Abstract
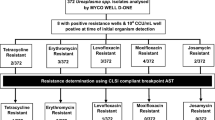
The focus on urogenital mycoplasmas as the possible etiologic agents of urogenital infections and syndromes, has increased in the last decade. Of these, Mycoplasma genitalium is proven to be pathogenic and sexually transmitted. We compared five commercially available assays for the detection of these organisms in urogenital mycoplasma culture specimen remnants. Stored specimen remnants were tested on Aptima Mycoplasma genitalium, Allplex™ STI Essential and CGMT, ResitancePlus®MG and Allplex™ MG & AziR Assays. All positive M. genitalium specimens and culture negative, nucleic acid positive Ureaplasmas were sent to the National Microbiology Laboratory for confirmation. The Aptima Mycoplasma genitalium assay detected 7 M. genitalium infections, the Allplex™ STI-EA and the Allplex™ CGMT detected 6 M. genitalium positives, and the Allplex™MG and AziR and SpeeDx ResistancePlus® MG detected 5 M. genitalium positives, four with macrolide resistant genes. The Allplex™ STI Essential assay was 100% sensitive and specific for Mycoplasma hominis and Ureaplasma targets. As seen in other studies, the Aptima Mycoplasma genitalium assay was 100% sensitive and specific for the detection of M. genitalium. The multiplex assays had lower sensitivities for M. genitalium detection (Allplex™ STI Essential and CGMT sensitivity of 85.71%; Allplex™ MG & AziR and SpeeDx ResistancePlus® MG sensitivity of 71.43%) with high specificities of 100%. Assays tested have high sensitivities and specificities for the detection of urogenital mycoplasmas especially M. genitalium macrolide resistance markers. All labs wanting to perform onsite detection of these organisms will find an assay to easily fit into their workflow.
Similar content being viewed by others
Data availability
The anonymized data is available and can be provided upon request.
References
Taylor-Robinson D, Jensen JS (2011) Mycoplasma genitalium: from Chrysalis to multicolored butterfly. Clin Microbiol Rev 24(3):498–514
Manhart LE, Broad JM, Golden MR (2011) Mycoplasma genitalium: should we treat and how? Clin Infect Dis 53(Suppl 3):S129–S142
Lis R, Rowhani-Rahbar A, Manhart LE (2015) Mycoplasma genitalium infection and female reproductive tract disease: a meta-analysis. Clin Infect Dis 61(3):418–426
Sasaki Y, Honda M, Makino M, Sasaki T (1993) Mycoplasmas stimulate replication of human immunodeficiency virus type 1 through selective activation of CD4+ T lymphocytes. AIDS Res Hum Retroviruses 9(8):775–780
Napierala MS, Weiss HA (2009) Association of Mycoplasma genitalium and HIV infection: a systematic review and meta-analysis. AIDS 23(5):611–620
Martin DH, Manhart LE, Workowski KA (2017) Mycoplasma genitalium from basic science to public health: summary of the results from a national institute of allergy and infectious diseases technical consultation and consensus recommendations for future research priorities. J Infect Dis 216(S2):S427–S430
Workowski KA, Bolan GA (2015) Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 64(3):1–136
Jensen JS, Cusini M, Gomberg M, Moi H (2016) European guideline on Mycoplasma genitalium. JEADV 30(10):1650–1656
The Australasian STI Management Guidelines. http://www.sti.guidelines.org.au/. Accessed March 12, 2020
Soni S, Horner P, Rayment M, Pinto-Sander N, Naous N, Parkhouse A, Bancroft D, Patterson C, Fifer H (2019) British association for sexual health and HIV national guideline for the management of infection with Mycoplasma genitalium (2018). Int J STD AIDS 30(10):938–950
Canadian Guidelines on Sexually Transmitted Infections—Management and treatment of specific infections—Mycoplasma genitalium Infections. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/sexually-transmitted-infections/canadian-guidelines-sexually-transmitted-infections-49.html. Accessed March 12, 2020
Horner P, Donders G, Cusini M, Gomberg M, Jensen JS, Unemo M (2018) Should we be testing for urogenital Mycoplasma hominis, Ureaplasma parvum and Ureaplasma urealyticum in men and women? A position statement from the European STI Guidelines Editorial Board. J Eur Acad Dermatol Venereol 32(11):1845–1851
Jensen JS (2012) Protocol for the detection of Mycoplasma genitalium by PCR from clinical specimens and subsequent detection of macrolide resistance-mediating mutations in region V of the 23S rRNA gene. Methods Mol Biol 903:129–139
Daxboeck F, Zitta S, Stadler S, Iro E, Krause R (2005) Mycoplasma hominis and Ureaplasma urealyticum in patients with sterile pyuria. J Infect 51:54–58
Chernesky M, Jang D, Martin I, Hoang LMN, Naidu P, Levett PN, Wylie J, Rebbapragada A, Ratnam S, Smieja M, Weinbaum B, Getman D, Canadian MG Study Group (2017) Mycoplasma genitalium antibiotic resistance-mediating mutations in Canadian women with or without Chlamydia trachomatis infection. Sex Transm Dis 44(7):433–435
Gratrix J, Plitt S, Turnbull L, Smyczek P, Brandley J, Scarrott P, Naidu P, Parker P, Blore B, Bull A, Shokoples S, Bertholet L, Martin I, Chernesky M, Read R, Singh A (2017) Prevalence and antibiotic resistance of Mycoplasma genitalium among STI clinic attendees in Western Canada: a cross-sectional analysis. BMJ Open (Online) 7:e016300. https://bmjopen.bmj.com/content/7/7/e016300.citation-tools. Accessed March 12, 2020
