Abstract
In-utero transfusion is now well under control and improves the survival of foetuses monitored for fetal anemia with a survival rate of more than 80 %. The aim was to evaluate short-term neonatal outcome after fetal severe anemia managed by intrauterine transfusions. We did a retrospective study of all neonates born after management of severe fetal anemia (n = 93) between January 1999 and January 2013 in our regional center. The two main causes of anemia were maternal red blood cell alloimmunization (N = 81, 87 %) and Parvovirus B19 infection (N = 10, 10.8 %). In the alloimmunization group, phototherapy was implemented in 85.2 % of cases with a maximum level of bilirubin of 114.4 ± 60.7 (mg/dl). Transfusion and exchange transfusion were, respectively, required in 51.9 % and in 34.6 % of cases. One neonate presented a convulsive episode, and we observed three neonatal deaths. In the parvovirus group, none of the child had anemia at birth and no management was necessary.
Conclusion: Contemporary management of Rhesus disease is associated with encouraging neonatal outcomes. In case of Parvovirus infection, no specific management is necessary at. But, in all cases of fetal anemia, children should be followed up with particular attention to neurologic development.
What is Known: • In-utero transfusion is now well under control and improves the survival of fetuses monitored for fetal anemia. • Limited studies are available on the effect of IUT on postnatal outcome in infants with a history of fetal anemia. |
What is New: • Contemporary management of severe Rhesus disease is associated with encouraging neonatal outcomes. • The majority of infants can be managed with phototherapy and a limited number of top-up transfusions and exchange transfusions. In case of Parvovirus infection, the short-term neonatal outcome is excellent. |
Similar content being viewed by others
Abbreviations
- CMV:
-
Cytomegalovirus
- ET:
-
Exchange transfusion
- GA:
-
Gestational age
- IUT:
-
Intrauterine transfusion
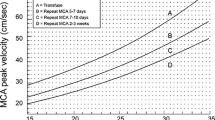
- MCA PSV:
-
MIddle cerebral artery peak systolic velocity
- MRI:
-
Magnetic resonance imaging
- NDI:
-
Neurodevelopmental impairment
- PT:
-
Phototherapy
- Rh:
-
Rhesus
References
al-Alaiyan S, al Omran A (1999) Late hyporegenerative anemia in neonates with rhesus hemolytic disease. J Perinat Med 27(2):112–115
Alcock GS, Liley H (2002) Immunoglobulin infusion for isoimmune haemolytic jaundice in neonates. Cochrane Database Syst Rev 3, CD003313
Branger B, Winer N (2006) Epidemiology of anti-D allo-immunization during pregnancy. J Gynécol Obstét Biol Reprod 35(1 Suppl):1S87–81S92
Carbonne B, Nguyen A, Cynober E, Castaigne V, Cortey A, Brossard Y (2008) Prenatal diagnosis of anoxic cerebral lesions caused by profound fetal anemia secondary to maternal red blood cell alloimmunization. Obstet Gynecol 112:442–444
De Boer IP, Zeestraten ECM, Lopriore E, van Kamp IL, Kanhai HHH, Walther FJ (2008) Pediatric outcome in rhesus hemolytic disease treated with and without intrauterine transfusion. Am J Obstet Gynecol 198(1):54–e1–4
De Jong EP, Lindenburg IT, van Klink JM, Oepkes D, van Kamp IL, Walther FJ et al (2012) Intrauterine transfusion for parvovsirus B19 infection: long-term neurodevelopmental outcome. Am J Obstet Gynecol 206(3):204–e1–5
Ebbesen F (1979) Late anaemia in infants with rhesus haemolytic disease treated with intensive phototherapy. Eur J Pediatr 130(4):285–290
Farrant B, Battin M, Roberts A (2001) Outcome of infants receiving in-utero transfusions for haemolytic disease. N Z Med J 114(1139):400–403
