the infant was apnoeic. We did not demonstrate any significant difference in the number of desaturations; indeed, the infants in both groups experienced very few desaturations.
Our study was terminated before our calculated sample size. We were mindful that all 12 infants in our 1-h cross-over study had lower OI results on PAV compared to ACV [1]. Hence, we wished to stop this study as early as possible if all the PAV results were again superior to the ACV results.
In our previous study [1], we also reported that on PAV, the median pressure time product level was significantly lower than on ACV indicating a lower work of breathing, which may reflect more synchronised support by the ventilator throughout inspiration. Neurally adjusted ventilatory assist (NAVA) also applies airway pressure throughout inspiration. During NAVA, the pressure applied is proportional to the electrical activity of the diaphragm. In a cross-over study of 14 preterm infants [3], asynchrony was significantly lower during 12 h on NAVA than during 12 h on pressure regulated, volume controlled ventilation. In addition, amongst ten infants recovering from severe acute respiratory distress syndrome, oxygenation was superior after 8 h of NAVA compared to after 8 h of pressure support ventilation (PSV) [5]. These data [1, 3, 5] and the results currently reported suggest ventilation modes which apply airway pressure in proportion to the infant’s respiratory effort throughout inspiration may be superior to those modes in which synchronisation is only at the start of inspiration (ACV) or the start and end of inspiration (pressure support ventilation).
Conclusion
In conclusion, we have demonstrated in a short-term cross-over study, PAV compared to ACV was associated with significantly superior oxygenation which likely reflects the better synchronisation of the inflation pressure and tidal volume throughout inspiration. We, therefore, feel these data emphasise the need now for a randomised controlled trial.
Abbreviations
- ACV:
-
Assist control ventilation
- BPD:
-
Bronchopulmonary dysplasia
- FiO2:
-
Fraction of inspired oxygen concentration
- MAP:
-
Mean airway pressure
- OI:
-
Oxygenation index
- PAV:
-
Proportional assist ventilation
- PCV:
-
Patient controlled ventilation
- PEEP:
-
Positive end expiratory pressure
- PIP:
-
Peak inspiratory pressure
- SIMV:
-
Synchronised intermittent mandatory ventilation
References
Bhat P, Patel DS, Hannam S, Rafferty GF, Peacock JL, Milner AD et al (2015) Crossover study of proportional assist versus assist control ventilation. Arch Dis Child Fetal Neonatal Ed 100:F35–F38
Hird M, Greenough A, Gamsu HR (1990) Gas trapping during high frequency positive pressure ventilation using conventional ventilators. Early Hum Dev 22:51–56
Longhini F, Ferrero F, De Luca D, Cosi G, Alemani M, Colombo D et al (2015) Neurally adjusted ventilatory assist in preterm neonates with acute respiratory failure. Neonatology 107:60–67
Patel DS, Rafferty GF, Hannam S, Lee S, Milner AD, Greenough A (2010) In vitro assessment of proportional assist ventilation. Arch Dis Child Fetal Neonatal Ed 95:F331–F337
Piastra M, De Luca D, Costa R, Pizza A, De Sanctis R, Marzano L et al (2014) Neurally adjusted ventilatory assist vs pressure support ventilation in infants recovering from severe acute respiratory distress syndrome: nested study. J Crit Care 312:e1–e5
Schulze A (2002) Respiratory mechanical unloading and proportional assist ventilation in infants. Acta Paediatr Suppl 437:19–22
Schulze A, Rieger-Fackeldey E, Gerhardt T, Claure N, Everett R, Bancalari E (2007) Randomized crossover comparison of proportional assist ventilation and patient-triggered ventilation in extremely low birth weight infants with evolving chronic lung disease. Neonatology 92:1–7
Acknowledgements
AG, ADM and PB designed the study. SS undertook all the assessments. JLP advised on the analysis. All authors were involved in the production of the manuscript.
Funding
PB was supported by the Charles Wolfson Charitable Trust. The research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. AG is an NIHR Senior Investigator.
Competing interests
AG has held grants from various ventilator manufacturers; AG and ADM have received honoraria for giving lectures and advising various ventilator manufacturers.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Patrick Van Reempts
Rights and permissions
About this article
Cite this article
Shetty, S., Bhat, P., Hickey, A. et al. Proportional assist versus assist control ventilation in premature infants. Eur J Pediatr 175, 57–61 (2016). https://doi.org/10.1007/s00431-015-2595-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-015-2595-4