Unemo M, Salado-Rasmussen K, Hansen M, Olsen O, Falk M, Golparian D, Aasterød M, Ringlander J, Stezckó Nilsson C, Sundqvist M, Schønning K, Moi H, Westh H, Jensen JS (2018) Clinical and analytical evaluation of the new Aptima Mycoplasma genitalium assay, with data on M. genitalium prevalence and antimicrobial resistance in M. genitalium in Denmark, Norway and Sweden in 2016. Clin Microbiol Infect 24(5):533–539
Le Roy C, Pereyre S, Hénin N, Bébéar C (2017) French prospective clinical evaluation of the Aptima Mycoplasma genitalium CE-IVD assay and macrolide resistance detection using three distinct assays. J Clin Microbiol 55(11):3194–3200
Jensen JS, Bradshaw CS, Tabrizi SN, Fairley CK, Hamasuna R (2008) Azithromycin treatment failure in Mycoplasma genitalium positive patients with non-gonococcal urethritis is associated with induced macrolide resistance. Clin Infect Dis 47:1546–1553
Manhart LE (2014) Diagnostic and resistance testing for Mycoplasma genitalium: what will it take? Clin Infect Dis 59:31–33
Tagg KA, Jeoffreys NJ, Couldwell DL, Donald JA, Gilbert GL (2013) Fluoroquinolone and macrolide resistance-associated mutations in Mycoplasma genitalium. J Clin Microbiol 51:2245–2249
Nijhuis RH, Severs TT, Van der Vegt DS, Van Zwet AA, Kusters JG (2015) High levels of macrolide resistance-associated mutations in Mycoplasma genitalium warrant antibiotic susceptibility-guided treatment. J Antimicrob Chemother 70:2515–2518
Lau A, Bradshaw CS, Lewis D, Fairley CK, Chen MY, Kong FY, Hocking JS (2015) The efficacy of azithromycin for the treatment of genital Mycoplasma genitalium: a systematic review and meta-analysis. Clin Infect Dis 61:1389–1399
Walker J, Fairley CK, Bradshaw CS et al (2013) Mycoplasma genitalium incidence, organism load, and treatment failure in a cohort of young Australian women. Clin Infect Dis 56:1094–1100
Deguchi T, Yasuda M, Horie K et al (2015) Drug resistance-associated mutations in Mycoplasma genitalium in female sex workers. Japan Emerg Infect Dis 21:1062–1064
Salado-Rasmussen K, Jensen JS (2014) Mycoplasma genitalium testing pattern and macrolide resistance: a Danish nationwide retrospective survey. Clin Infect Dis 59:24–30
Chernesky M, Jang D, Martin I, Arias M, Shah A, Smieja M, Ratnam S, Getman D, Schachter J (2019) Mycoplasma genitalium, Chlamydia trachomatis, and Neisseria gonorrhoeae detected with Aptima Assays performed on self-obtained vaginal swabs and urine collected at home and in a clinic. Sex Transm Dis 46(9):e87-89
Taylor-Robinson D (2017) Mollicutes in vaginal microbiology: Mycoplasma hominis, Ureaplasma urealyticum, Ureaplasma parvum and Mycoplasma genitalium. Res Microbiol 168:875–881
Le Roy C, Hénin N, Bébéar C, Pereyre S (2017) Evaluation of a commercial multiplex quantitative PCR (qPCR) assay for simultaneous detection of Mycoplasma genitalium and macrolide resistance-associated mutations in clinical specimens. J Clin Microbiol 55(3):978–979
Tabrizi SN, Su J, Bradshaw CS, Fairley CK, Walker S, Tan LY, Mokany E, Garland SM (2017) Prospective evaluation of ResistancePlus MG, a new multiplex quantitative PCR assay for detection of Mycoplasma genitalium and macrolide resistance. J Clin Microbiol 55(6):1915–1919
Funding
This project had no external funding. The labor was provided in kind by the laboratories and test kits were provided by the manufacturers at no charge. Seegene Inc. provided the CFX96 as a loan for the duration of the study.
Author information
Authors and Affiliations
Contributions
PN conceived the study, developed the study methodology with NZ and SS, reviewed the study results and authored the manuscript together with AS. SS performed all the testing and collated the results. Irene Martin performed the confirmatory testing. All authors participated in the review and editing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Prenilla Naidu received honoraria for speaking engagements from Hologic® (2016) and Seegene Inc. (2019). The other authors have no conflicts of interest to declare.
Ethical approval
Ethics approval for the study was obtained from the Human Research Ethics Board at the University of Alberta. The authors confirm that this manuscript reports on results of their original research. This manuscript is not under consideration for publication by any other journal. A small portion of the data (the Seegene assay results) was presented at a workshop at the STI & HIV 2019 World Congress in Vancouver, Canada.
Consent to participate
Remnant specimens submitted for testing of the same organisms by culture were anonymized and used for this study. Consent to participate in this study was thus not required.
Consent for publication
All authors have approved this manuscript for submission for publication.
Additional information
Edited by Volkhard A. J. Kempf.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Naidu, P., Shokoples, S., Martin, I. et al. Evaluation of 5 commercial assays for the detection of Mycoplasma genitalium and other Urogenital Mycoplasmas. Med Microbiol Immunol 210, 73–80 (2021). https://doi.org/10.1007/s00430-021-00699-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-021-00699-1