Garabedian C, Philippe M, Vaast P, Wibaut B, Salleron J, Delsalle A et al (2014) Is intrauterine exchange transfusion a safe procedure for management of fetal anaemia? Eur J Obstet Gynecol Reprod Biol 179:83–87
Jackson JC (1997) Adverse events associated with exchange transfusion in healthy and ill newborns. Pediatrics 99(5):E7
Klumper FJ, van Kamp IL, Vandenbussche FP, Meerman RH, Oepkes D, Scherjon SA et al (2000) Benefits and risks of fetal red-cell transfusion after 32 weeks gestation. Eur J Obstet Gynecol Reprod Biol 92(1):91–96
Lindenburg IT, Smits-Wintjens VE, van Klink JM, Verduin E, van Kamp IL, Walther FJ et al (2012) Long-term neurodevelopmental outcome after intrauterine transfusion for hemolytic disease of the fetus/newborn: the LOTUS study. Am J Obstet Gynecol 206(2):141.e1–141.e8
Mari G, Deter RL, Carpenter RL, Rahman F, Zimmerman R, Moise KJ Jr et al (2000) Noninvasive diagnosis by Doppler ultrasonography of fetal anemia due to maternal red-cell alloimmunization. Collaborative group for doppler assessment of the blood velocity in anemic fetuses. N Engl J Med 342(1):9–14
McGlone L, Simpson JH, Scott-Lang C, Cameron AD, Brennand J (2011) Short-term outcomes following intrauterine transfusion in Scotland. Arch Dis Child Fetal Neonatal Ed 96(1):F69–F70
Moise KJ Jr, Argoti PS (2012) Management and prevention of red cell alloimmunization in pregnancy: a systematic review. Obstet Gynecol 120(5):1132–1139
Nagel HTC, de Haan TR, Vandenbussche FPHA, Oepkes D, Walther FJ (2007) Long-term outcome after fetal transfusion for hydrops associated with parvovirus B19 infection. Obstet Gynecol 109(1):42–47
Patra K, Storfer-Isser A, Siner B, Moore J, Hack M (2004) Adverse events associated with neonatal exchange transfusion in the 1990s. J Pediatr 144(5):626–631
Saigal S, Doyle LW (2008) An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 371(9608):261–269
Schumacher B, Moise KJ Jr (1996) Fetal transfusion for red blood cell alloimmunization in pregnancy. Obstet Gynecol 88(1):137–150
Trevett TN, Dorman K, Lamvu G, Moise KJ (2005) Antenatal maternal administration of phenobarbital for the prevention of exchange transfusion in neonates with hemolytic disease of the fetus and newborn. Am J Obstet Gynecol 192(2):478–482
Van Kamp IL, Klumper FJCM, Oepkes D, Meerman RH, Scherjon SA, Vandenbussche FPHA et al (2005) Complications of intrauterine intravascular transfusion for fetal anemia due to maternal red-cell alloimmunization. Am J Obstet Gynecol 192(1):171–177
Weisz B, Rosenbaum O, Chayen B, Peltz R, Feldman B, Lipitz S (2009) Outcome of severely anaemic fetuses treated by intrauterine transfusions. Arch Dis Child Fetal Neonatal Ed 94(3):F201–F204
Compliance with Ethical Standards
Conflict of interest
All authors declare that they have no competing interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval was granted by the French Ethics Committee of research in Obstetrics and Gynecology (CEROG OBS 2012-02-04).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author’s contributions
C. Garabedian collected, analysed datas, and wrote the paper. T. Rakza, D. Thomas, P. Vaast, D. Subtil, B. Wibaut, and V. Debarge are all IUT operators and supervised and corrected this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Patrick Van Reempts
Rights and permissions
About this article
Cite this article
Garabedian, C., Rakza, T., Thomas, D. et al. Neonatal outcome after fetal anemia managed by intrauterine transfusion. Eur J Pediatr 174, 1535–1539 (2015). https://doi.org/10.1007/s00431-015-2573-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-015-2573-x